Hepatocellular Carcinoma with An Uncertain Diagnosis in A 40-Year-Old Sudanese Patient from An Untreated Diagnosis to Tuberculosis Is Treated
Article Information
Fadi M. Toum Ahmed1, Mogahid Alteib Yousif Alteib2*, Osman Asim Babker3
1Internal Medicine Specialist, Sinnar, University, Sennar, Sudan
2House officer, sinnar teaching hospital, Sinnar, University, Sennar, Sudan
3Medical student, Sinnar, University, Sennar, Sudan
*Corresponding Author: Mogahid Alteib Yousif Alteib, House officer, sinnar teaching hospital, Sinnar, University, Sennar, Sudan
Received: 16 November 2023; Accepted: 11 December 2023; Published: 29 December 2023
Citation: Fadi M. Toum Ahmed, Mogahid Alteib Yousif Alteib, Osman Asim Babker. Hepatocellular Carcinoma with An Uncertain Diagnosis in A 40-Year-Old Sudanese Patient from An Untreated Diagnosis to Tuberculosis Is Treated. Archives of Clinical and Medical Case Reports. 7 (2023): 448-452.
Share at FacebookAbstract
We report a case of 40 years old male retired farmer. Was diagnosed with portal hypertension due to prehepatic fibrosis and esophageal varices bleeding had chronic liver disease due to schistosomiasis and spontaneous bacterial peritonitis 8 years ago. presented complaints of small bowel chronic diarrhea, weight loss, progressive Shortness of breath low-grade fever complicated by an infection he had a history of jaundice and chronic anemia. Not smokers or adapted to drinking alcohol. On physical examination, the patient looked very ill and emaciated, Pale not jaundiced or cyanosed, Cervical lymph node was enlarged and small, and the Finger clipping grade 4 Features of Chronic liver disease. On chest examination, there is bronchial breathing bilaterally at middle zones with fine end-inspiratory crepitation, Course crepitation at base bilateral and Loud S2. Scaphoid abdomen with Splenomegaly 16 cm Blow costal margin, Liver span 8 cm, No ascites, PR not done. The first report found hepatocellular cancer, and the second report revealed this persistent metastasis in our patient with chronic liver disease, which first presents on an initial ultrasound and which we then diagnose with an abdominal CT scan. The liver tissue acquired from a liver biopsy is then used to make the histological and/or bacteriological diagnosis of extrapulmonary TB, which can be very challenging to do. Sometimes, a patient's full recovery from a particular therapy is required before a clinical diagnosis can be confirmed [6]. After the patient had recovered from anti-tuberculosis treatment, histology showed granulomatous liver TB, ruling out HCC and Mets, and visual inspection reveals cervical lymph node enlargement.
Keywords
Hepatocellular carcinoma; Tuberculosis; Sudanese
Hepatocellular carcinoma articles; Tuberculosis articles; Sudanese articles
Hepatocellular carcinoma articles Hepatocellular carcinoma Research articles Hepatocellular carcinoma review articles Hepatocellular carcinoma PubMed articles Hepatocellular carcinoma PubMed Central articles Hepatocellular carcinoma 2023 articles Hepatocellular carcinoma 2024 articles Hepatocellular carcinoma Scopus articles Hepatocellular carcinoma impact factor journals Hepatocellular carcinoma Scopus journals Hepatocellular carcinoma PubMed journals Hepatocellular carcinoma medical journals Hepatocellular carcinoma free journals Hepatocellular carcinoma best journals Hepatocellular carcinoma top journals Hepatocellular carcinoma free medical journals Hepatocellular carcinoma famous journals Hepatocellular carcinoma Google Scholar indexed journals carcinoma articles carcinoma Research articles carcinoma review articles carcinoma PubMed articles carcinoma PubMed Central articles carcinoma 2023 articles carcinoma 2024 articles carcinoma Scopus articles carcinoma impact factor journals carcinoma Scopus journals carcinoma PubMed journals carcinoma medical journals carcinoma free journals carcinoma best journals carcinoma top journals carcinoma free medical journals carcinoma famous journals carcinoma Google Scholar indexed journals Tuberculosis articles Tuberculosis Research articles Tuberculosis review articles Tuberculosis PubMed articles Tuberculosis PubMed Central articles Tuberculosis 2023 articles Tuberculosis 2024 articles Tuberculosis Scopus articles Tuberculosis impact factor journals Tuberculosis Scopus journals Tuberculosis PubMed journals Tuberculosis medical journals Tuberculosis free journals Tuberculosis best journals Tuberculosis top journals Tuberculosis free medical journals Tuberculosis famous journals Tuberculosis Google Scholar indexed journals Sudanese articles Sudanese Research articles Sudanese review articles Sudanese PubMed articles Sudanese PubMed Central articles Sudanese 2023 articles Sudanese 2024 articles Sudanese Scopus articles Sudanese impact factor journals Sudanese Scopus journals Sudanese PubMed journals Sudanese medical journals Sudanese free journals Sudanese best journals Sudanese top journals Sudanese free medical journals Sudanese famous journals Sudanese Google Scholar indexed journals Ventricular articles Ventricular Research articles Ventricular review articles Ventricular PubMed articles Ventricular PubMed Central articles Ventricular 2023 articles Ventricular 2024 articles Ventricular