Impact of Personality and Experiences of Interventional Radiologists in Outcome of CT-Guided Percutaneous Lung Biopsies
Article Information
Kühn JP1,4, Kromrey ML1, Schulze L2, Schäfer S1, Ittermann T3, Mensel B1, Radosa CG4, Grabe H2, Hoffmann RT4
1Institute of Diagnostic Radiology and Neuroradiology, University Medicine Greifswald, Greifswald, Germany
2Department of Psychiatry and Psychotherapy, University Medicine Greifswald, Greifswald, Germany
3Institute of Community Medicine, University Medicine Greifswald, Greifswald, Germany
4Institute and Policlinic of Radiology and Interventional Radiology, University Hospital Carl Gustav Carus, TU Dresden, Dresden, Germany
*Corresponding Author: Jens-Peter Kühn, Institute and Policlinic of Radiology and Interventional Radiology University Medicine, University Hospital Carl Gustav Carus, TU Dresden Dresden, D-01277, Germany
Received: 01 September 2019; Accepted: 16 September 2019; Published: 19 September 2019
Citation: Kühn JP, Kromrey ML, Schulze L, Schäfer S, Ittermann T, Mensel B, Radosa CG, Grabe H, Hoffmann RT. Impact of Personality and Experiences of Interventional Radiologists in Outcome of CT-Guided Percutaneous Lung Biopsies. Journal of Radiology and Clinical Imaging 2 (2019): 034-044.
Share at FacebookAbstract
Purpose: To investigate how personality traits and professional experience of interventional radiologists affect outcome and complications in computed-tomography (CT)-guided percutaneous transthoracic needle biopsy (PTNB) of pulmonary nodules.
Materials and Methods: A retrospective database search retrieved 1,056 PTNBs carried out by 38 interventional radiologists from 2006 through 2014, and 445 interventions performed by 14 radiologists were included in the study (exclusion criteria: lack of consent by radiologist, less than 20 PTNBs performed by the radiologist, and PTNB with incomplete data). Interventions were evaluated with regard to the occurrence of complications, technical success, and intervention-related predictors. Personality traits of interventionalists were assessed using the NEO-FFI-30 (questionnaire measuring the “Big Five”) and State-Trait Anxiety Inventory. Outcome of PTNB was adjusted for intervention-related predictors and matched with factors describing the personality and experience of each of the 14 radiologists.
Results: There were no significant differences among the 14 radiologists in terms of technical success (range: 75.0-95.5%, P=0.406) and overall complication rate (range: 44.7-85.7%, P=0.088) or major (range: 15.6- J Radiol Clin Imaging 2019; 2 (3): 034-044 DOI: 10.26502/jrci.2809012 Journal of Radiology and Clinical Imaging 35 40.9%, P=0.679) and minor complications (range: 31.6-71.4%, P=0.074). Personality traits had no effect on technical success and complication rates, and there was likewise no effect of years of practical experience on technical success (P=0.254) or complications (P=0.470).
Conclusion: Personality traits and practical experience of the interventional radiologist have no impact on the technical success or complication rate of PTNB.
