Impact of Psychological Stress during COVID 19 Pandemic on Quality of Life of Health Care Workers in Mental Health Hospital in Egypt
Article Information
Zeinab Mohamed El Nagar1*, Marwa Abdel Meguid Hammed1,, Yasmine Mahmoud Massoud2, Heba Adel Hassan1, Mohamed Youssef Mohamed1, Ola Mohamad Aufa1
1Psychiatric institute, Faculty of Medicine, Ain Shams University, Cairo, Egypt and psychological medicine hospital , Cairo, Egypt
2Tropical department, Faculty of Medicine, Ain Shams University, Cairo, Egypt
*Corresponding Author: Zeinab Mohamed Ahmed El Nagar, Lecturer of Psychiatry, Department of Psychiatry, Faculty of Medicine, Ain Shams University, No. 38 Abbaseya st., Dar El Malak, Postal code 1187, Cairo, Egypt
Received: 28 May 2022; Accepted: 08 June 2022; Published: 15 June 2022
Citation: Zeinab Mohamed El Nagar, Marwa Abdel Meguid Hammed, Yasmine Mahmoud Massoud, Heba Adel Hassan, Mohamed Youssef Mohamed, Ola Mohamad Aufa. Impact of Psychological Stress during COVID 19 Pandemic on Quality of Life of Health Care Workers in Mental Health Hospital in Egypt. Journal of Psychiatry and Psychiatric Disorders 6 (2022): 178-195.
Share at FacebookAbstract
Background: COVID-19 outbreak resulted in negative mental health consequences such as depression, anxiety, and stress, particularly among health-care workers. Objective: To evaluate health care worker mental well-being and explore the reasons standing beyond their concerns and fears.
Methods: From January to June 2021, we recruited 107 health care workers from psychiatric hospitals. The translated Arabic version COVID stress scale was used to assess their level of stress. The WHO Quality of Life - BREF score was used to assess their level of affection for their quality of life.
Results: The majority of our sample (45.8%) was between the ages of 20 and 30. Females made up 37.8% of the group. The majority of them were infected during the first wave. The COVID Stress Scale (CSS) revealed that 21.5% of participants had no signs or symptoms of depression, while 55.1% had mild symptoms. Only 23.4% of our sample had moderate to severe symptoms. When categorised by domains, the mean CSS score was 12.21 ± 5.62 for danger subscale, 6.18 ± 4.07 for socioeconomic subscale, 8.44 ± 4.58 for xenophobia subscale, 7.99 ± 4.18 for contamination subscale, 5.87 ± 4.32 for traumatic subscale, and 11.13 ± 6.15 for compulsive subscale. The mean scores for the WHO QOL-brief score for physical aspect were 91.51 ± 21.5, 75.25 ± 12.84 for psychological aspect, 40.42 ± 8.52 for social aspect, and 96.26 ± 17.76 for environmental aspect.
Conclusion: we discovered that health-care workers experienced high levels of stress, particularly during and after COVID -19 pandemic waves.
Keywords
COVID-19; CSS; WHO-QOL; Health care; Mental health hospital; Stress; Egypt
COVID-19 articles; CSS articles; WHO-QOL articles; Health care articles; Mental health hospital articles; Stress articles; Egypt articles.
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals COVID Stress Scale articles COVID Stress Scale Research articles COVID Stress Scale review articles COVID Stress Scale PubMed articles COVID Stress Scale PubMed Central articles COVID Stress Scale 2023 articles COVID Stress Scale 2024 articles COVID Stress Scale Scopus articles COVID Stress Scale impact factor journals COVID Stress Scale Scopus journals COVID Stress Scale PubMed journals COVID Stress Scale medical journals COVID Stress Scale free journals COVID Stress Scale best journals COVID Stress Scale top journals COVID Stress Scale free medical journals COVID Stress Scale famous journals COVID Stress Scale Google Scholar indexed journals WHO-QOL articles WHO-QOL Research articles WHO-QOL review articles WHO-QOL PubMed articles WHO-QOL PubMed Central articles WHO-QOL 2023 articles WHO-QOL 2024 articles WHO-QOL Scopus articles WHO-QOL impact factor journals WHO-QOL Scopus journals WHO-QOL PubMed journals WHO-QOL medical journals WHO-QOL free journals WHO-QOL best journals WHO-QOL top journals WHO-QOL free medical journals WHO-QOL famous journals WHO-QOL Google Scholar indexed journals Health care articles Health care Research articles Health care review articles Health care PubMed articles Health care PubMed Central articles Health care 2023 articles Health care 2024 articles Health care Scopus articles Health care impact factor journals Health care Scopus journals Health care PubMed journals Health care medical journals Health care free journals Health care best journals Health care top journals Health care free medical journals Health care famous journals Health care Google Scholar indexed journals Mental health hospital articles Mental health hospital Research articles Mental health hospital review articles Mental health hospital PubMed articles Mental health hospital PubMed Central articles Mental health hospital 2023 articles Mental health hospital 2024 articles Mental health hospital Scopus articles Mental health hospital impact factor journals Mental health hospital Scopus journals Mental health hospital PubMed journals Mental health hospital medical journals Mental health hospital free journals Mental health hospital best journals Mental health hospital top journals Mental health hospital free medical journals Mental health hospital famous journals Mental health hospital Google Scholar indexed journals Stress articles Stress Research articles Stress review articles Stress PubMed articles Stress PubMed Central articles Stress 2023 articles Stress 2024 articles Stress Scopus articles Stress impact factor journals Stress Scopus journals Stress PubMed journals Stress medical journals Stress free journals Stress best journals Stress top journals Stress free medical journals Stress famous journals Stress Google Scholar indexed journals Egypt articles Egypt Research articles Egypt review articles Egypt PubMed articles Egypt PubMed Central articles Egypt 2023 articles Egypt 2024 articles Egypt Scopus articles Egypt impact factor journals Egypt Scopus journals Egypt PubMed journals Egypt medical journals Egypt free journals Egypt best journals Egypt top journals Egypt free medical journals Egypt famous journals Egypt Google Scholar indexed journals Post Traumatic Stress Disorder; articles Post Traumatic Stress Disorder; Research articles Post Traumatic Stress Disorder; review articles Post Traumatic Stress Disorder; PubMed articles Post Traumatic Stress Disorder; PubMed Central articles Post Traumatic Stress Disorder; 2023 articles Post Traumatic Stress Disorder; 2024 articles Post Traumatic Stress Disorder; Scopus articles Post Traumatic Stress Disorder; impact factor journals Post Traumatic Stress Disorder; Scopus journals Post Traumatic Stress Disorder; PubMed journals Post Traumatic Stress Disorder; medical journals Post Traumatic Stress Disorder; free journals Post Traumatic Stress Disorder; best journals Post Traumatic Stress Disorder; top journals Post Traumatic Stress Disorder; free medical journals Post Traumatic Stress Disorder; famous journals Post Traumatic Stress Disorder; Google Scholar indexed journals Quality of life- Brief score articles Quality of life- Brief score Research articles Quality of life- Brief score review articles Quality of life- Brief score PubMed articles Quality of life- Brief score PubMed Central articles Quality of life- Brief score 2023 articles Quality of life- Brief score 2024 articles Quality of life- Brief score Scopus articles Quality of life- Brief score impact factor journals Quality of life- Brief score Scopus journals Quality of life- Brief score PubMed journals Quality of life- Brief score medical