Healthcare Practitioners’ Views of their Role in Addressing the Medical Comorbidites of People with Mental Illness
Article Information
Monica Zolezzi1*, Sara Abdulrhim2, Nour Isleem3, Farah Zahrah4, Yassin Eltorki5
1Assistant Professor, Clinical Pharmacy and Practice, College of Pharmacy, QU Health, Qatar University
2MSc Student, Clinical Pharmacy and Pharmacy Practice, College of Pharmacy, Qatar University
3Clinical Pharmacy Specialist, Women Wellness and Research Center, Hamad Medical Corporation, Doha, Qatar 4Clinical Pharmacist, Al Wakrah Hospital, Hamad Medical Corporation, Doha, Qatar
5Clinical Pharmacy Specialist, Mental Health Hospital, Hamad Medical Corporation, Doha, Qatar
*Corresponding Author: Monica Zolezzi, Clinical Pharmacy and Practice, College of Pharmacy, QU Health, Qatar University, Doha, Qatar
Received: 27 January 2020; Accepted: 05 February 2020; Published: 06 March 2020
Citation:
Monica Zolezzi, Sara Abdulrhim, Nour Isleem, Farah Zahrah, Yassin Eltorki. Healthcare practitioners’ views of their role in addressing the medical comorbidites of people with mental illness. Journal of Psychiatry and Psychiatric Disorders 4 (2020): 31-44.
Share at FacebookAbstract
Objectives: To explore the views and experiences of different healthcare professionals in Qatar about their role addressing the medical comorbidities of people with serious mental illness (SMI).
Subjects and Methods: Qualitative study using a purposive sampling strategy to include representative viewpoints from physicians, pharmacists, and nurses working at outpatient settings throughout Doha, Qatar. Semi-structured interviews were conducted, and transcripts analyzed employing qualitative phenomenological approach to inquiry.
Results: A total of eighteen interviews to healthcare practitioners (HCPs) were conducted. Four major common themes emerged from these interviews, including: 1) knowledge and awareness about the medical comorbidities among people with serious mental illness (SMI); 2) perceptions of current practice in relation to addressing the medical comorbidities of people with SMI; 3) perceived barriers to the provision of medical care to people with SMI; 4) possible solutions to address the barriers identified.
Conclusion: Results of this study suggest that HCPs perceive that people with SMI in Qatar receive suboptimal standard levels of care for their medical comorbidities. The integration of medical and mental healthcare services and fostering shared responsibility that includes family members were strongly recommended to improve the physical health of people with SMI.
Keywords
Mental illness; Medical comorbidities; Health care practitioners’ views
Mental illness articles, Medical comorbidities articles, Health care practitioners views articles
Mental illness articles Mental illness Research articles Mental illness review articles Mental illness PubMed articles Mental illness PubMed Central articles Mental illness 2023 articles Mental illness 2024 articles Mental illness Scopus articles Mental illness impact factor journals Mental illness Scopus journals Mental illness PubMed journals Mental illness medical journals Mental illness free journals Mental illness best journals Mental illness top journals Mental illness free medical journals Mental illness famous journals Mental illness Google Scholar indexed journals Medical comorbidities articles Medical comorbidities Research articles Medical comorbidities review articles Medical comorbidities PubMed articles Medical comorbidities PubMed Central articles Medical comorbidities 2023 articles Medical comorbidities 2024 articles Medical comorbidities Scopus articles Medical comorbidities impact factor journals Medical comorbidities Scopus journals Medical comorbidities PubMed journals Medical comorbidities medical journals Medical comorbidities free journals Medical comorbidities best journals Medical comorbidities top journals Medical comorbidities free medical journals Medical comorbidities famous journals Medical comorbidities Google Scholar indexed journals Health care practitioners’ views articles Health care practitioners’ views Research articles Health care practitioners’ views review articles Health care practitioners’ views PubMed articles Health care practitioners’ views PubMed Central articles Health care practitioners’ views 2023 articles Health care practitioners’ views 2024 articles Health care practitioners’ views Scopus articles Health care practitioners’ views impact factor journals Health care practitioners’ views Scopus journals Health care practitioners’ views PubMed journals Health care practitioners’ views medical journals Health care practitioners’ views free journals Health care practitioners’ views best journals Health care practitioners’ views top journals Health care practitioners’ views free medical journals Health care practitioners’ views famous journals Health care practitioners’ views Google Scholar indexed journals serious mental illness articles serious mental illness Research articles serious mental illness review articles serious mental illness PubMed articles serious mental illness PubMed Central articles serious mental illness 2023 articles serious mental illness 2024 articles serious mental illness Scopus articles serious mental illness impact factor journals serious mental illness Scopus journals serious