Importance of Multifocal Intraocular Lenses in The Elderly Population
Article Information
Ibrahim Sahbaz*
Department of Ophthalmology, Üsküdar University Faculty of Medicine, Istanbul, Turkey
*Corresponding Author: Ibrahim Sahbaz, Department of Ophthalmology, Üsküdar University Faculty of Medicine, Istanbul, Turkey
Received: 16 March 2020; Accepted: 26 March 2020; Published: 31 March 2020
Citation: Ibrahim Sahbaz. Importance of Multifocal Intraocular Lenses in The Elderly Population. Journal of Ophthalmology and Research 3 (2020): 08-15.
Share at FacebookAbstract
Background: Vision rehabilitation in elderly populations.
Objective: We aimed to evaluate potential factors affecting the visual quality and other parameters in the selection of appropriate intraocular lenses in cataract surgery for patients with senile cataract. In addition, we evaluated the type of intraocular lenses optimal for cataract surgeries in elderly patients and attempted to analyze the significance of visual rehabilitation without glasses to improve the quality-of-life of elderly patients who are unable to use glasses.
Method: We retrospectively investigated the records of 49 eyes from 49 patients who underwent cataract surgery for senile cataract during 2014–2015. Preoperative and postoperative pupil sizes were measured using The Oasis brand of pupillometer, and changes in the pupil size were statistically analyzed. Distribution of variables was analyzed using the Kolmogorov–Smirnov test. The Wilcoxon test was used for repeated measurements. Study data was analyzed using the SPSS 22.0 program.
Results: Of all patients, 32 were males and 17 were females (age, 48–81 years). A significant decrease in the pupil size was postoperatively noted (p < 0.05). The mean preoperative pupil size decreased to 4.1 ± 0.9 mm from 4.9 ± 1.0 mm during the first postoperative month.
Conclusion: Cataract is usually related to aging. Multifocal intraocular lenses (MIOLs) are not or only slightly affected by the pupil size and enable the elderly to meet their daily needs without depending on glasses and, thus, improve their quality-of-life after cataract surgery. Thus, we recommend MIOLs that function independent of pupil size as appropriate for cataract surgeries in elderly patients.
Keywords
Intraocular lens; Dementia; Cataract; Pupil
Intraocular lens articles, Dementia articles, Cataract articles, Pupil articles
Article Details
Introduction
Cataract is a common eye disease that occurs among the elderly. The incidence of cataract increases with age. Age-related cataract is the most frequent cause of visual problems in the elderly. The prevalence of cataract is 50% in patients aged 65–74 years and 70% in those aged >75 years. The pathogenesis of age-related cataract is multifactorial and remains unclear [1]. Conventional monofocal intraocular lenses (IOLs) have a uniform but limited range of focus. The level of focusing of monofocal IOLs can be arranged for either far, intermediate, or near distances. However, it remains necessary to use corrective lenses to compensate for other distances. Therefore, multifocal (MIOLs) or accommodative IOLs have gained much attention in cataract surgery [2].
In recent years, cataract surgery has become an extremely precise and safe surgical procedure owing to the development of phacoemulsification technique and advanced IOL designs. Moreover, cataract surgery has gone beyond being a vision-correction operation and has instead become a refractive procedure that improves the quality-of-life of patients by eliminating the need for glasses. In fact, patients not only request to achieve correct visual acuity but also to achieve improved visual quality that eliminates the need for glasses for far, intermediate, and near distances after surgery.
Previous studies have reported that the pupil size affects the higher order aberrations and, thus, has a great impact on the visual quality [3-5]. It is also important in refractive procedures, including refractive surgery, multifocal lens implantation, and multifocal contact lenses [6]. In this study, we evaluated the pupil size and associated visual acuity before and after phacoemulsification in elderly patients with senile cataract.
Currently, the average life expectancy has increased owing to advancements in medicine and socio-economic developments, which have triggered a rapid increase in the elderly population. Extended lifetime brings an elevation in age-related diseases. According to the data of the Turkish Statistical Institute (TURKSTAT), the average life expectancy (total, male, and female, respectively) in the Turkish society was 73.9, 71.6, and 76.3 years in 2010. These figures are projected to increase to 75.4, 72.7, and 78.3 years by 2020. Currently, the number of individuals aged ≥85 years is 488.568 in Turkey. It is expected that the elderly population will constitute 9.8% of the total Turkish population in 2025, equaling 8.253.000 individuals [7].