journals Quality of life- Brief score free journals Quality of life- Brief score best journals Quality of life- Brief score top journals Quality of life- Brief score free medical journals Quality of life- Brief score famous journals Quality of life- Brief score Google Scholar indexed journals Statistical Package for Social Sciences articles Statistical Package for Social Sciences Research articles Statistical Package for Social Sciences review articles Statistical Package for Social Sciences PubMed articles Statistical Package for Social Sciences PubMed Central articles Statistical Package for Social Sciences 2023 articles Statistical Package for Social Sciences 2024 articles Statistical Package for Social Sciences Scopus articles Statistical Package for Social Sciences impact factor journals Statistical Package for Social Sciences Scopus journals Statistical Package for Social Sciences PubMed journals Statistical Package for Social Sciences medical journals Statistical Package for Social Sciences free journals Statistical Package for Social Sciences best journals Statistical Package for Social Sciences top journals Statistical Package for Social Sciences free medical journals Statistical Package for Social Sciences famous journals Statistical Package for Social Sciences Google Scholar indexed journals
Article Details
Abbreviations:
Covid-19: Coronavirus 2019; CSS: Covid Stress Scale; HCWs: Healthcare Workers; PPE: Personal Protective Equipment; Pro-Qol: Professional Quality of life score; PTSD: Post Traumatic Stress Disorder; Qol: Quality of life; Sars-Cov2: Sever acute respiratory syndrome Corona Virus; SPSS: Statistical Package for Social Sciences; WHO: World Health Organization; WHO-Qol: World Health Organization- Quality of life- Brief score.
1. Introduction
The outbreak of a new coronavirus disease (COVID-19, formerly known as nCoV-2019) was first reported in Wuhan, China since late December 2019 [1]. It is an acute fatal disease with progressive fatal respiratory complications that end up with death [2]. In April 2020, there were more than 1 million cases of infected patients all over 60 countries around the world. Wu et al. found that mortality rate reached 2.3% after analysis of 72,314 cases. In addition, 14% of patients were reported to have serious complications and 5% of the patients were critical [2]. Being a newly discovered pandemic, its clinical presentation, epidemiological features, the pattern of transmission, implication on the public health and the preparation of the health facilities to face it were still unclear. That is why this pandemic represented a fear that threatens the psychological health of people; not only healthy people but also at-risk individuals especially the health care workers. These problems range from fear and anxiety to severe depression and burnout [3]. This sense of fear and anxiety was present among healthcare workers (HCW) working not only in hospitals, inpatient and outpatient care, large tertiary care centres, and all isolation units specifically, those HCW who are in direct contact with confirmed and suspected cases. They are prone to both infection risk and mental health problems [4]. With more progression, the need for health care resources increases which may not be compatible with that emergency situation as there is not enough manpower. This in turn puts the health care workers under pressure as they are afraid of being infected. They began to experience fear, sleep disturbance, anxiety and depressive symptoms and emotional disturbance. Despite that, there was not enough services providing counselling and screening for anxiety, depression and suicidal attempts for physicians during that era [5]. It is expected that health care workers; not only doctors but also paramedics as ambulance workers; are liable to depression, anxiety, burnout syndrome and post-traumatic stress disorder (PTSD) after cessation of that pandemic. Many socioeconomic and psychological factors were reported to be associated with the development of stress, anxiety and depression [6]. The relative deficiency of knowledge in addition to misunderstanding about any new discovered virus among the HCW leads to the rapid spread of infection worldwide which in turn put patients’ own lives at risk (Hoffman and Silverberg, 2018). That is why gaining more knowledge about how to deal with the virus greatly affects their attitude towards the new virus. According to their knowledge, many HCW have already modified their attitude or suspended their work to uncertain time [7].
Mental health care workers as other health care workers are prone to the same stressors in addition to other stressors unique to their profession. One of these factors is the multidisciplinary approach required sometimes to treat certain patients. In addition, poor work environment and those patients who commit suicide are considered a source of stress that can lead mental HCWs to PTSD. All of these perspectives make the mental HCWs prone to face a poor quality of life and more stress during pandemics [8]. In 2020, Thakur and Jain performed an international cross-sectional study among 41 countries including UK, USA and China to identify the factors associated with development of post pandemics psychological disturbances. They found that among 2527 HCWs, lack of personal protective equipment (PPE), mental health support availability and presence of t raining raising their awareness about the pandemic before deployment were the most common factors associated with depression and anxiety found among HCWs [9]. The World Health Organization (WHO) declared that managing HCW mental health and psychosocial wellbeing during this time is as important as managing their physical health to face the COVID-19 pandemic [10]. To our knowledge, there was a scarce of data concerning the mental health of HCW in Egypt, so we tried to evaluate HCW mental well-being and explore the reasons standing beyond their concerns and fears.
2. Material and Methods
We interviewed 107 participants who are working in mental health hospital from January 2021 to June 2021 and agree to participate in the study. Participants included (psychiatrist, internal medicine doctors, psychologist, nurses, service workers, security and administrate employee). The purpose of the study was offered to all participants before being enrolled. An interview was made with each participant by an experienced psychiatrist. Each participant was offered 2 scales; CSS (the COVID stress scale) and the WHO QOL – brief (the World health organization quality of life brief) [11]. A pilot study was conducted on the validity and reliability of CSS scale, with sample included 106 of participants who were randomly selected from society. The CSS will be re distributed to the same 106 participants after two weeks to assess the validity coefficient and also the confidence coefficient compared to the impact event scale (gold standard) [12].
2.1. The COVID Stress scale (CSS)
It includes 36 items which was developed during the era of COVID – 19 for identifying people who need mental health services. These 36 items were categorized into 5 domains; Danger and contamination fears, fears about economic consequences, xenophobia, compulsive checking and reassurance seeking and traumatic stress symptoms about COVID-19 [13]. Arabic version was used after translation and backtranslation to English was done to ensure accuracy of version used this step was conducted via 35 bilingual experts from psychologist and psychiatric university staff. Experts’ recommendations were done to adapt our culture and language [12].