mental illness PubMed journals serious mental illness medical journals serious mental illness free journals serious mental illness best journals serious mental illness top journals serious mental illness free medical journals serious mental illness famous journals serious mental illness Google Scholar indexed journals healthcare practitioners articles healthcare practitioners Research articles healthcare practitioners review articles healthcare practitioners PubMed articles healthcare practitioners PubMed Central articles healthcare practitioners 2023 articles healthcare practitioners 2024 articles healthcare practitioners Scopus articles healthcare practitioners impact factor journals healthcare practitioners Scopus journals healthcare practitioners PubMed journals healthcare practitioners medical journals healthcare practitioners free journals healthcare practitioners best journals healthcare practitioners top journals healthcare practitioners free medical journals healthcare practitioners famous journals healthcare practitioners Google Scholar indexed journals physical illness articles physical illness Research articles physical illness review articles physical illness PubMed articles physical illness PubMed Central articles physical illness 2023 articles physical illness 2024 articles physical illness Scopus articles physical illness impact factor journals physical illness Scopus journals physical illness PubMed journals physical illness medical journals physical illness free journals physical illness best journals physical illness top journals physical illness free medical journals physical illness famous journals physical illness Google Scholar indexed journals National Mental Health Strategy articles National Mental Health Strategy Research articles National Mental Health Strategy review articles National Mental Health Strategy PubMed articles National Mental Health Strategy PubMed Central articles National Mental Health Strategy 2023 articles National Mental Health Strategy 2024 articles National Mental Health Strategy Scopus articles National Mental Health Strategy impact factor journals National Mental Health Strategy Scopus journals National Mental Health Strategy PubMed journals National Mental Health Strategy medical journals National Mental Health Strategy free journals National Mental Health Strategy best journals National Mental Health Strategy top journals National Mental Health Strategy free medical journals National Mental Health Strategy famous journals National Mental Health Strategy Google Scholar indexed journals CVD articles CVD Research articles CVD review articles CVD PubMed articles CVD PubMed Central articles CVD 2023 articles CVD 2024 articles CVD Scopus articles CVD impact factor journals CVD Scopus journals CVD PubMed journals CVD medical journals CVD free journals CVD best journals CVD top journals CVD free medical journals CVD famous journals CVD Google Scholar indexed journals Health care articles Health care Research articles Health care review articles Health care PubMed articles Health care PubMed Central articles Health care 2023 articles Health care 2024 articles Health care Scopus articles Health care impact factor journals Health care Scopus journals Health care PubMed journals Health care medical journals Health care free journals Health care best journals Health care top journals Health care free medical journals Health care famous journals Health care Google Scholar indexed journals psychology articles psychology Research articles psychology review articles psychology PubMed articles psychology PubMed Central articles psychology 2023 articles psychology 2024 articles psychology Scopus articles psychology impact factor journals psychology Scopus journals psychology PubMed journals psychology medical journals psychology free journals psychology best journals psychology top journals psychology free medical journals psychology famous journals psychology Google Scholar indexed journals
Article Details
1. Introduction
Over the past two decades, the scientific literature reporting increased morbidity and premature mortality among people with mental health conditions as a result of poor physical health is vast [1-3]. In addition to this morbidity and morbidity gap, there is also evidence of disparities in the provision of medical care to people with mental illness: they are less likely to have regular physical or diagnostic examinations, and to receive evidence-based medications for chronic medical conditions than people without mental illness [1, 4-9]. In a recently published study in Qatar, which consisted on a retrospective chart review of patients attending a psychiatric outpatient clinic, it was reported that almost 30% of patients with serious mental illness (SMI) had at least one medical comorbidity for which inadequate medical care was being provided [10]. Reasons for the gap in medical care to people with mental illness have been highlighted in several studies, including: fragmentation of care, limited access and time pressure in general practice, staff attitudes regarding what falls within their clinical role, communication difficulties between services, lack of training, inadequate access or compliance with clinical guidelines in the part of healthcare practitioners (HCPs) to support people with psychiatric comorbidity [5, 11-15].
