Impact of Indication for Labour Induction on Caesarean Section Delivery
Article Information
Jasmeet Kumari*, Anam Munir, Maire Milner
Department of Obstetrics and Gynaecology, Our Lady of Lourdes Hospital Drogheda, Republic of Ireland
*Corresponding Author: Jasmeet Kumari, Department of Obstetrics & Gynaecology, Our Lady of Lourdes Hospital, Drogheda, Republic of Ireland
Received: 29 March 2021; Accepted: 07 April 2021; Published: 16 April 2021
Citation:
Jasmeet Kumari, Anam Munir, Maire Milner. Impact of Indication for Labour Induction on Caesarean Section Delivery. Obstetrics and Gynecology Research 4 (2021): 101-107.
Share at FacebookAbstract
Objective: The aim of this study is to determine the impact of indication for induction of labour on mode of delivery. Study design: A retrospective study.
Place and duration of study: Our Lady of Lourdes Hospital, Drogheda, RCSI group of hospitals, Ireland, from 1st January 2019 till 31st December 2019.
Methodology: In this retrospective cohort 409 case notes of primigravida whose labour was induced were selected. Indication for induction, Gestational age, parity, BMI and mode of delivery was taken into account.
Results: In 2019, 2908 patients delivered a baby over 500g in the unit. Among these 1011 (34.8%) were primipara and 1897(65.2%) were multipara. The caesarean section (CS) rate for the year was 34.3% and induction rate 32.3%.
Conclusion: Mode of delivery was affected by indication of induction which was highest among women induced for suspected macrosomia. CS is a major surgery with adverse risks to mother both in current and subsequent pregnancies. Maternal demographic factors like obesity (BMI >30), advanced birth weeks and, nulliparity are independent risk factors for CS risk. A planned caesarean deliveryshould be discussed with the woman in presence of secondary risk factors, to avoid the trauma and prolong hospitalization that can result from failed induction.
Keywords
Labour Induction, Caesarean Section
Labour Induction articles Labour Induction Research articles Labour Induction review articles Labour Induction PubMed articles Labour Induction PubMed Central articles Labour Induction 2023 articles Labour Induction 2024 articles Labour Induction Scopus articles Labour Induction impact factor journals Labour Induction Scopus journals Labour Induction PubMed journals Labour Induction medical journals Labour Induction free journals Labour Induction best journals Labour Induction top journals Labour Induction free medical journals Labour Induction famous journals Labour Induction Google Scholar indexed journals Caesarean Section articles Caesarean Section Research articles Caesarean Section review articles Caesarean Section PubMed articles Caesarean Section PubMed Central articles Caesarean Section 2023 articles Caesarean Section 2024 articles Caesarean Section Scopus articles Caesarean Section impact factor journals Caesarean Section Scopus journals Caesarean Section PubMed journals Caesarean Section medical journals Caesarean Section free journals Caesarean Section best journals Caesarean Section top journals Caesarean Section free medical journals Caesarean Section famous journals Caesarean Section Google Scholar indexed journals maternal articles maternal Research articles maternal review articles maternal PubMed articles maternal PubMed Central articles maternal 2023 articles maternal 2024 articles maternal Scopus articles maternal impact factor journals maternal Scopus journals maternal PubMed journals maternal medical journals maternal free journals maternal best journals maternal top journals maternal free medical journals maternal famous journals maternal Google Scholar indexed journals vaginal delivery articles vaginal delivery Research articles vaginal delivery review articles vaginal delivery PubMed articles vaginal delivery PubMed Central articles vaginal delivery 2023 articles vaginal delivery 2024 articles vaginal delivery Scopus articles vaginal delivery impact factor journals vaginal delivery Scopus journals vaginal delivery PubMed journals vaginal delivery medical journals vaginal delivery free journals vaginal delivery best journals vaginal delivery top journals vaginal delivery free medical journals vaginal delivery famous journals vaginal delivery Google Scholar indexed journals twin pregnancies articles twin pregnancies Research articles twin pregnancies review articles twin pregnancies PubMed articles twin pregnancies PubMed