Because of age-related changes in the organs, some organ functions may decelerate or completely deteriorate. Alzheimer-type dementia and mild cognitive impairment disrupt the daily quality-of-life of patients [8, 9]. Dementia, which is handled by geriatric psychiatry, is noted in elderly patients and has been reported to adversely affect an individual’s quality of life. It mostly influences the intellectual performance, memory, and personality of affected individuals [10]. The prevalence of dementia increases with aging and can reach 20%–40% among patients aged >85 years. The most common cause of dementia is the Alzheimer’s disease, which accounts for 50%–60% of all dementia cases [11]. Furthermore, falling accidents are frequently noted among the elderly patients because of their decreased physical and mental abilities related to aging. An investigation into the relationship between health problems and falling incidents has revealed that only visual impairment (refractive error) and cataract are associated with falling incidents [12]. Orthopedic, neurological, psychiatric, and other types of diseases related to aging impair an elderly patient’s ability to perform daily life activities, leaving them in the need of nursing. Changes in the nervous system due to aging reduce the learning ability, memory, and data processing of patients. Besides age-related neurodegenerative diseases, there has also been a serious increase in the incidence of stroke [13]. Dementia severely affects the memory, leading to difficulties, or even failures, in using simple objects such as glasses and comb. Executive dysfunction causes the impairment of abstraction, planning, reasoning, and mental flexibility. Individuals cannot find appropriate solutions to these issues that they face during their daily life activities [14]. Parkinson’s disease, which leads to motor disorders, is another disease that has become common among the elderly. Because of age-related health problems, including those mentioned above, the use of glasses (far or near) is almost impossible and that of optical instruments becomes highly complicated at older ages. Degenerative joint diseases also obstruct the use of separate glasses for near and far distances because such diseases decrease the ability of the elderly to properly use their hands. A previous study has indicated that the prevalence of osteoarthritis increases with age, with a prevalence of >80% in patients aged ≥65 years [15].
Material & Methods
We retrospectively investigated the records of 49 eyes from a total of 49 patients (32 males and 17 females; age range: 48–81 years) diagnosed with senile cataract for which they underwent cataract surgery (Table 1). The study protocol was approved by the University of Health Sciences, Haydarpaşa Numune Training and Research Hospital Ethics Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki. Routine preoperative ophthalmological examinations of the patients were carried out.
|
Median (Min–Max) |
Avg ± SD/n (%) |
|||
|
Age, years |
66.0 (48.0–81.0) |
65.4 ± 7.7 |
||
|
Sex |
Women Men |
17 32 |
34.7% 65.3% |
|
|
Side |
Right Left |
36 39 |
48.0% 52.0% |
|
Table 1:
The exclusion criteria in this study included previous eye trauma, optical neuropathy, and a history of uveitis, congenital eye abnormality, and similar disorders. Only those cases that were undertaken by the same surgeon were considered. Patients who experienced surgical complication(s) were also excluded.
For patients included in the analysis, the preoperative and postoperative pupil sizes were measured using The Oasis brand of pupillometer. Changes in the pupil size were statistically analyzed. All procedures were performed by the same surgeon under topical anesthesia. Phacoemulsification was performed through a clear cornea incision created using a 3-mm keratome. A viscoelastic material was used to fill the anterior chamber. For all patients, capsulorhexis was performed, followed by hydrodissection. After the removal of nucleus using the phaco-tip, the cortex was aspirated. A balanced salt solution (BBS; 500 mL) was used as the infusion solution for phacoemulsification, irrigation, and aspiration. Subsequently, the lens capsule was inflated with the viscoelastic material, after which IOL was placed into the capsular bag. The viscoelastic material was then carefully aspirated. The operation was completed with the inflation of incisions. The same type of IOL (AcrySof® IQ Monofocal IOLSN60WF) was used for all patients. Postoperative medications including antibiotics (0.5% moxifloxacin ophthalmic solution), steroids (0.1% dexamethasone), and anti-inflammatory drugs (0.3% nepafenac) were administered at the same dose for 4 weeks. The pupil size was measured prior to operation and at the first postoperative month. Patients were seated in a dark room for 5 min before the measurement. In similar studies, the postoperative pupil size was generally measured at the end of the 6th week after operation [16]. A photometer was used to control the light intensity in the room, and each patient was waited at a mild light level (4 cd/m2) for 5 min. The preoperative and postoperative measurements were performed by the same medical team. The pupil diameter was measured thrice for each patient, and measurements were averaged and recorded for the analysis. Descriptive statistics used included median, standard deviation, median, min–max, percentage, and frequency. The distribution of variables was analyzed using the Kolmogorov–Smirnov test. The Wilcoxon signed-rank test was used for repeated measurements. Study data were analyzed using the SPSS 22.0 program.