Globally, momentum is gaining in terms of raising awareness, increasing understanding, and articulating strategies for addressing the added burden of physical illness on people with SMI as part of the health agenda. In Qatar, one of the strategies outlined by the National Mental Health Strategy (NMHS) is building multidisciplinary primary care teams [16]. These teams need to be aware of the current care gaps and be prepared to engage in the provision of evidence-based medical treatments available for people with SMI. As such, the main goal of this study was to have a better understanding of the current medical care provided to patients with SMI in Qatar from the perspectives of HCPs and to explore their views on their role in addressing the added burden of physical illness in this population, their causes, what is amenable to change and how this change might be brought about. This understanding will help building strategies for the integration of medical and mental healthcare services to fill the care gaps that have been highlighted.
2. Methods
2.1 Study design
Qualitative study using semi-structured individual interviews to explore HCPs’ views and experiences about the physical health of people with SMI. A qualitative phenomenological approach to inquiry was adopted where common themes were drawn from the essence of several HCPs lived experiences about the management of the medical comorbidities in people with SMI.
2.2 Study participants and data collection
A purposive sampling strategy was used to include representative viewpoints from physicians, pharmacists and nurses working in primary health care (including community pharmacies and primary health care clinics) and tertiary health care (e.g. hospitals) throughout Doha, Qatar. Participants were contacted in person or via e-mail and provided with a participant information sheet and consent form. The consent form was signed by the participant at the time of the face-to-face interview after discussion of the study purpose and data collection procedures.
A semi-structured interview tool was developed to guide the interviewers. The questions were designed to elicit information from participants on the following broad topics:
- Awareness of the prevalence of medical comorbidities and physical health care needs amongst people with mental illness
- Current practices within the health care system to address the medical comorbidities of people with mental illness
- Perceived barriers to the provision of physical assessments and management of the medical comorbidities in patients with mental illness
- Perceived interventions and solutions needed to address these barriers
- Perceived training needs of health care professionals to address the physical health needs and medical comorbidities of people with mental illness
Interviews were scheduled at a mutually convenient time at the HCPs’ practice site. Interviews were conducted separately by three researchers (SA, NI, or FZ), took approximately forty-five minutes to one hour to complete, and were audio-recorded. Researchers then participated in a post-interview ‘debriefing’ session with other members of the research team (MZ, YE). The interview audio recordings were transcribed verbatim and inserted into an Excel data sheet. Data collection continued until saturation of themes was reached and no new issues emerged.
2.3 Data analysis
Thematic analysis was undertaken to identify key themes emerging from the interviews, using the principles recommended by Braun and Clarke for qualitative research [17]. As illustrated in (Figure 1), the transcripts were read, ensuring accuracy by comparing transcribed content to recordings, and re-read by each researcher separately (SA, NI, or FZ) to identify key phrases that were coded as relevant to the research question. These codes were collated around categories that were collapsed into thematic material. These themes were validated and further examined by the entire research team (MZ, SA, NI, FZ, YE) to identify the synergies, points of difference and to ensure findings were not unduly influenced by a single researcher’s perspective.
2.4 Ethical approval
The study protocol was approved by the Institutional Review Board (IRB) at Qatar University (reference number: 18-060-3-016) and at Hamad Medical Corporation, Medical Research Center (reference number: 16023/16).