Central articles twin pregnancies 2023 articles twin pregnancies 2024 articles twin pregnancies Scopus articles twin pregnancies impact factor journals twin pregnancies Scopus journals twin pregnancies PubMed journals twin pregnancies medical journals twin pregnancies free journals twin pregnancies best journals twin pregnancies top journals twin pregnancies free medical journals twin pregnancies famous journals twin pregnancies Google Scholar indexed journals gestation articles gestation Research articles gestation review articles gestation PubMed articles gestation PubMed Central articles gestation 2023 articles gestation 2024 articles gestation Scopus articles gestation impact factor journals gestation Scopus journals gestation PubMed journals gestation medical journals gestation free journals gestation best journals gestation top journals gestation free medical journals gestation famous journals gestation Google Scholar indexed journals fetal weight articles fetal weight Research articles fetal weight review articles fetal weight PubMed articles fetal weight PubMed Central articles fetal weight 2023 articles fetal weight 2024 articles fetal weight Scopus articles fetal weight impact factor journals fetal weight Scopus journals fetal weight PubMed journals fetal weight medical journals fetal weight free journals fetal weight best journals fetal weight top journals fetal weight free medical journals fetal weight famous journals fetal weight Google Scholar indexed journals antepartum haemorrhage articles antepartum haemorrhage Research articles antepartum haemorrhage review articles antepartum haemorrhage PubMed articles antepartum haemorrhage PubMed Central articles antepartum haemorrhage 2023 articles antepartum haemorrhage 2024 articles antepartum haemorrhage Scopus articles antepartum haemorrhage impact factor journals antepartum haemorrhage Scopus journals antepartum haemorrhage PubMed journals antepartum haemorrhage medical journals antepartum haemorrhage free journals antepartum haemorrhage best journals antepartum haemorrhage top journals antepartum haemorrhage free medical journals antepartum haemorrhage famous journals antepartum haemorrhage Google Scholar indexed journals IVF pregnancy articles IVF pregnancy Research articles IVF pregnancy review articles IVF pregnancy PubMed articles IVF pregnancy PubMed Central articles IVF pregnancy 2023 articles IVF pregnancy 2024 articles IVF pregnancy Scopus articles IVF pregnancy impact factor journals IVF pregnancy Scopus journals IVF pregnancy PubMed journals IVF pregnancy medical journals IVF pregnancy free journals IVF pregnancy best journals IVF pregnancy top journals IVF pregnancy free medical journals IVF pregnancy famous journals IVF pregnancy Google Scholar indexed journals maternal age articles maternal age Research articles maternal age review articles maternal age PubMed articles maternal age PubMed Central articles maternal age 2023 articles maternal age 2024 articles maternal age Scopus articles maternal age impact factor journals maternal age Scopus journals maternal age PubMed journals maternal age medical journals maternal age free journals maternal age best journals maternal age top journals maternal age free medical journals maternal age famous journals maternal age Google Scholar indexed journals
Article Details
1. Introduction
Induction of labour (IOL) rates have risen in recent decades [1]. In UK, caesarean deliveries have increased from 19.7% in 2000 to 26.2% in 2015 [1]. Indications include those which are based on strong evidence, e.g gestational diabetes (GDM), spontaneous rupture of membranes, hypertensive disorders, suspected fetal compromise, maternal age & those which are more dubious e.g. suspected fetal macrosomia and maternal request [2]. Clinicians should acknowledge the available evidence for decision making and discuss this with the patient. IOL increases the risk of caesarean section (CS) [3]. IOL for indications without strong supportive evidence may be one of the predictors for rising CS rate, this not only affects maternal health and future pregnancy but also has economic consequences [4]. CS carries almost a three times risk of maternal morbidity and mortality compared to vaginal delivery [5]. Wide variation in CS rates, from 14 to 52 percent in 31 different European countries has raised the issue of current practice [6]. The aim of this study is to relate the indications for IOL to delivery outcome.