Scopus articles Ventricular impact factor journals Ventricular Scopus journals Ventricular PubMed journals Ventricular medical journals Ventricular free journals Ventricular best journals Ventricular top journals Ventricular free medical journals Ventricular famous journals Ventricular Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Diagnosis articles Diagnosis Research articles Diagnosis review articles Diagnosis PubMed articles Diagnosis PubMed Central articles Diagnosis 2023 articles Diagnosis 2024 articles Diagnosis Scopus articles Diagnosis impact factor journals Diagnosis Scopus journals Diagnosis PubMed journals Diagnosis medical journals Diagnosis free journals Diagnosis best journals Diagnosis top journals Diagnosis free medical journals Diagnosis famous journals Diagnosis Google Scholar indexed journals epithelium articles epithelium Research articles epithelium review articles epithelium PubMed articles epithelium PubMed Central articles epithelium 2023 articles epithelium 2024 articles epithelium Scopus articles epithelium impact factor journals epithelium Scopus journals epithelium PubMed journals epithelium medical journals epithelium free journals epithelium best journals epithelium top journals epithelium free medical journals epithelium famous journals epithelium Google Scholar indexed journals
Article Details
1. Introduction
A significant side effect of liver illness, portal hypertension is brought on by several clinical diseases that make the portal blood flow into the liver more difficult. Due to significant structural changes brought on by fibrosis and increased vascular tone in the hepatic microcirculation, cirrhosis is characterized by portal hypertension, which is primarily caused by an increase in intrahepatic vascular resistance. Collateral vessel development and arterial vasodilation advance with the onset of portal hypertension, increasing blood flow to the portal circulation. Esophageal varices or ascites may eventually result from the hyperdynamic circulatory condition [1]. In individuals with cirrhosis who present with a variety of symptoms, spontaneous bacterial peritonitis (SBP) is a prevalent and usually deadly bacterial infection of the ascites. As there is no intra-abdominal source of infection or inflammatory process, the diagnosis is determined in the absence of subsequent peritonitis. More study has identified cause variables including the transfer of gut bacteria to lymph nodes, making the etiology less mysterious. SBP occurs in cirrhotic individuals with a variety of etiologies, not only alcohol, and later research has shown causing factors like this. Sodium and water retention and fluid overflow into the peritoneal cavity is caused by portal hypertension, splanchnic vasodilation, and activation of the renin-angiotensin cascade [2]. In both primary care settings and specialty gastrointestinal clinics, chronic diarrhea is a common presenting complaint. Chronic diarrhea is believed to affect more than 5% of the world's population. While there are many causes of chronic diarrhea, the degradation of intestinal barrier function, dysbiosis, and mucosal micro-inflammation are now recognized as underlying factors in several chronic diarrheal illnesses [3]. The most typical cause of anemia in patients who are hospitalized is anemia of chronic disease (ACD) or anemia of chronic inflammation. The ACD is only present in individuals whose current disease triggers an active immune/inflammatory response that reduces iron absorption at many locations, not in patients whose sickness or its treatment directly produces anemia, as is the case with some cancers and the use of cytotoxic medications [4]. Numerous recurrent bacterial and fungal infections affect patients with chronic granulomatous disease (CGD). The lungs, digestive tract, and skin, as well as the lymph nodes that drain these structures, are the organs most frequently affected by these infections. A large number of other organs, most notably the liver, bones, kidneys, and brain, can be harmed due to the infection's potential to spread hematogenous (through the blood) and contiguously (by touch) within an individual [5]. Diagnosing tuberculosis (TB) can be challenging because of its diverse clinical presentation. As a result of the lymphohematogenous spread of Mycobacterium tuberculosis, disseminated tuberculosis (TB) is characterized by the presence of two or more noncontiguous locations. One-fifth of all TB cases 2 contain extrapulmonary involvement, which can happen even in the absence of radiological or histological signs of pulmonary infection. Hepatic tuberculosis is uncommon3 and can develop as a primary case or as a result of an old tubercular focus becoming active, especially in the absence of miliary TB. Due to the clinical signs' general nature and the fact that they can resemble several other disorders, diagnosis can be challenging. ultimately end with fulminant hepatic failure, which might be deadly. The liver tissue collected by liver biopsy is used to determine the histological and/or bacteriological diagnosis of extra pulmonary TB, which can be highly challenging. On occasion, a clinical diagnosis is only established following a full recovery from a particular treatment [6].