Keywords
Interventional radiology; Percutaneous lung biopsy; PTNB; Personality
Interventional radiology articles, Percutaneous lung biopsy articles, PTNB articles, Personality articles
Interventional radiology articles Interventional radiology Research articles Interventional radiology review articles Interventional radiology PubMed articles Interventional radiology PubMed Central articles Interventional radiology 2023 articles Interventional radiology 2024 articles Interventional radiology Scopus articles Interventional radiology impact factor journals Interventional radiology Scopus journals Interventional radiology PubMed journals Interventional radiology medical journals Interventional radiology free journals Interventional radiology best journals Interventional radiology top journals Interventional radiology free medical journals Interventional radiology famous journals Interventional radiology Google Scholar indexed journals Percutaneous lung biopsy articles Percutaneous lung biopsy Research articles Percutaneous lung biopsy review articles Percutaneous lung biopsy PubMed articles Percutaneous lung biopsy PubMed Central articles Percutaneous lung biopsy 2023 articles Percutaneous lung biopsy 2024 articles Percutaneous lung biopsy Scopus articles Percutaneous lung biopsy impact factor journals Percutaneous lung biopsy Scopus journals Percutaneous lung biopsy PubMed journals Percutaneous lung biopsy medical journals Percutaneous lung biopsy free journals Percutaneous lung biopsy best journals Percutaneous lung biopsy top journals Percutaneous lung biopsy free medical journals Percutaneous lung biopsy famous journals Percutaneous lung biopsy Google Scholar indexed journals percutaneous transthoracic needle biopsy articles percutaneous transthoracic needle biopsy Research articles percutaneous transthoracic needle biopsy review articles percutaneous transthoracic needle biopsy PubMed articles percutaneous transthoracic needle biopsy PubMed Central articles percutaneous transthoracic needle biopsy 2023 articles percutaneous transthoracic needle biopsy 2024 articles percutaneous transthoracic needle biopsy Scopus articles percutaneous transthoracic needle biopsy impact factor journals percutaneous transthoracic needle biopsy Scopus journals percutaneous transthoracic needle biopsy PubMed journals percutaneous transthoracic needle biopsy medical journals percutaneous transthoracic needle biopsy free journals percutaneous transthoracic needle biopsy best journals percutaneous transthoracic needle biopsy top journals percutaneous transthoracic needle biopsy free medical journals percutaneous transthoracic needle biopsy famous journals percutaneous transthoracic needle biopsy Google Scholar indexed journals Personality articles Personality Research articles Personality review articles Personality PubMed articles Personality PubMed Central articles Personality 2023 articles Personality 2024 articles Personality Scopus articles Personality impact factor journals Personality Scopus journals Personality PubMed journals Personality medical journals Personality free journals Personality best journals Personality top journals Personality free medical journals Personality famous journals Personality Google Scholar indexed journals computed-tomography articles computed-tomography Research articles computed-tomography review articles computed-tomography PubMed articles computed-tomography PubMed Central articles computed-tomography 2023 articles computed-tomography 2024 articles computed-tomography Scopus articles computed-tomography impact factor journals computed-tomography Scopus journals computed-tomography PubMed journals computed-tomography medical journals computed-tomography free journals computed-tomography best journals computed-tomography top journals computed-tomography free medical journals computed-tomography famous journals computed-tomography Google Scholar indexed journals CT-guided PTNB articles CT-guided PTNB Research articles CT-guided PTNB review articles CT-guided PTNB PubMed articles CT-guided PTNB PubMed Central articles CT-guided PTNB 2023 articles CT-guided PTNB 2024 articles CT-guided PTNB Scopus articles CT-guided PTNB impact factor journals CT-guided PTNB Scopus journals CT-guided PTNB PubMed journals CT-guided PTNB medical journals CT-guided PTNB free journals CT-guided PTNB best journals CT-guided PTNB top journals CT-guided PTNB free medical journals CT-guided PTNB famous journals CT-guided PTNB Google Scholar indexed journals radiologist articles radiologist Research articles radiologist review articles radiologist PubMed articles radiologist PubMed Central articles radiologist 2023 articles radiologist 2024 articles radiologist Scopus articles radiologist impact factor journals radiologist Scopus journals radiologist PubMed journals radiologist medical journals radiologist free journals radiologist best journals radiologist top journals radiologist free medical journals radiologist famous journals radiologist Google Scholar indexed journals State-Trait Anxiety Inventory articles State-Trait Anxiety Inventory Research articles State-Trait Anxiety Inventory review articles State-Trait Anxiety Inventory PubMed