2. Methods
This retrospective cohort study was conducted in a university affiliated Irish hospital with 2954 deliveries (including twin pregnancies) last year. The study population comprised 409 primigravida who underwent induction of labour and delivered at this hospital between January 1st and December 31st 2019. Patients with previous CS, multiple gestation and intrauterine fetal death were excluded A literature search was performed through Medline and Cochrane library using key words like “induction of labour”, “indications for induction of labour”, “risk of caesarean delivery with induction of labour”. Indication for induction of labour was noted. The primary outcome was mode of delivery; spontaneous vaginal delivery (SVD), operative delivery (OVD) and CS. The aim of this study was to determine the association between indication for IOL with risk of CS. The indications are classified as; (a) diabetes in pregnancy. (b) Suspected fetal compromise that includes small for gestational age (SGA) and intrauterine growth retardation (IUGR)-In this group, the estimated fetal weight was less than 10th percentile which is calculated from ultrasound and customised serial growth charts. (c) Hypertensive disorders in pregnancy, that includes chronic hypertension, pregnancy induced hypertension (PIH) and preeclampsia (PET). (d) Suspected macrosomia included estimated fetal weight as confirmed by growth ultrasound and customised growth chart was above 90th centile. (e) Spontaneous rupture of membrane (SROM) at term. (f) Postdates pregnancy, gestation > 40 weeks. (g) Induction for fetal concerns e.g. static growth/fall in growth, oligohydramnios, reduced fetal movements at term, antepartum haemorrhage, obstetric cholestasis and non-reassuring CTG. (h) Induction for miscellaneous factors, e.g. maternal age > 40 years, IVF pregnancy, maternal request for induction, polyhydramnios, raised liver function tests and headache in two patients (without any medical condition), In this group one patient had artificial rupture of membranes after successful external cephalic version, a patient was induced secondary to prolonged latent phase of first stage of labour, the reason for IOL in a patient was not known. To ensure clarity, patients with previous CS, multiple gestation and intrauterine fetal deaths were excluded. The main limitations are; being a single centered study with a year of maternity hospital data, it may not be applicable to other centers with different populations.
3. Results
Of the 409 women in our study having IOL, 139 (34%) had SVD. 116 (28.4%) OVD and 154 (37.6%) had CS. Of 105 women induced for SROM, 38 (36.2%) had SVD, 35(33.3%) had OVD and 32(30.5%) had CS. Of 80 women induced for post-dates, 25 31.2%) had SVD, 23(28.8%) had OVD and 32(40%) had CS. Of 54 women induced for GDM, 18 (33.3%) had SVD, 11(20.4%) had OVD and 25(46.3%) had CS. Of 48 patients induced for fetal concerns, 17(35.4%) had SVD, 13(27.1%) had OVD and 18(37.5%) had CS. Of 39 women induced for IUGR/SGA, 18(46.2%) had SVD, 14(35.9%) had OVD and 7(17.9%) had LSCS. Of 36 women induced for PIH or PET, 9(25%) had SVD, 8(22.2%) had OVD and 19(52.8%) had CS. The miscellaneous group of 33 women had induction between 39 and 40 weeks due indications as shown in table, 11/33(33.3%) had SVD, 9/3(27.3%) had OVD and 13/33(39.4%) had CS. Of 14 women induced for suspected fetal macrosomia 3(21.4%) had SVD, 3(21.4%) had OVD and 8(57.2%) had CS. 5/14(35.7%) patients had failed induction. Of 409 induced patients who delivered, postpartum haemorrhage was noted in 28 women: 13(46.4%) had CS, 9(32.2%) had OVD and 6(21.4%) had SVD. Number of babies admitted to Neonatal intensive care unit (NICU) were 33. 7/33 admissions were for low Apgar score and 26 were for short-term observation. No baby required cooling. Of 270 women who delivered vaginally, 3 had a third-degree perineal tear and 4 had shoulder dystocia. In these women shoulder dystocia was managed by first line maneuvers within 5 minutes of head delivery. These babies were born with good Apgar scores and no one required resuscitation. Their Birth weight ranged from 3.5kg to 4kg.