2.2. The Arabic version of World health organization quality of life brief scale (WHO-QOL BREF) [14]
It includes 26 items 24 of which cover 4 QOL domains the first domain; physical health includes 7 items, the second one; psychological health; includes 4 items. The third one; Social relationships; includes 3 items. The fourth one; environment; includes 8 items. Ethical approval was obtained from the ethical committee of Ain Shams University. Participants had the right to stop at any time of the study. Data were collected anonymously then coded and analysed.
2.3. Statistical analysis
We used statistical package for social sciences (SPSS) version 20 for windows for data analysis. Quantitative data was described in terms of mean and standard deviation if normally distributed. Kolmogrov-Semornov test was used for assessment of normality of distribution of numerical variables. Chi-square test was used for testing the association between categorical variables. Independent sample t test was used for testing the difference of a numerical variable between 2 groups. P value less than 0.05 was considered statistically significant.The proportion of stress problems in HCW during COVID-19 pandemic was reviewed by Maryam Vizheh et al. in 2020 [15] and reported in a systematic review with widely varied prevalence. A sample size of at least 104 produces a two-sided 95% confidence interval with a width equal to 0.199 when the sample proportion is 0.50.Sample size calculation: We used G power 3.0.01 for windows for calculating the sample size required and found that with power of 95%, α error of 5% and p value 0.5, effect size =0.2 the minimum required sample size for analysis was 104 participants.
3. Results
The study was conducted on a wide age group ranging from 20 to 60 years. Their mean age was 31.86 ± 5.42 years old. Most of them (47.7%, 51 participants) were between 30 and 45 years old. While only 7 participants (6.5%) were between 45 and 60 years old.73.8% of them (79 participants) were females. Most participants (99 participants, 92.5%) were living in urban areas.
Most participants (64.5%, 69 participants) were Single. 35 participants (32.7% of participants) were Married. Only 3 participants (2.8%) were divorced. On reviewing their educational status, we found that 52 participants (48.6% of them) were Postgraduates; 54 participants (50.5%) were still students. only One participant (0.9%) was still among secondary school students. We found that there were 51 participants (47.7%) injured during the 1st wave along with 35 participants (32.7%) injured during the 2nd wave. On the other hand, only 21 participants (19.6%) were recorded during the 3rd wave. On reviewing their job, we found that 52.3% of participants (56 participants) were of medical personnel as shown in Table 1.
|
Socio-Demographic data |
No |
|
Age (years) |
|
|
20-30 years |
49 (45.8) |
|
30-45 years |
51 (47.7) |
|
45-59 years |
7 (6.5) |
|
Gender |
|
|
Female |
79 (73.8) |
|
Male |
28 (26.2) |
|
Marital status |
|
|
Single |
69 (64.5) |
|
Married |
35 (32.7) |
|
Divorced |
3 (2.8) |
|
Level of education |
|
|
Post graduated |
52 (48.6) |
|
University |
54 (50.5) |
|
School (till secondary) |
1 (0.9) |
|
COVID Wave |
|
|
1st |
51 (47.7) |
|
2nd |
35 (32.7) |
|
3rd |
21 (19.6) |
|
Job |
|
|
Medical |
56 (52.3) |
|
Administrative |
21 (19.6) |
|
Security |
15 (14) |
|
Service |
15 (14) |
|
Current Address |
|
|
Urban |
99 (92.5) |
|
Rural |
8 (7.5) |
Table 1: illustrates the sociodemographic characteristics of the included participants (n=107).
COVID Stress Scale (CSS) was administrated to all participants and found that 55.1% of participants suffering from mild stress while 23.4% of them (25 participants) were suffering from moderate stress. On the other hand, 21.5% of participants (23 patients) did not suffer any stress according to CSS as shown in Table 2.
|
COVID Stress Scale |
Frequency |
|
Absent |
23 (21.5) |
|
Mild |
59 (55.1) |
|
Moderate |
25 (23.4) |
|
Total |
107 |
Table 2: illustrates the CSS scores among all participants (n=107).
We found that mean score for COVID stress scale for participants was 51.81 ± 20.83. for domains; the mean was 12.21 ± 5.62 for danger subscale, 6.18 ± 4.07 for socioeconomic subscale, 8.44 ± 4.58 for xenophobia, 7.99 ± 4.18 for contamination, 5.87 ± 4.32 for traumatic and 11.13 ± 6.15 for compulsive fears. For WHO quality of life (WHO-QOL) score, we found that mean scores for the physical domain was 91.51 ± 21.5, for psychological domain was 75.25 ± 12.84, for social domain was 40.42 ± 8.52 and for environmental status was 96.26 ± 17.76 as shown in Table 3.
|
Domain |
Mean ± SD |
|
COVID stress scale (CSS) |
|
|
Danger |
12.21 ± 5.62 |
|
Socioeconomic |
6.18 ± 4.07 |
|
Xenophobia |
8.44 ± 4.58 |
|
Contamination |
7.99 ± 4.18 |
|
Traumatic |
5.87 ± 4.32 |
|
Compulsive |
11.13 ± 6.15 |
|
Total score |
51.81 ± 20.83 |
|
WHO quality of life scale (WHO-QOL) |
|
|
Physical |
91.51 ± 21.5 |
|
Psychological |
75.25 ± 12.84 |
|
Social |
40.42 ± 8.52 |
|
Environmental |
96.26 ± 17.76 |
Table 3: illustrates the score for CSS and WHO-QOL sub scales among all participants (n=107).
When studying the association between CSS and the sociodemographic characteristics we found that there was no significant difference between age groups concerning the domains of CSS. The fear of danger domain was slightly higher among younger group compared to the other groups, but this was statistically insignificant (p=0.275). for the socioeconomic fears, the score was higher among older group compared to the others and this was also insignificant (p=0.366) as shown in Table 4. Xenophobia and fear of contamination scores were higher among older group compared to the others. However, this was insignificant (p=0.251, p=0.755). Traumatic fear and compulsive disorders were insignificantly more common among younger patients (p=0.583, p=0.644) respectively as shown in Table 4. The gender difference showed no significant association with CSS scores in most domains although males had slightly higher scores concerning socioeconomic fears, fear of contamination, traumatic fears, compulsive disorders compared to females’ group (p=0.163, p=0.989, p=0.253, p=0.663) respectively. On the other hand, we found that xenophobia scores were significantly higher among males compared to females (0.046) as shown in Table 4.