articles State-Trait Anxiety Inventory PubMed Central articles State-Trait Anxiety Inventory 2023 articles State-Trait Anxiety Inventory 2024 articles State-Trait Anxiety Inventory Scopus articles State-Trait Anxiety Inventory impact factor journals State-Trait Anxiety Inventory Scopus journals State-Trait Anxiety Inventory PubMed journals State-Trait Anxiety Inventory medical journals State-Trait Anxiety Inventory free journals State-Trait Anxiety Inventory best journals State-Trait Anxiety Inventory top journals State-Trait Anxiety Inventory free medical journals State-Trait Anxiety Inventory famous journals State-Trait Anxiety Inventory Google Scholar indexed journals Percutaneous Lung Biopsies articles Percutaneous Lung Biopsies Research articles Percutaneous Lung Biopsies review articles Percutaneous Lung Biopsies PubMed articles Percutaneous Lung Biopsies PubMed Central articles Percutaneous Lung Biopsies 2023 articles Percutaneous Lung Biopsies 2024 articles Percutaneous Lung Biopsies Scopus articles Percutaneous Lung Biopsies impact factor journals Percutaneous Lung Biopsies Scopus journals Percutaneous Lung Biopsies PubMed journals Percutaneous Lung Biopsies medical journals Percutaneous Lung Biopsies free journals Percutaneous Lung Biopsies best journals Percutaneous Lung Biopsies top journals Percutaneous Lung Biopsies free medical journals Percutaneous Lung Biopsies famous journals Percutaneous Lung Biopsies Google Scholar indexed journals NEO-FFI-30 articles NEO-FFI-30 Research articles NEO-FFI-30 review articles NEO-FFI-30 PubMed articles NEO-FFI-30 PubMed Central articles NEO-FFI-30 2023 articles NEO-FFI-30 2024 articles NEO-FFI-30 Scopus articles NEO-FFI-30 impact factor journals NEO-FFI-30 Scopus journals NEO-FFI-30 PubMed journals NEO-FFI-30 medical journals NEO-FFI-30 free journals NEO-FFI-30 best journals NEO-FFI-30 top journals NEO-FFI-30 free medical journals NEO-FFI-30 famous journals NEO-FFI-30 Google Scholar indexed journals
Article Details
1. Introduction
Interventional radiology is a subspecialty within radiology and includes the complete spectrum of minimal-invasive interventions ranging from image-guided diagnostic procedures to acute and elective therapeutic interventions. To become a certified interventional radiologist, a resident needs an excellent medical background and practical skills and experience. Little is known about whether the experience and personality of an interventional radiologist also affect the outcome of interventions performed by him or her. Therefore, it is not clear at present whether everyone is suitable to become an interventional radiologist.
Computed-tomography-guided percutaneous transthoracic needle biopsy (CT-guided PTNB) of the lung is a challenging intervention with several complications including serious events such as pneumothorax and pulmonary bleeding with frequencies of 17-60% [1-7] and 1-29% [8-11], respectively. Hemoptysis occurs in very few cases (0.2-4%) [8,12]. For these reasons, PTNB of suspicious pulmonary lesions is a good candidate for evaluating how the interventional radiologist’s experience and personality might affect outcome. Therefore, the purpose of this study was to investigate how personality traits and practical experience of interventional radiologists affect the outcome and occurrence of complications in patients undergoing CT-guided PTNB of pulmonary nodules.
2. Materials and Methods
The local ethics committee of the University Greifswald approved this study. Written informed consent was obtained
from all interventional radiologists included in our analysis. Analysis of intervention-related predictors and outcome of PTNB as well as assessment of practical experience and personality traits were performed by a medical student unrelated to the participating interventional radiologists.
2.1 CT-guided percutaneous transthoracic lung biopsy (PTNB)
Indications for CT-guided PTNB were established by a certified tumor board consisting of a surgeon, an internal medicine specialist, a pathologist, and an interventional radiologist. Individual risk assessment was performed for each patient, and an interventional radiologist finally decided about the intervention based on the following criteria: morphology and location of the lesion, length of interventional pathway, and patient comorbidities. CT-guided PTNB was randomly carried out by the radiologist who was assigned to the workplace at the time of intervention. Before the intervention, the radiologist checked the patient’s laboratory values, especially coagulation parameters, planned the strategy, and ensured that informed consent to undergo biopsy was available. Thereafter, CT-guided PTNB was performed in a standardized manner using a 14-18 Gauge biopsy system (Quick-Core Biopsy needle, Cook Medical USA) with a through length of 2 cm) The interventionalist decided whether to obtain more samples for final histopathologic diagnosis. At the end of the procedure, a final CT scan was acquired to identify possible complications such as pneumothorax or hemorrhage. In addition, a postinterventional chest X-ray was performed after four hours. Figure 1demonstrates and overview of the interventional procedure.