Results
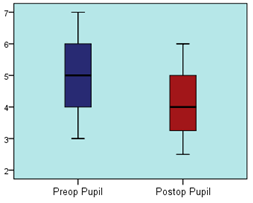
The preoperative pupil size ranged from 3 mm to 7 mm among the patients (median, 5 mm; average, 4.9 ± 1.0 mm), whereas the postoperative pupil size ranged from 2.5 mm to 6 mm (median, 4 mm; average, 4.1 ± 0.9 mm). There was a significant decrease in the postoperative pupil size compared with the preoperative size (p = 0.05) (Table 2). The mean decrease in the postoperative pupil size was 0.8 mm during the first postoperative month. Thus, the postoperative pupil size showed a significant decrease (p < 0.05) than the preoperative pupil size (Table 2).
|
Median (Min–Max) |
Avg ± SD |
p |
|||
|
Pupil size, mm |
Preoperative Postoperative |
5.0 4.0 |
3.0–7.0 2.5–6.0 |
4.9 ± 1.0 4.1 ± 0.9 |
0.000 |
|
Wilcoxon test |
|||||
Table 2:
Discussion
Monofocal IOLs are the commonly preferred IOLs after cataract surgery. Patients receiving standard monofocal IOLs, which offer clear vision at a single distance, often require glasses for mid-range and near distance vision. Furthermore, some patients may also need glasses for far distance vision. The most significant factor for the use of monofocal IOLs is their low cost. However, currently, there are various IOL types, including MIOLs, that provide clear vision after cataract surgery without the need for glasses. In fact, Accommodative IOLs and MIOLs were developed to eliminate the need for glasses.
MIOLs are of two types: diffractive and refractive. Diffractive MIOLs are designed in line with the Huygens–Fresnel principle and comprise concentric prisms placed in the front and back of the lens. Light bundles passing through prisms are split between the near and far distances, ensuring a focus at these distances. As a result, a patient fitted with these lenses can see both far and near distances without glasses. Refractive IOLs have spherical anterior and posterior surfaces, which cover the regions of anomeric aspherical adhesion. With light refractions at ranging levels in certain parts, IOLs achieve clarity and near and far vision. Complaints such as decreased clarity, contrast sensitivity, reflection, and halo may arise because of the overlapping of images created by different refractory parts of the retina. In contrast, postoperative visual defects are closely associated with the pupil size [17]. One of the most important shortcomings of MIOLs is that they divide the light energy between multiple images, which leads to decreased contrast sensitivity. In addition, halos are the inevitable adverse effects of MIOLs. These are defined as light reflections or blurred rings, which are particularly significant at night [18]. Thus, the bigger the pupil size, the greater are the visual disturbances related to the pupil size at night. Nevertheless, a smaller pupil size negatively affects the near and mid-range visual acuity.
The influence of pupil size varies across different IOLs. A previous study has reported that phacoemulsification temporarily reduces the pupil size, but the pupil reverts to its original form after some time [19]. In another study, the mean difference between the preoperative and postoperative pupil sizes was <0.5 mm and the pupil diameter showed a ≥0.8-mm change in 10% of patients [20]. In contrast, the mean decrease in the pupil size was 0.8 mm in the first postoperative month in our study. Donnenfeld et al. has reported similar results and stated that the mean preoperative pupil size after dark adaptation was 5.36 mm, which became 4.85 mm within 30–60 d after the operation [21]. We believe that the absence of lens support after operation plays a significant role in the decrease in the pupil size. Another factor influencing the pupil size is age. A study on pupil measurements of 222 subjects aged 65–89 years found a significant decrease in the pupil size under both dark and bright environments and indicated that the pupil diameter decreases with age [22]. The main problems associated with the pupil size are visual impairments, including contrast sensitivity, halo, glare, and decrease in the depth of focus. Moreover, a decreased pupil size adversely affects the visual acuity at near and mid-range distances. Some IOLs that are dependent on the pupil size, such as AMO ReZomm and Alcon ReStor; some that are independent of the pupil size, such as Amo Tecnis; and accommodating IOLs, such as Eyeonics Crystalens, are still in use (2). Recently, trifocal lenses—the new generation diffractive lenses—such as AT LISA tri (Carl Zeiss Meditec and FineVision, PhysIOL) have come into use. Alcon released the PanOptix trifocal version, which is the third version of trifocal lenses. Unlike classic diffractive lenses, trifocal IOLs do not cause the loss of a portion of light energy (18%–20%). The diffractive pattern is further modified in some lenses to control the refraction of different wavelengths of light; this process is called the chromatic aberration correction. An example of such a lens is the Tecnis Symfony (Abbott Medical Optics). Diffractive multifocality combined with an extended range of vision, achieved in the Symfony by chromatic aberration control and asphericity changes, and optical performance of the lens depending on the pupil control together helps modern MIOLs to become much more flexible in terms of near and, particularly, intermediate vision performance. These lenses also produce a significant increase in contrast sensitivity, which was lost in the earlier designs of lenses partially because of the dispersion of light created by the diffractive pattern. These changes lead to better visual outcomes with modern MIOLs [23]. Better visual outcomes can be achieved after considering the pupil size. Near, mid-range, and far visual acuity gain higher importance at older ages. The use of glasses or contact lenses has become almost impossible for elderly patients because of their orthopedic, neurological, psychiatric, and other diseases related to aging.