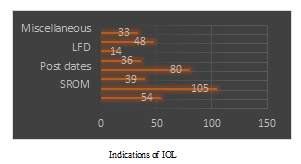
Figure 1: Indications for IOL and their mode of delivery.
|
Indication |
CS |
SVD |
OVD |
Total |
|
Indication for IOL |
CS |
SVD |
OVD |
|
|
SROM |
32 (30.5%) |
38 (36.2%) |
35 (33.3%) |
105 |
|
Postdates |
32 (40%) |
25 (31.2%) |
23 (28.8%) |
80 |
|
GDM |
25 (46.3%) |
18 (33.3%) |
11 (20.4%) |
54 |
|
Fetal concerns |
18 (37.5%) |
17 (35.4%) |
13 (27.1%) |
48 |
|
IUGR |
7 (17.9%) |
18 (46.2%) |
14 (35.9%) |
39 |
|
PIH/PET |
19 (52.8%) |
9 (25%) |
8 (22.2%) |
36 |
|
Miscellaneous factors |
13 (39.4%) |
11 (33.3%) |
9 (27.3%) |
33 |
|
LFD |
8 (57.2%) |
3 (21.4%) |
3 (21.4%) |
14 |
4. Discussion
Elective birth is recommended at or near term in women with either GDM or pre-existing diabetes mellitus. The rationale for this includes a reduction in perinatal complications secondary to fetal macrosomia [7], which is associated with prolonged labour, perineal trauma, emergency CS, fetal complications of hypoxic injury and shoulder dystocia. This group also carries risks of polyhydramnios and intrauterine fetal death [8, 9] and comprised 19% of our population: they all had GDM and were managed in the joint obstetric/ endocrine clinics. Depending on diabetic control they were managed with diet and lifestyle advice or metformin, with or without insulin. The patients underwent serial growth scans at 28, 32 and 36 weeks. Induction was usually jointly decided based on their diabetic control and fetal growth [10]. As per our hospital guidelines, women with GDM without metabolic, fetal or maternal complications are offered induction of labour at 40+4 weeks and otherwise, induction is scheduled at 38+4 weeks. The rate of vaginal delivery was 53.7% in this group
Hypertensive disorders, PIH and PET complicate 10 – 15% of pregnancies at term [11]: the definitive treatment is delivery as there is a risk of IUGR, intrauterine fetal death, HELLP syndrome and eclampsia [12]. In our population 6/100 women were induced due to PIH/PET between 36 and 39+6 weeks and the CS rate was 52.8%. They were all primigravida with a Bishop score of 0 to 1. To avoid the trauma of failed induction and prolonged hospital stay CS should be at least discussed with a primigravida with an unfavorable cervix, as the risk of CS is very high in any case. Term pregnancy is 37 weeks duration. There is an increasing risk of stillbirth with advancing gestation, particularly beyond 40 and 41 weeks [13]. Pregnancy is termed as prolonged after 41 weeks and post term at 42 weeks. There are no reliable tests for fetal well-being in this situation and doppler blood flow, biophysical scoring and cardiotocography have all been shown not to be of value [14]. There are different policies regarding management of post term pregnancies across Europe [15, 16]. Our practice is induction between 40+10 days and 42 weeks in the absence of risk factors. Randomised controlled trials have shown that IOL at >40 weeks was associated with fewer neonatal deaths, neonatal intensive care unit (NICU) admissions and low Apgar score but the number needed to treat to prevent one perinatal death was 4262.
Induction for SROM at or above 37 completed weeks is associated with reduction in chorioamniotis, maternal sepsis and NICU admissions [17]. About 60 percent of women labour spontaneously within 24 hours of SROM; they should be advised about the 1% risk of serious neonatal infection compared to 0.5% with intact membranes, if labour did not commence [18]. As per hospital policy, once the diagnosis is confirmed these patients are commenced on prophylactic antibiotics 18hrs after SROM and labour is induced at 24 hrs. CS rate in this group was 30.5%. Our suspected macrosomia group constituted fourteen women. Induction was planned between 37 to 40 weeks depending on Bishop score. The aim was to reduce the risk of instrumental birth, birth injuries, shoulder dystocia, obstetrical anal sphincter injuries in mothers with suspected macrosomia [19] and induction resulted in a CS rate of 57.2%. No birth weight in this group was above 4.5 kg, the heaviest baby was 4.2 kg. Analysis of non-randomised studies by Sanchez- Ramos et al indicates that risk of CS may be increased when IOL is undertaken for suspected macrosomia [20]. The value of ultrasound in late pregnancy in this situation is questionable, particularly when the outcome for intervention is so poor.