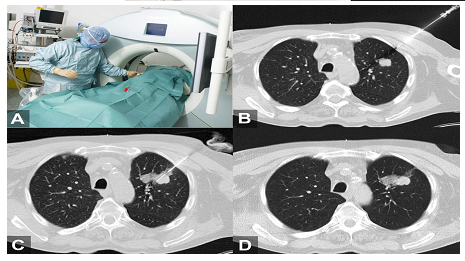
Figure 1: Procedure of computer tomography-guided PTNB. A) Setting of an image-guided PTNB under sterile conditions. B) After local anesthesia a coaxial needle system was placed in the direction of the suspected pulmonary nodules. C) Thereafter, biopsy cannula/stylet was placed within the nodule, especially in the boundary of the tumor. D) Finally, computer tomography was performed after biopsy to exclude complications. In this case a hemorrhage as minor complication was observed, which required no further treatment.
2.2 Patients and interventional radiologists
From 2006 through 2014, a total of 1,056 clinically indicated CT-guided PTNB of potential malignant pulmonary nodules in 981 patients were performed. The study center is a training facility for radiologists subspecializing in interventional radiology. During the 8-year study period, 38 radiologists performed CT-guided PTNB. Transthoracic biopsies performed by radiologists not consenting to study participation or who had an experience of less than 20 prior PTNBs and PTNB with incomplete data were excluded, resulting in 445 interventions performed by 14 radiologists that were included in our retrospective analysis. Characteristics of the 14 radiologists are presented in Table 1.
Table 1: Characteristics of the 14 interventional radiologists.
2.3 Definition of outcome and procedure-related predictors
The outcome of each intervention was defined by the technical success and the occurrence of overall complications and minor and major complications. Following the new CIRSE (Cardiovascular and Interventional Radiological Society) recommendations regarding the classification of complications in the setting of quality assurance [13], minor complications correspond to grades 1 and 2 and major complications to grade 3 and above. We defined technical success, if histopathology confirmed a malignant lesion. Histopathologically benign lesions were followed up after 3 - 6 months. Technical success of these benign lesions was finally verified if the tumor demonstrated no progression in the follow-up.
Complications were assessed during hospitalization. Intervention-related complications not requiring treatment, e.g., small pneumothorax, were defined as minor complications. Major complications were intervention-related complications requiring treatment or resulting in a longer hospital stay, e.g., pneumothorax requiring chest tube placement. In addition, potential predictors influencing technical success and rate of complications were assessed. These included lesion size, tumor localization, pleural contact of the tumor, length of interventional pathway, needle size, and number of pleural passes.
2.4 Interventionalists’ experience and personality traits
Two features related to interventionalists were assessed: professional experience and personality traits. Professional experience was assessed based on the start of residency. The State-Trait Anxiety Inventory (STAI-TRAIT) was used to assess anxiety. The inventory consists of two subscales measuring anxiety as both state and trait. Here, we only assessed trait-anxiety, i.e., transsituational, persistent anxiety as a general condition. This subscale contains 20 items and scores range from 20 (no anxiety) to 80 (maximum manifestation of anxiety) [14]. The Big-Five Inventory (BFI) is a tool to assess the well-known five dimensions of personality - openness, conscientiousness, extraversion, agreeableness and neuroticism - defined by the Five Factor Theory of Personality [15, 16]. Radiologists were asked to rate 44 items on a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree).
2.5 Statistics
Intervention-related predictors were associated with technical success and complications in multivariable logistic regressions. Differences in technical success or complications between individual interventional radiologists were evaluated by likelihood ratio tests comparing two logistic regression models – the first adjusted for lesion size, interventional pathway, and pleural contact, and the second with the interventional radiologists. Associations of personal traits with technical success and complications were investigated by mixed-effects logistic regression models. Here, the respective personal trait was set as fixed effect and the confounders, i.e., lesion size, length of interventional pathway, and pleural contact, were set as random effects. For calculation, we used the meqrlogit command in Stata with Laplacian approximation.
Since multiple tests were performed (n=24) to associate personality traits with technical success and complications, we used a Bonferroni correction for the level of significance. Thus, a P-value <0.002 was considered to indicate statistically significant differences in all analyses. All analyses were conducted using Stata 14.1 (Stata Corporation, College Station, TX, USA).