In conclusion, currently, cataract surgery can be successfully performed using advanced instruments and devices. The ability of elderly patients to sustain their quality of life and maintain their visual needs without depending on glasses is closely associated with the characteristics of the IOL placed in their eye as well as the success of cataract surgery. IOLs widely vary in terms of their material and technological characteristics. The pupil size is extremely important in the selection of correct MIOLs in elderly patients. The pupil size decreases with age, and the pupil diameter decreases after cataract surgery. Therefore, we believe that the purpose of a cataract surgery should be to ensure visual rehabilitation in elderly patients, unless there is a contraindication, and that selecting an MIOL that is not or only slightly influenced by the pupil size is important in patients with senile cataract.
Conflict of Interest
There is no conflict of interest. No financial support was received for this study.
References
- Pelit A. Aydın P. Oküler yaşlanma. Geriatri 4 (2001): 28-32.
- İzzet CA. Surgical treatment of presbyopia and multifocal intraocular lenses: Transitioning from cataract to refractive intraocular lens surgery. Glokom-Katarakt 2 (2007).
- Petermeier K, Frank C, Gekeler F, et al. Influence of the pupil size on visual quality and spherical aberration after implantation of the Tecnis 1-piece intraocular lens. British journal of ophthalmology 95 (2011): 42-45.
- Fernandez de Castro LE, Sandoval HP, Bartholomew LR, et al. High-order aberrations and preoperative associated factors. Acta Ophthalmologica Scandinavica 85 (2007): 106-110.
- McKelvie J, McArdle B, McGhee C. The influence of tilt, decentration, and pupil size on the higher-order aberration profile of aspheric intraocular lenses. Ophthalmology 118 (2011): 1724-1731.
- Erkılıç K, Tuzcu EA, Özkırış A, et al. Effect of pupillary size on ocular aberrations. Abant Med J 3 (2014): 134-137.
- (http://www.tuik.gov.tr ; 08.07.2010).
- Perry RJ, Hodges JR. Attention and executive deficits in Alzheimer's disease: A critical review. Brain 122 (1999): 383-404.
- Arnáiz E, Almkvist O. Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease. Acta Neurologica Scandinavica 107 (2003): 34-41.
- WA Lishman. Organic Psychiatry. Blackwell Scientific Publications, Oxford (1987).
- Ineichen B. Measuring the rising tide: how many dementia cases will there be by 2001?. The British Journal of Psychiatry 150 (1987): 193-200.
- Tunçay SU, Özdinçler AR, Erdinçler DS. Geriatrik hastalarda düşme risk faktörlerinin günlük yaşam aktiviteleri ve yaşam kalitesine etkisi. Turkish Journal of Geriatrics 14 (2011): 245-252.
- Gurvit H, Bilgic B. Nöroloji Temel Kitabı 2. Baskı (2013): P. 938
- Gurvit İ. H. Demans Sendromu, Alzheimer Hastalıǧı ve Alzheimer Dışı Demanslar. İstanbul Tıp Fakültesi Nöroloji Kitabı (2011), p443.
- Karaaslan Y. Osteoartrit, MD Yayıncılık, Ankara (2000).
- Felson DT, Radin EL. What causes knee osteoarthrosis: are different compartments susceptible to different risk factors?. The Journal of rheumatology 21 (1994): 181-183.
- Eason J, Seward HC. Pupil size and reactivity following hydroxypropyl methylcellulose and sodium hyaluronate. British journal of ophthalmology 79 (1995): 541-543.
- Mesci C, Karakurt Y, Aydın N, et al. Comparison of visual functions with diffractive (Restor) and refractive (Rezoom) multifocal intraocular lenses after cataract operations. Glo-Kat 4 (2009): 183-188.
- Aslan BS, Akyol N. Multifocal intraocular lenses for cataract surgery and neuroadaptation. Glokom-Katarakt 3 (2008).
- Hayashi K, Hayashi H. Pupil size before and after phacoemulsification in nondiabetic and diabetic patients. Journal of Cataract & Refractive Surgery 30 (2004): 2543-2550.
- Koch DD, Samuelson SW, Villarreal R, et al. Changes in pupil size induced by phacoemulsification and posterior chamber lens implantation: consequences for multifocal lenses. Journal of Cataract & Refractive Surgery 22 (1996): 579-584.
- Donnenfeld E, Gupta A, Morris M, et al. The effect of cataract surgery on the pupil light response, presented at XXXI. Congress of the European Society of Cataract and Refractive Surgeons in 5-9 October 2013
- Birren JE, Casperson RC, Botwinick J. Age changes in pupil size. Journal of Gerontology 5 (1950): 216-221.