We are the first hospital in Ireland to use the customised
growth assessment protocol (GAP) to detect Small for Gestational Age (SGA) babies- i.e., birth weight less than the 10th percentile [21]. Screening for SGA is challenging as Symphysiofundal Height (SFH) and growth ultrasound fail to reliably detect SGA [22]. Growth charts are customised individually for every patient depending on height, weight, ethnicity and parity at the booking visit. Various studies have shown its sensitivity and use as a reliable indicator for detecting in-utero SGA babies [23, 24]. A single centre study in 2018 showed that IOL at 37 weeks in cases of suspected fetal compromise is associated with lower stillbirth and neonatal death rates (p < .001), higher 1 and 5 min Apgar scores and a higher vaginal birth rate [25]. According to RCOG recommendations, SGA fetus should be offered delivery at 37 weeks’ gestation [26]. In our study 39 women were diagnosed to have SGA/IUGR fetus and were induced between 37 and 38 weeks. 82.1% of these patients delivered vaginally. Advanced maternal age is a risk factor for adverse perinatal outcome, and induction is usually considered at 40 weeks to reduce the risk of stillbirth. A retrospective cohort study by Knight et, showed that IOL at 40 weeks in women over 35 years in absence of any comorbidities, was associated with a lower risk of in-hospital perinatal death and meconium aspiration syndrome. The number needed to treat analysis indicated that 562 women would require IOL at 40 weeks to prevent one perinatal death [27]. Women requesting IOL at 40 weeks or after, in absence of any medical indication justify an intervention once the patient understands the pros and cons of the IOL procedure. There is evidence to support no increased risk of CS or other serious complications if patients are induced for reasons thought not to be medically justified by medical professionals [28]. Women presenting with reduced fetal movements at term are at increased risk of stillbirth or fetal growth restriction [29]. In our study group, 17 patients were induced for reduced fetal movements at 39 to 40 weeks. 7/14 (41.2%) patients with RFM had CS.
5. Conclusion
Mode of delivery was affected by indication of induction, which is evident from CS rate in this study group (37.6%). Suspected macrosomia is the group with highest CS rate (57.2%), followed by hypertensive disorders in pregnancy. A sensible approach should be used in patients undergoing induction of labour for suspected macrosomia, with particular attention to Bishop’s score. Caesarean delivery is a major surgery with adverse risks to mother both in her current and subsequent pregnancies. Maternal demographic factors like obesity (BMI >30), advanced birth weeks, nulliparity and poor cervical assessment are correlated independently with risk of CS [30]. In lieu of above-mentioned data, a planned CS when considering IOL for indications like hypertensive disorders of pregnancy can be justifiable in presence of secondary risk factors to avoid the trauma and prolonged hospitalization resulting from failed induction.
Conflict of Interest
There is no potential conflict of interest related to this article.
Patients’ Consent
Consent for the participation in study was not obtained from patients as data was collected from medical record without disclosing patient’s identity.
Authors Contribution
JK: Data collection, principal investigator, lead author, reviewing, writing and submitting manuscript.
AM: Statistical analysis.
MM: Study design, editing and reviewing of final draft.
References
- Wise J. Alarming global rise in caesarean births, figures show. BMJ 363 ( 2018): k4319.
- Coates D, Makris A, Catling C, et al. A systematic scoping review of clinical indications for induction of labour. PLoS One 15 (2020).
- Swarnamani K, Davies-Tuck M, Wallace E, et al. double-blind randomized Placebo-controlled trial of melatonin as an adjuvant agent in induction of labour (MILO): a study protocol. BMJ Open 10 (2020).
- Gibbons L, Belizanl JM, Lauer JA, et al. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. World health report 30 (2010): 1-31.
- Liu S, Liston Robert M, Joseph KS, et al. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. Canadian Medical Association Journal 176 (2007): 455-460.
- Macfarlane A, Blondel B, Mohangoo A, et al. Wide differences in mode of delivery within Europe: risk-stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG 123 (2016): 559-568.