Concerning marital status, we found that divorced participants had high danger fearing scores compared to other groups (p=0.289). for xenophobia, divorced patients had less scores compared to other group (p=0.88). however, married participants had higher fear of contamination compared to the others (p=0.949) as shown in Table 4. For the level of education, school students had higher scores of fears compared to the others. However, this was statistically insignificant (p=0.205). on the other hand, they had the lowest scores concerning xenophobia and compulsive disorders fears. And this was also insignificant (p=0.773, p=0.548) as shown in Table 4. For residence, no significant difference between patients living in urban and rural areas concerning all aspects of CSS (p=0.729, p=0.23, p=0.102, p=0.732, p=0.617, p=0.513) respectively as shown in Table 4.
|
Variable |
COVID stress scale (CSS) |
|||||
|
Danger |
Socio-economic |
Xenophobia |
Contamination |
Traumatic |
Compulsive |
|
|
Age 20 – 30 30 – 45 45 – 60 |
13.16 ± 5.73 11.39 ± 5.64 11.43 ± 4.65 |
5.57 ± 3.81 6.65 ± 4.48 7 ± 2.58 |
8.04 ± 4.59 8.45 ± 4.6 11.14 ± 4.49 |
7.8 ± 4.72 8.04 ± 3.9 9 ± 2.16 |
6.35 ± 4.19 5.47 ± 4.53 5.43 ± 4.28 |
11.73 ± 6.66 10.57 ± 5.87 11 ± 5.1 |
|
P value |
0.275 |
0.366 |
0.251 |
0.775 |
0.583 |
0.644 |
|
Gender Male Female |
11.18 ± 5.22 12.57 ± 5.78 |
7.11 ± 4.82 5.85 ± 3.78 |
9.93 ± 4.88 4.41 ± 3.91 |
8 ± 4 7.99 ± 4.29 |
6.68 ± 4.73 5.58 ± 4.19 |
11.57 ± 5.99 10.97 ± 6.27 |
|
P value |
0.265 |
0.163 |
0.046 |
0.989 |
0.253 |
0.663 |
|
Marital status Single Married Divorced |
11.68 ± 5.73 12.91 ± 5.45 16 ± 5.57 |
6.23 ± 4.42 6.17 ± 3.58 5 ± 1 |
8.3 ± 4.63 8.71 ± 4.71 8.33 ± 4.16 |
7.91 ± 4.14 8.17 ± 4.52 7.67 ± 1.53 |
5.38 ± 4.32 6.6 ± 4.2 8.67 ± 6.03 |
11.36 ± 6.02 10.63 ± 6.59 11.67 ± 6.43 |
|
P value |
0.289 |
0.880 |
0.913 |
0.949 |
0.211 |
0.842 |
|
Level of education Postgraduate University School |
12.33 ± 5.5 11.91 ± 5.73 22 |
5.92 ± 3.87 6.43 ± 4.35 6 |
8.75 ± 4.76 8.17 ± 4.52 7 |
7.87 ± 4.12 8.11 ± 4.35 8 |
5.54 ± 4.12 6.15 ± 4.59 8 |
10.63 ± 5.98 11.69 ± 6.4 7 |
|
P value |
0.205 |
0.821 |
0.773 |
0.956 |
0.686 |
0.548 |
|
COVID wave 1st 2nd 3rd |
13.98 ± 6.7 10.6 ± 3.26 11.48 ± 4.71 |
5.39 ± 4.12 5.71 ± 3.1 8.86 ± 4.51 |
6.49 ± 4.1 9.11 ± 4 12.05 ± 4.36 |
8.47 ± 4.97 6.4 ± 3.1 9.48 ± 2.82 |
5.43 ± 4.25 6.26 ± 4.75 6.29 ± 3.94 |
10.69 ± 7.52 11.91 ± 4.41 10.9 ± 5.11 |
|
P value |
0.005 |
0.003 |
<0.001 |
0.014 |
0.613 |
0.656 |
|
Job Administrative Security Medical Service |
9.48 ± 2.8 12.8 ± 5.85 11.14 ± 4.92 19.4 ± 5.42 |
7.67 ± 4.62 7.67 ± 2.77 4.75 ± 4.11 7.93 ± 2.25 |
9.57 ± 4.21 12.47 ± 3.44 7.71 ± 4.75 5.53 ± 2.07 |
8.1 ± 2.9 9.07 ± 1.98 6.21 ± 3.93 13.4 ± 3.38 |
2.76 ± 2.95 6.6 ± 4.29 5.25 ± 3.77 11.8 ± 1.37 |
9.57 ± 2.5 12.07 ± 5.4 9.04 ± 5.59 20.2 ± 4.21 |
|
P value |
<0.001 |
0.002 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
Residence Urban Rural |
12.15 ± 5.69 12.88 ± 5.46 |
6.31 ± 4.13 4.5 ± 3.25 |
8.65 ± 4.58 5.88 ± 4.42 |
8.03 ± 4.18 7.5 ± 4.72 |
5.93 ± 4.39 5.13 ± 3.87 |
11.24 ± 6.19 9.75 ± 6.27 |
|
P value |
0.729 |
0.23 |
0.102 |
0.733 |
0.617 |
0.513 |
Table 4: illustrates the association between CSS and socio demographic characteristics among included participants (n=107).
On reviewing the quality of life of the health care workers, we found that the psychological and social subscales were significantly different among age groups (p=0.029, p=0.003). we found that higher age group participants (45 – 60) years old had a higher QOL compared to other groups whether psychologically and socially as shown in the Table 5 below. For gender distribution, we found that both males and females had nearly equal QOL scores whether physically, psychologically, socially and environmentally (p=0.668, p=0.987, p=0.788, p=0.725) respectively, as shown in the Table 5 below. For the marital status, we found that both single and married participants showed a high QOL compared to divorced ones concerning all aspects of QOL score. However, this was statistically insignificant (p=0.881, p=0.892, p=0.965, p=0.727) respectively, as shown in the Table 5 below. Despite those graduates and student showed a higher QOL compared to others in school as shown in the table below, but this was statistically insignificant for all aspects of QOL (p=0.166, p=0.497, p=0.145, p=0.120) respectively, as shown in the Table 5 below. On the other hand, we found that the type of COVID wave was a significant predictor for determining the QOL whether physically, socially and environmentally especially those who became infected in the 3rd wave (p=0.005, p=0.005, p<0.001) respectively. However, on the psychological level, we found that the difference was not statistically significant (p=0.064), as shown in the Table 5 below. We found that the residence was not a significant indicator for predicting the quality of life of HCWs whether physically, psychologically, socially and environmentally (p=0.089, p=0.692, p=0.577, p=0.455) respectively, as shown in the Table 5 below.