3. Results
Fourteen interventional radiologists with a prior experience of more than 20 PTNB who consented to participate in this study and undergo testing of personality traits were analyzed. The study results are based on the analysis of 445 interventions in 442 patients. Exclusion criteria for CT-guided PTNB interventions and for interventional radiologists performing the procedures are summarized in Figure 2.
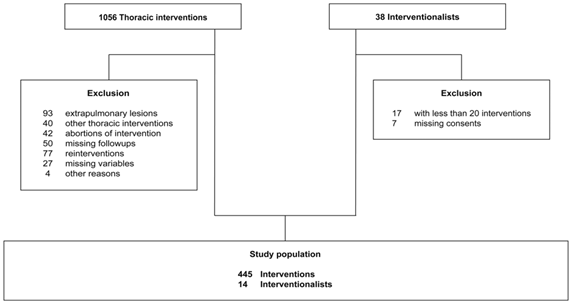
Figure 2: Flow chart of inclusion and exclusion criteria.
The intervention-related predictors investigated had no significant influence on technical success: lesion size (OR: 1.10; P=0.259), pleural contact of the tumor (OR: 1.42; P=0.273), length of interventional pathway (OR: 0.97; P=0.622), needle size with reference 18 Gauge (OR: 1.20; P=0.567), tumor localization (right/left) (OR: 0.89; P=0.664), and tumor localization (peripheral/central) (OR: 0.84; P=0.721).
In contrast, the rate of complications was significantly influenced by lesion size (OR: 0.77; P ≤ 0.001), length of interventional pathway (OR: 1.33; P ≤ 0.001), and pleural contact of the tumor (OR: 0.23; P ≤ 0.001). A summary of predictors’ influence on technical success and rate of complications, including minor and major complications, is given in Table 2.
OR=odds ratio; 95%-CI=confidence interval; p=level of significance
Table 2: Predictors of technical success and rate of complications.
After adjustment for relevant predictors, i.e., lesion size, length of interventional pathway, and pleural contact of the tumor, we found no significant difference among the 14 interventional radiologists in terms of technical success, which ranged from 75.0% to 95.5% with a mean ± SD of 85.3 ± 6.4% (P=0.406). We also found no significant difference among the interventional radiologists in terms of complication rates, which ranged from 44.7% to 85.7%, mean ± SD: 66.1 ± 10.8% (P=0.088). This applied to both major complications (range 15.6 - 40.9%; mean ± SD: 21.5 ± 6.6%; P=0.679) and minor complications (31.6-71.4%; mean ± SD: 53.4 ± 11.8%; P=0.074).
Interventionalists varied in their experience, ranging from 1.3 to 21.8 years (mean ± SD: 8.3 ± 5.0 years), but years of experience in radiology had no significant influence on technical success (OR: 1.00; (0.99; 1.00); P=0.254) or on the rate of overall complications (OR: 1.00; (0.99; 1.02); P=0.470), minor complications (OR: 1.00; (0.99; 1.00); P=0.381) and major complications (OR: 1.00; (1.00; 1.00); P=0.866). The personality test scores for the five items of the STAI-TRAIT were as follows: anxiety: 27-57 points (mean 37.8 ± 9.6 points): openness to experience: 7-19 points (mean 12.5 ± 2.9 points); conscientiousness: 12-18 points (mean 14.8 ± 2.1 points); extraversion: 8-16 points (mean 10.3 ± 2.1 points); agreeableness: 7-18 points (mean 14.1 ± 2.8 points); and neuroticism: 8-16 points (mean 8.3 ± 2.7 points) (Table 3; Figure 3).
Overall personality traits had no effect on technical success or the occurrence of complications (Table 4). Categorizing interventional radiologists in groups according to lower 25th percentile and higher 75th percentile confirmed this result (data not shown).
Data are expressed as median, 25th and 75th percentile
Table 3: Personal traits in relation to technical success and rate of complications.
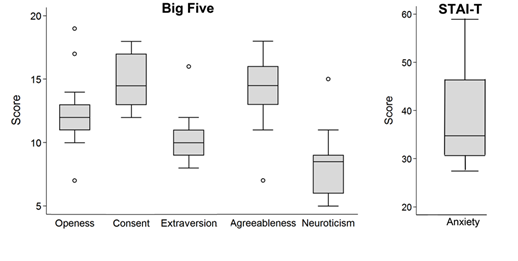
Figure 3: Distribution of personality and mental traits (A - Big-Five; B - STAIT-TRAIT) of 14 interventional radiologists. A higher score indicates a higher expression of the trait.