- Brudenell M, Doddridge M. Delivering the infant. In: Lind T editor(s). Current Reviews in Obstetrics and Gynaecology. Diabetic Pregnancy. New York: Churchill Livingstone 13 (1989).
- Diabetes in pregnancy- management from preconception to the postnatal period. NICE guideline No 3. (2015)
- Management of Diabetes .Scottish Intercollegiate Guidelines Network (SIGN) (2010).
- Guidelines for the Management of Pre-gestational and Gestational Diabetes Mellitus from Pre-conception to the Postnatal Period. Health Service Executive (2010).
- Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol 102 (2003): 181-192.
- Management of hypertension in pregnancy. Clinical practice guideline. RCPI May (2016).
- Rosenstein MG, Cheng YW, Snowden JM, et al. Risk of stillbirth and infant death stratified by gestational age. Obstet Gynecol 120 (2012): 76-82.
- Galal M, Symonds I, Murray H, et al. Postterm pregnancy. Facts Views Vis Obgyn 4 (2012): 175-187.
- Vayssière C, Haumonte JB, Chantry A, et al. Prolonged and post-term pregnancies: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol 169 (2013): 10-16.
- Zeitlin J, Blondel B, Alexander S, et al. Variation in rates of postterm birth in Europe: reality or artefact?. BJOG 114 (2007): 1097-1103.
- Tran SH, Cheng YW, Kaimal AJ, et al. Length of rupture of membranes in the setting of premature rupture of membranes at term and infectious maternal morbidity. Am J Obstet Gynecol 198 (2008).
- Intrapartum care. NICE clinical guideline No. 190. Royal College of Obstetricians & Gynaecoloists (2014).
- Moldeus K, Cheng YW, Wikstrom A K, et al. Induction of labor versus expectant management of large-for-gestational-age infants in nulliparous women. PloS one 12 (2017).
- Sanchez-Ramos L, Bernstein S, Kaunitz AM. Expectant management versus labor induction for suspected fetal macrosomia: a systematic review. Obstetrics and Gynecology 100 (2002): 997-1002.
- Deegan N, Milne G, O’Coigligh S, et al .Introduction of A Growth Assessment Protocol “Gap-Customized Growth Chart” For The First Time In The Republic of Ireland; Preliminary Results. Fourth Irish Congress of Obstetrics, Gynaecology & Perinatal Medicine (2017).
- Hargreaves K, Cameron M, Edwards H, et al. Is the use of symphysis-fundal height measurement and ultrasound examination effective in detecting small or large fetuses?. Journal of Obstetrics and Gynaecology 31 (2011): 380-383.
- Roex A, Nikpoor P, van Eerd E, et al. Serial plotting on customised fundal height charts results in doubling of the antenatal detection of small for gestational age fetuses in nulliparous women. Aust N Z J Obstet Gynaecol 52 (2012): 78-82.
- Jayawardena L, Sheehan P . Introduction of a customised growth chart protocol increased detection of small for gestational age pregnancies in a tertiary Melbourne hospital. Aust N Z J Obstet Gynaecol 59 (2019): 493-500.
- Rabinovich A, Tsemach T, Novack L, et al. Late preterm and early term: when to induce a growth restricted fetus? A population-based study. Journal of Maternal-Fetal & Neonatal Medicine 31 (2018): 926-932.
- Investigation and management of small for gestational age foetus. Green top guideline No 31 (2014).
- Knight HE, Cromwell DA, Gurol-Urganci I, et al. Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study. PLoS Med 14 (2017) .
- Bircher C, Shepstone L, Yushchenko I, et al. Induction of Labour for Maternal Request: An Observational Study of Maternal and Fetal Outcomes. Rev Recent Clin Trial 9 (2014): 91-95.
- Holm Tveit JV, Saastad E, Stray-Pedersen B, et al. Maternal characteristics and pregnancy outcomes in women presenting with decreased fetal movements in late pregnancy. Acta Obstet Gynecol Scand 88 (2009): 1345-1351
- Giugliano E, Cagnazzo E, Milillo V, et al. The risk factors for failure of labor induction: a cohort study. J Obstet Gynaecol India 64 (2014): 111-115.