|
Domain |
WHO-QOL BREEF |
|||
|
Physical |
Psychological |
Social |
Environmental |
|
|
Age 20 – 30 30 – 45 45 – 60 |
86.37 ± 22.58 95.14 ± 19.88 101.14 ± 20.88 |
72.16 ± 12.19 77.02 ± 12.75 84 ± 14.24 |
37.71 ± 8 41.96 ± 8.52 47.43 ± 5.38 |
92.33 ± 18.31 98.51 ± 18.45 100 ± 18.04 |
|
P value |
0.059 |
0.029 |
0.003 |
0.204 |
|
Gender Male Female |
90 ± 19.31 92.05 ± 22.45 |
75.29 ± 13.47 75.24 ± 12.78 |
40 ± 8.98 40.51 ± 8.41 |
94.71 ± 17.72 96.15 ± 18.82 |
|
P value |
0.668 |
0.987 |
0.788 |
0.725 |
|
Marital status Single Married Divorced |
91.59 ± 19.8 91.89 ± 24.97 85.33 ± 27.23 |
74.84 ± 13.89 76.11 ± 11.52 74.67 ± 9.24 |
40.23 ± 8.11 40.69 ± 9.13 40 ± 13.86 |
94.96 ± 17.13 97.71 ± 21.13 92 ± 20 |
|
P value |
0.881 |
0.892 |
0.965 |
0.727 |
|
Level of education Postgraduate University School |
94.77 ± 21.7 88.89 ± 21.18 64 |
76.38 ± 12.68 74.37 ± 13.18 64 |
40.85 ± 8.69 40.22 ± 8.2 24 |
98.92 ± 19 93.19 ± 17.54 72 |
|
P value |
0.166 |
0.497 |
0.145 |
0.120 |
|
COVID wave 1st 2nd 3rd |
84.71 ± 25.96 96.11 ± 16.53 100.38 ± 9.29 |
72.94 ± 12.41 75.31 ± 15.63 80.76 ± 6.02 |
38.04 ± 8.7 41.03 ± 8.86 44.95 ± 5.04 |
88.78 ± 19.47 102.06 ± 16.19 102.29 ± 13.3 |
|
P value |
0.005 |
0.064 |
0.005 |
<0.001 |
|
Job Administrative Security Medical Service |
101.14 ± 14.92 102.13 ± 12.45 92.36 ± 20.56 64.27 ± 18.48 |
80.95 ± 14.02 81.87 ± 7.84 71.64 ± 13.8 74.13 ± 4.5 |
42.86 ± 8.5 44.8 ± 5.89 39.57 ± 8.88 35.47 ± 6.57 |
105.52 ± 14.56 97.07 ± 12.69 95.21 ± 17.78 82.93 ± 23.54 |
|
P value |
<0.001 |
0.005 |
0.009 |
0.003 |
|
Residence Urban Rural |
90.51 ± 21.51 104 ± 19.94 |
75.11 ± 13.19 77 ± 9.01 |
40.24 ± 8.66 42 ± 6.67 |
95.39 ± 18.86 100.5 ± 12.55 |
|
P value |
0.089 |
0.692 |
0.577 |
0.455 |
Table 5: illustrates the relation between WHO QOL domains and sociodemographic characteristics among selected participants (n=107).
3.1. Reliability
In sample repeatability (test-retest reliability) of the COVID stress and quality of life in health care worker: The scale was tested for repeatability over 61 individuals during a period of 15 days, utilizing a scale testing as illustrated in table 6.
|
COVID stress and quality of life in health care worker |
Force Means ± Std. Dev. |
F-test |
p-value |
ICC (95% C.I.) |
|
Q1 |
1.72±0.90 |
18.30 |
<0.001** |
0.896 (0.833-0.937) |
|
Q2 |
2.44±1.10 |
35.52 |
<0.001** |
0.945 (0.910-0.967) |
|
Q3 |
2.74±1.12 |
14.16 |
<0.001** |
0.868 (0.789-0.919) |
|
Q4 |
2.16±1.16 |
16.86 |
<0.001** |
0.888 (0.820-0.931) |
|
Q5 |
1.61±1.07 |
21.85 |
<0.001** |
0.912 (0.858-0.947) |
|
Q6 |
1.52±1.09 |
16.80 |
<0.001** |
0.888 (0.820-0.931) |
|
Total Danger Subscale |
12.20±4.96 |
31.79 |
<0.001** |
0.939 (0.900-0.963) |
|
Q7 |
0.67±0.85 |
172.27 |
<0.001** |
0.988 (0.981-0.993) |
|
Q8 |
0.67±0.83 |
81.89 |
<0.001** |
0.976 (0.960-0.985) |
|
Q9 |
0.97±1.09 |
46.96 |
<0.001** |
0.958 (0.931-0.975) |
|
Q10 |
1.61±1.00 |
120.11 |
<0.001** |
0.983 (0.973-0.990) |
|
Q11 |
0.69±0.89 |
93.16 |
<0.001** |
0.979 (0.965-0.987) |
|
Q12 |
1.69±1.03 |
62.08 |
<0.001** |
0.968 (0.948-0.981) |
|
Total Socio-economic Subscale |
6.30±4.65 |
323.67 |
<0.001** |
0.994 (0.990-0.996) |
|
Q13 |
1.39±1.10 |
13.69 |
<0.001** |
0.864 (0.783-0.916) |
|
Q14 |
1.05±1.11 |
12.46 |
<0.001** |
0.851 (0.764-0.908) |
|
Q15 |
1.28±0.99 |
7.96 |
<0.001** |
0.777 (0.654-0.860) |
|
Q16 |
1.33±1.14 |
18.36 |
<0.001** |
0.897 (0.834-0.937) |
|
Q17 |
1.41±1.10 |
8.72 |
<0.001** |
0.794 (0.679-0.871) |
|
Q18 |
1.50±1.16 |
13.14 |
<0.001** |
0.859 (0.775-0.913) |
|
Total Xenophobia Subscale |
7.96±5.25 |
10.66 |
<0.001** |
0.828 (0.729-0.893) |
|
Q19 |
1.48±1.07 |
18.78 |
<0.001** |
0.899 (0.837-0.938) |
|
Q20 |
1.92±1.05 |
7.32 |
<0.001** |
0.760 (0.629-0.849) |
|
Q21 |
1.48±0.96 |
11.27 |
<0.001** |
0.837 (0.742-0.899) |
|
Q22 |
1.10±0.99 |
16.28 |
<0.001** |
0.884 (0.814-0.929) |
|
Q23 |
1.02±1.00 |
33.06 |
<0.001** |
0.941 (0.904-0.964) |
|
Q24 |
0.78±1.00 |
25.94 |
<0.001** |
0.926 (0.879-0.955) |
|
Total Contamination Subscale |
7.77±5.04 |
18.57 |
<0.001** |
0.898 (0.835-0.937) |
|
Q25 |
1.26±0.95 |
14.37 |
<0.001** |