OR=odds ratio; 95%-CI=confidence interval; p=level of significance
Table 4: Influence of personality traits on technical success and complication rate.
4. Discussion
Our study investigated how the personality and experience of interventional radiologists affected the technical success and complication rates of CT-guided percutaneous transthoracic pulmonary biopsies (PTNB). We found no significant influence of interventionalists’ experience and the personality traits investigated here on technical success or complications. Psychological testing is increasing being used to select residents for the different medical specialties. The Department of Radiology of Baylor College of Medicine (Houston, Texas) developed a structured interview procedure to measure both noncognitive and cognitive qualities of candidates [17]. The authors defined five attributes - interpersonal skills, recognition of limits, curiosity, conscientiousness, and confidence level – as most essential for a radiology resident’s performance and were able to select better residents from a personality point of view based on these criteria. This was the rationale for our study, as psychological concepts might also be helpful in selecting suitable candidates for training in interventional radiology.
Several studies have shown that personality traits play a role in the selection of subspecialties by physicians. For instance, Warschkow et al. show that surgeons are characterized by an excess of achievement orientation and extraversion, whereas internists have decreased aggressiveness [18]. Interestingly, their study reveals a discrepancy between self- and external assessment of personality only among surgeons. Another study comparing surgeons and other physicians by McCulloch et al. demonstrated that surgeons were significantly more extraverted, more intolerant of uncertainty, and less neurotic than their internal medicine colleagues [19]. Likewise, surgical residents were found to score higher for conscientiousness, extraversion, and openness than the general population [20]. However, all studies conducted so far have investigated personality traits in terms of differences between specialties but not with regard to how they might affect the outcome of treatment or interventional procedures. For the reasons outlined above, transthoracic biopsy is a good case in point to evaluate the influence of the interventionalist’s experience and personality on outcome.
PTNB is routinely used for lesion characterization as it has fewer complications than open surgery. The most common complications after PTNB are pneumothorax with an incidence of up to 50-60% [1-6] and pulmonary hemorrhage with 1-29% [8-11]. To reduce these high rates, recent research has focused on identifying possible predictors of PTNB-related complications. These studies have revealed that the rate of complications is predominantly affected by lesion size, length of interventional pathway, and pleural contact of the tumor [21, 22]. Other possible intervention-related risk factors include presence of pulmonary emphysema and body position [1, 21, 23]. To the best of our knowledge, the possible role of personality traits or experience of the radiologist performing PTNB has not been investigated before.
We found no significant influence of interventionalists’ experience and five major personality traits - anxiety, openness, conscientiousness, extraversion, agreeableness. and neuroticism - on technical success and complication rates. Our study has several limitations. We retrospectively analyzed patient data from interventions performed over an eight-year period. In contrast, personality traits of the interventionalists were prospectively assessed at a single point in time and might have changed over time, for example through further training or growing experience. It is possible that, in some instances, difficult biopsies were performed by more experienced radiologists or by a junior interventional radiologist assisted by an experienced interventionalist. Such cases might have biased our results. To increase the robustness of our results, we considered influencing confounders as described above. However, other possible predictors not investigated, e.g., pulmonary emphysema, could also have had an impact on our findings. Finally, we defined technical success if a malignant result was obtained or if in the case of benign result, the lesion was stable on a 3-6 month follow-up. The time interval of less than 6 months might be too short for a final diagnosis.
5. Conclusion
In conclusion, PTNB is a clinically accepted procedure with a high technical success and a moderate rate of complications. Lesion size, tumor localization, and length of interventional pathway are predictors of technical success of PTNB but appear to have no influence on the complication rate. Personality traits and professional experience of the interventional radiologist have no impact on the technical success or complication rate of PTNB.
6. Main Points
- CT-guided percutaneous transthoracic needle biopsy of pulmonary nodules has a high technical success and a moderate complication rate.
- Lesion size, tumor localization, and length of interventional pathway are predictors of technical success of PTNB but appear to have no influence on the complication rate.
- Years of experience and personality traits of interventional radiologists play a minor part in the outcome of PTNB.