2. Patient Information
Our patient is a male farmer who has retired at the age of 40. was identified as having portal HTN eight years ago as a result of PPF and an OV bleeder. The patient who arrived complained of chronic diarrhea for the last seven months. There was a lot of bouncing diarrhea that frequently roused the patient from sleep and had a yellow-brown color that wasn't unpleasant or filled with blood or mucous. It is not worsened by any variables and is responding to therapy. No other notable GIT symptoms were present. In addition to losing weight With perspiration but no rigidity, the condition linked with a low-grade fever on/off was seen to manifest in the afternoon and at night. Since four months ago, the patient has experienced a progressive S.O.B. that gets worse with moderate exertion and gets worse with mild exertion along with a dry cough but no orthopnea, Paroxysmal Nocturnal dyspnea, chest pain, syncopal attack, or lower limb weakness. Four days before admission, when the cough turned productive and the temperature rose along with S.O.B. at rest, the situation deteriorated. Other systems were unremarkable in history.
Regarding his past medical history, the patient had been suffering from a long history of recurrent hospital admissions and blood transfusions due to anemia of recurrent attacks of anemia of chronic disease and schistosome, their history of chronic liver disease Spontaneous Bacterial Peritonitis more than 7 months of recurrent endoscopes, jaundice 4months ago, No history of operations, No history of DM, HTN or others. Regarding social history Patient was a farmer who retired since his illness depends physically and financially on his family, is married, has Health insurance, and is not a smoker or alcohol user family history is unremarkable. Investigations were done to reach the diagnosis as I will describe below, his drug history is Not known allergic to any medications known by the patient or family, On norfloxacin, spironolactone, propranolol, pantoprazole, folic acid, and hemoglobin.
3. Examination
The patient had a very ill and emaciated appearance, was pale without being jaundiced or cyanosed, had an enlarged and small cervical lymph node, had finger clipping grade 4, and had symptoms of chronic liver illness. His cardiopulmonary examination showed bilateral middle zone bronchial breathing with fine end-inspiratory crepitation, course crepitation at the base, loud S2, scaphoid abdomen upon inspection, their splenomegaly 16 cm B.C.M., 8 cm liver span, No ascites, and no PR. On examination, other systems were clear. The patient had a very ill and emaciated appearance, was pale without being jaundiced or cyanosed, had an enlarged and small cervical lymph node, had finger clipping grade 4, and had symptoms of chronic liver illness. His cardiopulmonary examination showed bilateral middle zone bronchial breathing with fine end-inspiratory crepitation, course crepitation at the base, loud S2, scaphoid abdomen upon inspection, their splenomegaly 16 cm B.C.M., 8 cm liver span, No ascites, and no PR. On examination, other systems were clear.
The patient had a very ill and emaciated appearance, was pale without being jaundiced or cyanosed, had an enlarged and small cervical lymph node, had finger clipping grade 4, and had symptoms of chronic liver illness. His cardiopulmonary examination showed bilateral middle zone bronchial breathing with fine end-inspiratory crepitation, course crepitation at the base, loud S2, scaphoid abdomen upon inspection, their splenomegaly 16 cm B.C.M., 8 cm liver span, No ascites, and no PR. On examination, other systems were clear.

Figure 1: Hand and foot patient picture, he had features of finger clubbing grade 4.

Figure 2: Shows features of scaphoid abdomen and splenomegaly 16 cm B.C.M.