0.870 (0.792-0.920) |
|
Q26 |
1.13±0.97 |
36.97 |
<0.001** |
0.947 (0.914-0.968) |
|
Q27 |
0.80±0.96 |
9.12 |
<0.001** |
0.802 (0.691-0.877) |
|
Q28 |
1.05±1.01 |
12.52 |
<0.001** |
0.852 (0.765-0.909) |
|
Q29 |
0.72±0.99 |
13.57 |
<0.001** |
0.863 (0.781-0.915) |
|
Q30 |
0.67±0.91 |
97.89 |
<0.001** |
0.980 (0.967-0.988) |
|
Total Traumatic Subscale |
5.64±4.79 |
19.82 |
<0.001** |
0.904 (0.845-0.941) |
|
Q31 |
1.87±1.23 |
21.74 |
<0.001** |
0.912 (0.858-0.946) |
|
Q32 |
1.97±1.06 |
14.10 |
<0.001** |
0.868 (0.789-0.918) |
|
Q33 |
1.03±1.12 |
29.37 |
<0.001** |
0.934 (0.893-0.960) |
|
Q34 |
1.57±1.28 |
12.19 |
<0.001** |
0.848 (0.759-0.906) |
|
Q35 |
1.11±0.98 |
7.95 |
<0.001** |
0.777 (0.653-0.860) |
|
Q36 |
1.33±1.01 |
5.47 |
<0.001** |
0.691 (0.533-0.802) |
|
Compulsive Checking Subscale |
8.89±4.92 |
11.47 |
<0.001** |
0.840 (0.746-0.901) |
|
Total Covid Stress Index 1st reading |
48.75±23.19 |
15.18 |
<0.001** |
0.876 (0.802-0.924) |
Table 6: Mean forces applied with standard deviations to achieve the COVID stress and quality of life in health care worker (n=61).
Throughout the testing COVID stress and quality of life in health care worker were applied to the samples. The interclass Correlation Coefficient (ICC) with absolute agreement and average measure was utilized to assess repeatability for the data. The ICC was 0.876, 95% C.I. (0.802-0.924), F=15.18, p < 0.001. The results indicated good repeatability of the scale as shown in Table 6.
3.2. Validity
The results of constructive validity: it shows the results of constructive validity through the correlation coefficient of each dimension with the total degree as shown in Table 7 and figure 1.
|
Items |
COVID stress and quality of life in health care worker |
|||
|
First Reading |
Second Reading |
|||
|
r |
p-value |
r |
p-value |
|
|
Q1 |
0.624 |
<0.001** |
0.622 |
<0.001** |
|
Q2 |
0.693 |
<0.001** |
0.69 |
<0.001** |
|
Q3 |
0.484 |
<0.001** |
0.484 |
<0.001** |
|
Q4 |
0.599 |
<0.001** |
0.597 |
<0.001** |
|
Q5 |
0.75 |
<0.001** |
0.751 |
<0.001** |
|
Q6 |
0.644 |
<0.001** |
0.64 |
<0.001** |
|
Total Danger Subscale |
0.819 |
<0.001** |
0.817 |
<0.001** |
|
Q7 |
0.586 |
<0.001** |
0.594 |
<0.001** |
|
Q8 |
0.593 |
<0.001** |
0.591 |
<0.001** |
|
Q9 |
0.666 |
<0.001** |
0.665 |
<0.001** |
|
Q10 |
0.578 |
<0.001** |
0.576 |
<0.001** |
|
Q11 |
0.438 |
<0.001** |
0.435 |
<0.001** |
|
Q12 |
0.559 |
<0.001** |
0.555 |
<0.001** |
|
Total Socioeconomic Subscale |
0.701 |
<0.001** |
0.699 |
<0.001** |
|
Q13 |
0.658 |
<0.001** |
0.654 |
<0.001** |
|
Q14 |
0.337 |
0.008* |
0.344 |
0.007* |
|
Q15 |
0.678 |
<0.001** |
0.677 |
<0.001** |
|
Q16 |
0.794 |
<0.001** |
0.797 |
<0.001** |
|
Q17 |
0.714 |
<0.001** |
0.7 |
<0.001** |
|
Q18 |
0.741 |
<0.001** |
0.737 |
<0.001** |
|
Total Xenophobia Subscale |
0.822 |
<0.001** |
0.819 |
<0.001** |
|
Q19 |
0.784 |
<0.001** |
0.786 |
<0.001** |
|
Q20 |
0.758 |
<0.001** |
0.758 |
<0.001** |
|
Q21 |
0.767 |
<0.001** |
0.768 |
<0.001** |
|
Q22 |
0.497 |
<0.001** |
0.498 |
<0.001** |
|
Q23 |
0.797 |
<0.001** |
0.792 |
<0.001** |
|
Q24 |
0.744 |
<0.001** |
0.751 |
<0.001** |
|
Total Contamination Subscale |
0.875 |
<0.001** |
0.876 |
<0.001** |
|
Q25 |
0.66 |
<0.001** |
0.659 |
<0.001** |
|
Q26 |
0.658 |
<0.001** |
0.658 |
<0.001** |
|
Q27 |
0.638 |
<0.001** |
0.641 |
<0.001** |
|
Q28 |
0.614 |
<0.001** |
0.616 |
<0.001** |
|
Q29 |
0.696 |
<0.001** |
0.699 |
<0.001** |
|
Q30 |
0.464 |
<0.001** |
0.467 |
<0.001** |
|
Total Traumatic Subscale |
0.754 |
<0.001** |
0.756 |
<0.001** |
|
Q31 |
0.568 |
<0.001** |
0.568 |
<0.001** |
|
Q32 |
0.561 |
<0.001** |
0.562 |
<0.001** |
|
Q33 |
0.5 |
<0.001** |
0.498 |
<0.001** |
|
Q34 |
0.454 |
<0.001** |
0.455 |
<0.001** |
|
Q35 |
0.597 |
<0.001** |
0.6 |
<0.001** |
|
Q36 |
0.51 |
<0.001** |
0.51 |
<0.001** |
|
Compulsive Checking Subscale |
0.721 |
<0.001** |
0.721 |
<0.001** |
|
r-Pearson Correlation Coefficient; *p-value <0.05 S; **p-value <0.001 HS |
||||
Table 7: Validity of Internal Consistency: For a measure of behaviors related to COVID stress and quality of life in health care worker (n=61).