References
- Nakamura M, Yoshizako T, Koyama S, et al. Risk factors influencing chest tube placement among patients with pneumothorax because of CT-guided needle biopsy of the lung. J Med Imaging Radiat Oncol 55 (2011): 474-478.
- Mahnken AH. Invasive procedure for clarification of pulmonary nodules. Radiologe 54 (2014): 478-84.
- Connor S, Dyer J, Guest P. Image-guided automated needle biopsy of 106 thoracic lesions: a retrospective review of diagnostic accuracy and complication rates. Eur Radiol 10 (2000): 490-494.
- Geraghty PR, Kee ST, McFarlane G, et al. CT-guided transthoracic needle aspiration biopsy of pulmonary nodules: needle size and pneumothorax rate. Radiology 229 (2003): 475-481.
- Tomiyama N, Yasuhara Y, Nakajima Y, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 59 (2006): 60-64.
- Otto S, Mensel B, Friedrich N, et al. Predictors of technical success and rate of complications of image-guided percutaneous transthoracic lung needle biopsy of pulmonary tumors. PLoS One 10 (2015): e0124947.
- Saji H, Nakamura H, Tsuchida T, et al. The incidence and the risk of pneumothorax and chest tube placement after percutaneous CT-guided lung biopsy - The angle of the needle trajectory is a novel predictor. Chest 121 (2002): 1521-1526.
- Poulou LS, Tsagouli P, Ziakas PD, et al. Computed tomography-guided needle aspiration and biopsy of pulmonary lesions: a single-center experience in 1000 patients. Acta Radiol 54 (2013): 640-645.
- Chakrabarti B, Earis JE, Pandey R, et al. Risk assessment of pneumothorax and pulmonary haemorrhage complicating percutaneous co-axial cutting needle lung biopsy. Respir Med 103 (2009): 449-455.
- Wiener RS, Schwartz LM, Woloshin S, et al. Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med 155 (2011): 137-144.
- Priola AM, Priola SM, Cataldi A, et al. Diagnostic accuracy and complication rate of CT-guided fine needle aspiration biopsy of lung lesions: a study based on the experience of the cytopathologist. Acta Radiol 51 (2010): 527-533.
- D'Alessandro V, Parracino T, Stranieri A, et al. Computed-tomographic-guided biopsy of thoracic nodules: a revision of 583 lesions. Clin Ter 158 (2007): 509-513.
- Filippiadis DK, Binkert C, Pellerin O, et al. Cirse Quality Assurance Document and Standards forClassification of Complications: The Cirse Classification System. Cardiovasc Intervent Radiol 40 (2017): 1141-1146.
- Spielberger CDG, Lushene RE, Vagg PR, et al. Manual for the state-trait anxiety inventory. Palo Alto, CA (1983).
- Digman JM. Personality Structure - Emergence of the 5-Factor Model. Annu Rev Psychol 41 (1990): 417-440.
- Goldberg LR. An alternative "description of personality": the big-five factor structure. J Pers Soc Psychol 59 (1990): 1216-1229.
- Lamki N, Watson AB, Fisher RG. Radiology resident selection: Objective Restructured Interview to assess five essential attributes. J Sci Res Med Sci 5 (2003): 27-30.
- Warschkow R, Steffen T, Spillmann M, et al. A comparative cross-sectional study of personality traits in internists and surgeons. Surgery 148 (2010): 901-907.
- McCulloch P, Kaul A, Wagstaff GF, et al. Tolerance of uncertainty, extroversion, neuroticism and attitudes to randomized controlled trials among surgeons and physicians. Br J Surg 92 (2005): 1293-1297.
- McGreevy J, Wiebe D. A preliminary measurement of the surgical personality. Am J Surg 184 (2002): 121-125.
- Boskovic T, Stanic J, Pena-Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis 1 (2014): S99-S107.
- Laurent F, Michel P, Latrabe V, et al. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy using a coaxial technique: Incidence and risk factors. Am J Roentgenol 172 (1999): 1049-1053.
- Lendeckel D, Kromrey ML, Ittermann T, et al. Pulmonary emphysema is a predictor of pneumothorax after CT-guided transthoracic pulmonary biopsies of pulmonary nodules. PLoS One 12 (2017): e0178078.