4. Investigation
On presentation, his blood test showed hemoglobin =9.2, mean corpuscular volume =73 f l, platelets =238*10 *3/Cm, and WBCs=5000*10*3. INR;1.1, ESR:90, the viral screen was negative, INR;1.1, acid-fast bacilli;5, stool; blood and pus cell, renal function test and electrolytes, blood urea in day one;31, day three;45, day seven;27. Albumin at day one;2, day three;2.6, other renal function and electrolytes were normal, LFT; AST;20 at day one, at day three AST was 23, ALP at day1;2781, day3;459, ALT at day 1 and 7; was normal .no malaria parasites have been seen in the blood film, HB at day 7; was 8.8. abdomen U\S; no feature of chronic liver disease, and there is splenomegaly and there is cirrhotic liver focal lesion. Chest X-ray showed features suggesting lung fibrosis involving reticular regular shadowing bilateral at the base of the lung. Chest CT scan showed reticular and nodular and grand gland appearance also suggesting lung fibrosis. abdomen CT showed two reports the first one showed a feature suggesting hepatocellular carcinoma, and the second report show a feature suggesting metastasis. Osephego-Gastroduodenoscopy showed grade 4 esophageal varices. histopathology showed granulomas lymphadenopathy which confirms tuberculosis, a colonoscopy was not done.
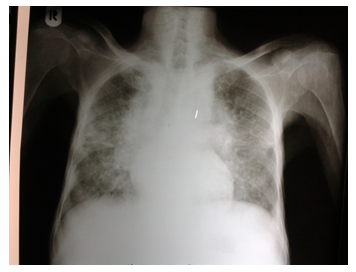
Figure 3: Chest x-ray showing feature suggesting lung fibrosis involving reticular regular shadowing bilateral at the base of the lung.
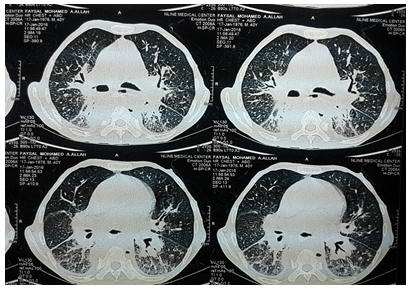
Figure 4: Chest CT scan showing reticular and nodular and grand gland appearance also suggesting lung fibrosis.
5. Treatment and Follow-Up
Our Patients have chronic liver disease he does not receive pyrazinamide because it's hepatotoxic. But he received Isoniazid and rifampicin plus two non-hepatoxic drugs such as streptomycin and ethambutol used for eight months.
We flowed the patient after weeks he start anti-tuberculous drugs patient improved and gain weight 1st follow-up his weight was 50 kg and then became 55 kg.
6. Discussion
According to an inquiry, clinical assessment, and examination, a man may have periportal fibrosis portal hypertension caused by Schistosoma, which would explain his lung fibrosis and increase his spleen. Several clinical conditions that impede the flow of blood into the liver through the portal vein lead to portal hypertension. Cirrhosis is characterized by portal hypertension, which is largely brought on by an increase in intrahepatic vascular resistance, due to the major structural changes brought on by fibrosis and increased vascular tone in the hepatic microcirculation [1]. In our patient with chronic liver illness, which initially manifests on an initial ultrasound, following which we do an abdominal CT scan, the first report revealed hepatocellular carcinoma and the second revealed this persistent metastasis. The histological and/or bacteriological diagnosis of extrapulmonary TB, which can be very difficult to make, is made using the liver tissue obtained via liver biopsy. On occasion, a clinical diagnosis is only confirmed after a specific treatment has allowed the patient to fully recover [6]. After histology reveals granulomatous liver TB, which rules out HCC and Mets after the patient underwent anti-tuberculous treatment improvement, there is cervical lymph node enlargement on inspection. Spontaneous bacterial peritonitis (SBP) is a common and typically fatal ascites bacterial infection seen in cirrhotic patients who exhibit a range of symptoms. The absence of subsequent peritonitis allows for the diagnosis to be made since there is no intra-abdominal source of infection or inflammatory process. The pathogenesis is less mysterious now that more research has shown contributing factors, including the spread of gut bacteria to lymph nodes. Later studies have revealed causes like these for SBP in cirrhotic patients, which has several etiologies other than alcohol. Portal hypertension, splanchnic vasodilation, and renin-angiotensin cascade activation are the three factors that lead to sodium and water retention as well as a fluid overflow into the peritoneal cavity [2]. After receiving therapy for a diagnosis of bacterial peritonitis that was previously made by experts, we investigated the case and determined that it was granulomatous TB after histology confirmed it. Anemia of chronic disease (ACD) or anemia of chronic inflammation is the most common cause of anemia in individuals who are hospitalized. ACD is not found in patients whose illness or its treatment directly causes anemia, as is the case with some cancers and the use of cytotoxic drugs, but only in those whose current disease causes an active immune/inflammatory response that reduces iron absorption at many locations [4]. In our situation, the patient has a history of many hospitalizations, and while the first test indicated low levels of hemoglobin after the patient received treatment, the levels of hemoglobin increased, confirming the presence of a chronic condition.