It is evident from the previous table that the scale statements of (36) all of results a significant of (<0.001), which indicates a strong internal correlation and consistency in answering the questions of this scale, and this is greatly reflected in the degree of reliability of this scale as shown in Table 7. Statistical analysis of these results showed significant agreement between the two readings in the detection. Comparison of first reading and second reading a yielded weighted Kappa =0.642, it was level “substantial agreement”, with p-value <0.001 highly significant as shown in Table 7 and Figure 1.
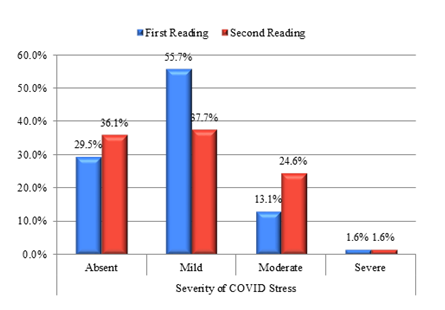
Figure 1: Kappa measure of agreement between the first reading and second reading in severity of COVID stress (n=61).
3.3. Validity
Discriminatory honesty means the comparison between the upper category “the highest quartile” (above 25% of the scores of the individuals with a high degree on the scale) of the sample members and the lower category “the lowest quartile” (less than 25% of the scores of the individuals with a low score on the scale) of the sample members on axes The questionnaire, the total scale, and table 8 illustrate this comparison.
|
Scales |
Groups |
No. |
Mean |
±SD |
t-test |
p-value |
|
Total score of COVID stress |
Lowest value |
11 |
62.09 |
16.15 |
10.517 |
<0.001** |
|
Highest value |
11 |
174.09 |
31.41 |
|||
|
Total score of Impact stress event |
Lowest value |
11 |
2.73 |
2.20 |
21.696 |
<0.001** |
|
Highest value |
11 |
29.73 |
3.50 |
Table 8: Shows the difference between the averages of the highest and lowest quartiles on the total scores of the two scales among the modified scale and the gold standard scale in total score of COVID stress (n=22 from total n=45).
It is clear from the previous table that all values of “t-value” are statistically significant at the level of 0.001, which indicates the discriminatory validity of the scale, and this confirms the validity of the scale for application, and indicates that the scale has one of the psychometric properties of a good measure, which is its ability to discriminate. Furthermore, it turns out that there is a strong correlation between the modified scale and the gold standard scale (r-value = 0.714 and p-value <0.001 highly significant correlation) (n=45) as shown in Figure 2. Statistical analysis of these results showed significant agreement between the two scales in the detection. Comparison of modified scale and gold standard scale a yielded weighted Kappa =0.602, it was level “substantial agreement”, with p-value <0.001 highly significant.
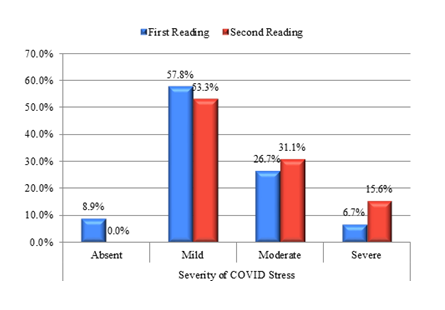
Figure 2: Kappa measure of agreement between the two scales among the modified scale and the gold standard scale in severity of COVID stress (n=45).
4. Discussion
Severe acute respiratory syndrome corona virus (SARS-COV2) or what is known as COVID 19 is a pandemic started from Wuhan since March 2019 and affected more than 200 million persons around the world. More than 4 million deaths have occurred around the world [16]. This in turn negatively affected the mental health of peoples especially the health care workers who are the first line defence for this spreading pandemic [17]. Psychological disturbances are one of the most common consequences for pandemics among HCWs like; anxiety, depression and post-traumatic stress disorders (PTSD) which were prevalent disorders in the previous outbreak of SARS in 2003 [18]. These symptoms remained for a long period up to one year [19]. In our study, 107 HCWs were recruited from mental health hospital. 26.2% of them were males. Half of them were psychiatrists and internal medicine doctors, nurses or other associated medical personnel. 14% were of the security team while 14% of participants were from services team. We measured their psychological health using COVID stress scale and WHO=QOL scores and found that stress was absent among 21.5% of participants, while positive in 78.5% of participants divided into 55.1% suffering from mild symptoms and 23.4% of them having moderate symptoms. In Mexico, Fernández et al., 2021 [20] performed a study among 912 nursing students and graduates and found that their average danger of contamination subscale was 39.34 ± 10.01 which was much higher than our results. Fair of socioeconomic consequences, xenophobia and traumatic stress scores were also higher (18.15 ± 6.24, 17.15 ± 6.35, 10.16) respectively compared to our findings. On the other hand, the mean compulsive checking was nearly equal between patients in both studies (12.89 ± 4.81 vs 11.13 ± 6.15). This may be explained by the high stress encountered by nursing staff as reported by Johannes et al., compared to other workers [21]. In our study, we found that males were more stressed concerning the pandemic in all subscales. However, this was insignificant except for xenophobia which was significantly evident among males compared to females (9.93 ± 4.88 vs 4.41 ± 3.91, p=0.04). This was in contrary to Fernández et al., who reported that females experienced more stress compared to males [20]. In our study, we found nearly half of the sample were infected through the first wave (47.7%, 51 participants) while 32.7% were infected in the second one. This was not the case among participants in Fernández et al., 2021 in which only 6.6% tested positive and 14.8% reported contact with suspected cases. This may be the reason for the difference in perceived stress and psychological disturbances due to difference in clinical experience dealing with the pandemic.
The quality of life is negatively affected during pandemics due to experienced anxiety, depression and lack of social support at these times. HCWs especially those on the frontline have poorer quality of life compared to others as they must deal with patients despite shortage of PPE and many other factors [22]. In our study, we used the WHO-QOL tool for assessment of the QOL of the health care workers. We found that the highest QOL scores were found in environmental status (96.26 ± 17.76) while the lowest scores were those for social domain which were 40.42 ± 8.51. Comparing these results to what has been approved in non-pandemic settings among the general population, we found that the psychological QOL for our population was nearly similar to that of the general population which was 70.6 ± 14 despite the presence of external stressors affecting their mental health [23]. In Malaysia, the QOL of health care workers working in university hospitals were assessed using WHOQOL and found that they have poorer physical and environmental quality of life compared to our population. Their mean scores were 74.06 ± 15.32 & 75.48 ± 14.65 respectively. However, their scores regarding psychological QOL were comparable to ours. On the other hand, their social QOL scores were higher compared to our findings (70.87 ± 19.67) [24]. This may be explained by the difference in health care systems and socioeconomic characteristics between the two populations. In Italy, Buselli et al. studied the quality of life of 265 HCWs working in a hospital in central town but using a different method of assessment; professional quality of life score (PRO-QOL). This tool measures three aspects; compassion satisfaction, secondary traumatization and burn out. Similar to our findings, they found that in general, they experience a poor outcome [25]. In our study, we found that physical quality of life was significantly associated with COVID wave difference and medical job difference were significantly associated with quality-of-life changes (p=0.005, p<0.001) respectively. However, psychological health was significantly associated with age and medical job differences (p=0.029, p=0.005) respectively. The social QOL was significantly dependent on age, COVID waves and medical job differences (p=0.003, p=0.005, p=0.009) respectively. However, environmental QOL was found to be associated with COVID wave and job differences (p<0.001, p=0.003) respectively. Social support especially from friends and family was found to be associated with higher quality of life [24].
5. Conclusion
Health care workers (HCWs) are prone to experience high levels of stress in pandemics as the current one; COVID-19. Despite there are many scales for measuring the degree of stress, all of them proved that stress and other psychiatric disturbances can occur at the time of pandemic. So, interventions must be made in order not to make HCWs negatively affected which in turn is reflected on the quality of the health system.
Authors Contributions
MH: study concept, critical revision of the manuscript, and design. MY and HH: study concept, and design, and critical revision of the manuscript. ZE and OA: recruitment of cases, analysis, interpretation of data, writing and editing the manuscript. YM: study concept, analysis, design, interpretation of data, and critical revision of the manuscript. All authors approved the final version of the manuscript and the manuscript submission to the specific reports.
Ethics declarations
The nature of the study was discussed with each participant and written informed consent was obtained from all participants before participating in the study. This study was approved by University Hospital Ethics Committee after a very clear statement that provided information on the following points; study rationale, participation in this study was completely free and voluntary, participation in the study had no direct benefit to the participant, although the data obtained could be used for the benefit of other patients, they may be withdrawn at any time without giving any justification and without affecting their care service, and the results of the study may be used for scientific publication but the identities of the patients and would be completely secret.
Human Rights and Animal Rights
No animal was used in this research. All human research procedures followed were in accordance with the ethical standard of the committee responsible for human experimentation (institutional and national) and with Helsinki Declaration of 1975, as revised in 2008.
Consent for Publication
Written informed consent was obtained from each participant prior to the study for publication of this research.
Availability of Data and Materials
Data supporting the findings of the article isn’t publicly available as a result of the privacy policies of the health facilities involved in the study, but it can be provided by the corresponding author on reasonable request.
Funding
"This research received no specific grant from any funding agency, commercial or not-for-profit-sectors".
Competing interests
The authors report no conflict of interest.
Acknowledgments
All authors are grateful for participating mental hospitals for providing us by data and volunteers of cases helped us to do such work. Finally for all volunteers’ participants who were very helpful in sharing in this work from all staff include psychiatrist, psychologist, internal medicine doctors, nurses, security, service and administrative team.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (2020): 497-506.
- Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nat 579 (2020): 265-269.
- Eder SJ, Steyrl D, Stefanczyk MM, et al. A. Predicting fear and perceived health during the COVID-19 pandemic using machine learning: A cross-national longitudinal study; PLoS ONE 1 (2021): 0247997.
- Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr 51 (2020):102080.
- Kar SK, Arafat SMY, Kabir R, et al. Coping with Mental Health Challenges During COVID-19. Coronavirus Dis 199 (2019).
- Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J Psychiatr 51 (2021).
- Vinck P, Pham PN, Bindu KK, et al. Institutional trust and misinformation in the response to the 2018-19 Ebola outbreaks in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis 19 (2019): 529-536.
- Rossler W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin Neurosci 266 (2016): 381.
- Thakur V, Jain A. COVID 2019-suicides: A global psychological pandemic. Brain, Behaviour, and Immunity, 88 (2020): 952- 953.
- World Health Organization (2020).
- Orley J. Programme on Mental Health World Health Organization CH-1211 Geneva 27, Switzerland, page 4. WHO instruction 76 (1996).
- Davey C, Heard R, Lennings C. Development of the Arabic versions of the Impact of Events Scale-Revised and the Posttraumatic Growth Inventory to assess trauma and growth in Middle Eastern refugees in Australia, Clinical Psychologist 19 (2014): 12043.
- Taylor S, Landry CA, Paluszek MM, et al. Development and initial validation of the COVID Stress Scales. J Anxiety Disord 72 (2020): 102232.
- The World Health Organization Quality of life assessment. Soc Sci Med 41 (1995): 1403.
- Vizheh M, Qorbani M, Arzaghi S, et al. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord 19 (2020): 1967-1978.
- Johns Hopkins Coronavirus Resource Center COVID-19 Map (2021).
- Pereira-Sanchez V, Adiukwu F, EL Hayek S, et al. COVID-19 effect on mental health: patients and workforce. The Lancet Psychiatry 7 (2020): e29-30.
- Koh D, Meng KL, Sin EC, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Med Care 43 (2005): 676-682.
- Lee AM, Wong JG, McAlonan GM, et al. Stress and Psychological Distress among SARS Survivors 1 Year after the Outbreak, the Canadian Journal of Psychiatry 52 (2007): 233-240.
- Fernández IAM, Moreno SC Díaz LC, et al. Fear, Stress, and Knowledge regarding COVID-19 in Nursing Students and Recent Graduates in Mexico. Investig y Educ en Enferm 39 (2021): 1-12.
- De Kock JH, Latham HA, Leslie SJ, et al. et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being.BMC Public Health 21 (2021): 104.
- Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr 52 (2020): 102066.
- Asante JO, Li MJ, Liao J, et al. The relationship between psychosocial risk factors, burnout and quality of life among primary healthcare workers in rural Guangdong province: a cross-sectional study. BMC Health Serv Res 19 (2019).
- Woon LSC, Mansor NS, Mohamad MA, et al. Quality of Life and Its Predictive Factors among Healthcare Workers after the End of a Movement Lockdown: The Salient Roles of COVID-19 Stressors, Psychological Experience, and Social Support. Front Psychol 12 (2021): 652326.
- Buselli R, Corsi M, Baldanzi S, et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). Int J Environ Res Public Health17 (2020): 1-12.