7. Conclusion
A patient from Sudan who is a 40-year-old retired farmer faces difficulty in being diagnosed with granulomatous liver disease. 8 years ago, I was identified as having chronic liver disease brought on by schistosomiasis and spontaneous bacterial peritonitis, as well as portal hypertension brought on by prehepatic fibrosis and esophageal varices hemorrhage. Small intestine persistent diarrhea, weight loss, gradual shortness of breath, low-grade fever aggravated by an infection, and he had a history of jaundice and chronic anemia were among his problems. not alcoholic drinkers or smokers. The patient seemed very unwell and malnourished upon physical examination. They were pale and neither jaundiced nor cyanosed. The finger clipping was grade 4 and the cervical lymph node was swollen and tiny. hepatic illness with a chronic course. On a chest exam, there is bilateral middle zone bronchial breathing with fine end-inspiratory crepitation, bilateral course crepitation at the base, and loud S2. 16 cm Blow costal border and a scaphoid abdomen 8 cm for liver span No ascites, no PR, and after a thorough study that included laboratory tests, imaging studies, histology, and according to case presentations, we identified the patient's condition as granulomatous liver disease. The patient was then given an antitubercular medication, and their condition improved.
It’s challenging to diagnose granulomatous liver disease, in a patient from Sudan who is 40 years old male retired farmer. Was diagnosed with portal hypertension due to prehepatic fibrosis and esophageal varices bleeding had chronic liver disease due to schistosomiasis and spontaneous bacterial peritonitis 8 years ago. presented complaints of small bowel chronic diarrhea, weight loss, progressive Shortness of breath low-grade fever complicated by an infection he had a history of jaundice and chronic anemia. Not smokers or adapted to drinking alcohol. On physical examination, the patient looked very ill emaciated, Pale not jaundiced or cyanosed, Cervical lymph node enlarged and small, Finger clubbing grade 4 Features of Chronic liver disease. On chest examination, there is bronchial breathing bilaterally at middle zones with fine end-inspiratory crepitation, Course crepitation at base bilateral, and Loud S2. Scaphoid abdomen with Splenomegaly 16 cm Blow costal margin, Liver span 8 cm, No ascites, PR not done, after the serial investigation done, laboratory and imaging, and histopathology and according to case presentation we diagnosed as granulated liver disease and the patient received anti-tuberculous drugs and the patient improved.
Ethical Approval and Consent to Participate
The protocol of this study was approved (No: 25-22) on 23rd of July, 2022 by the Institutional Review Board of the Faculty of Medicine, University of Gezira, Wad Medani, Sudan.
We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Before filling out the questionnaire, each participant provided written informed consent. Participants were assured about the confidentiality of any obtained information. The responses were kept confidentially and data from this research was managed only researchers in this study, Results will be used only for research and data cannot be traced back to their original sources.
Consent to Publication
Not applicable.
Availability of Data and Materials
The data set used and/or analyses during the case study are available from the corresponding author on reasonable request.
Conflict of Interest
Authors declared no competing of interest.
Funding
The study was self-funded.
Contribution Statement
F.M.T.A: Conceptualization, Data Creation, Investigation, Supervision, Formal analysis, writing the original draft.
M.A.Y.A: Conceptualization Data creation, Methodology, investigation, Writing the original draft.
O.A.B: Formal analysis, Writing the original draft.
References
- Iwakiri Y. Pathophysiology of portal hypertension. Clin Liver Dis 18 (2014): 281-291.
- Dever JB, Sheikh MY. Review article: Spontaneous bacterial peritonitis-bacteriology, diagnosis, treatment, risk factors, and prevention. Aliment Pharmacol Ther 41 (2015): 1116-1131.
- Alonso-Cotoner C, Abril-Gil M, Albert-Bayo M, et al. The Role of Purported Mucoprotectants in Dealing with Irritable Bowel Syndrome, Functional Diarrhea, and Other Chronic Diarrheal Disorders in Adults. Adv Ther 38 (2021): 2054-2076.
- Madu AJ, Ughasoro MD. Anaemia of Chronic Disease: An In-Depth Review. Med Princ Pract 26 (2017): 1-9.
- Roos Di. Chronic granulomatous disease. Br Med Bull 118 (2016): 50-63.
- Ribeiro S, Trabulo D, Cardoso C, et al. Tuberculose Disseminada num Doente Imunocompetente: A Resposta Está no Fígado. GE Port J Gastroenterol 23 (2016): 208-213.