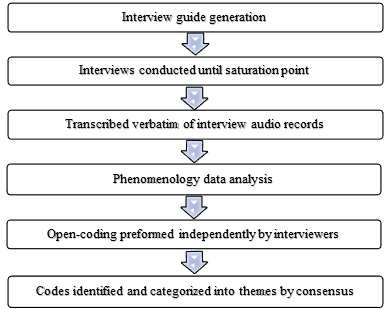
Figure 1: Qualitative data analysis process.
3. Results
Eighteen interviews were conducted to HCPs who consisted of 8 pharmacists, 4 physicians and 6 nurses. The practice sites of these HCPs were primary health care (including community pharmacies and primary health care clinics) and tertiary outpatient clinics within general and specialized mental health hospitals. All the participants had at least one year of experience providing services to people with mental illness in some capacity. Four major themes emerged from the analysis of the transcripts. These, together with the subthemes under each, are described in (Table 1).
3.1 Theme 1: HCPs’ knowledge and awareness about the medical comorbidities in people with SMI
3.1.1 Knowledge of specific medical comorbidities: Participants indicated that people with SMI are at an increased risk of specific medical comorbidities including: diabetes, CVD, hypertension, hyperthyroidism, metabolic syndrome, elevated cholesterol, obesity, poor dental health, lung problems, hepatitis, increased risk of bleeding and decreased immunity.
“It depends on the age. Young patients are mostly free [of medical comorbidities], but it also depends on the psychiatric medications they take. Old patients mostly have multiple comorbidities (diabetes and the metabolic syndrome, hypertension, obesity, bleeding, hormonal and electrolyte disturbances).” (Psychiatric nurse)
“Mostly, they have comorbidities [like diabetes] and elevated cholesterol; most of them are obese more than the general population, they have poor dental health.” (Physician)
|
Major Theme |
Subthemes |
Summary of Findings |
|
1. Knowledge and awareness |
1a. Knowledge of specific medical comorbidities 1b. Awareness of increased medical care needs 1c. Knowledge of specific tests and monitoring parameters 1d. Awareness of clinical practice guidelines |
Overall HCPs are aware about the medical comorbidities that are more prevalent in people with SMI. They are also aware of the increased medical care needs in those patients in comparison to the general population. However, HCPs apper to have limited knowledge and awareness of the physical tests required to monitor the medical comorbidities of people with SMI, and of relevant clinical practice guidelines. |
|
2. Perceptions of current practice |
2a. Patient self-awareness of wellness 2b. Responsibility for physical care 2c. Referral system 2d. Frequency of physical assessments |
An overall perception that people with mental illness do not care about their own physical health was reported. Varied opinions in regards to who is the key provider of the physical care needs in people with SMI were voiced. There was an overall perception that people with mental illness are just like other patients who need to be referred to primary health care centers when they have a medical problem. HCPs had inconsistent opinions in regards to the frequency of medical checks that people with SMI should have. |
|
3. Barriers to medical care |
3a. Patient factors 3b. Societal factors 3c. Treatment-emergent adverse effects 3d. Healthcare system |
There was an overall perception that people with SMI tend to self-treat some conditions without consulting their doctor, and that this population is non-compliant to medications, diet, or follow-up appointments. HCPs perceived there is suboptimal patient education, limited family engagement and mental health stigma that affects medical follow up of these patients. HCPs highlighted that medications to treat mental illness have side effects, such as sedation and decreased cognition, that make patients less likely to seek help. There was an overall perception that limited personnel in mental health hospitals is available to address the medical problems of these patients. There is also appointment scheduling and capacity problems to monitor outpatients with SMI. |
|
4. Solutions to barriers |
4a. Shared responsibility 4b. Patient and family education 4c. Staff education and training |
Caring for the physical health of psychiatric patients was predominantly voiced as being a shared responsibility among the different HCPs, and that it must involve educating patients and their families about the disease and the likely comorbidities. HCPs believe there is need for more education on how to address the medical comorbidities in patients with mental illness through continuing education programs, distribution of clinical practice guidelines, and on-site awareness campaigns. |
HCPs=Healthcare practitioners, SMI=Serious mental illness
Table 1: Themes derived from healthcare practitioners’ interviews.
3.1.2 Awareness of increased medical care needs: Participants indicated that people with SMI are at an increased need for screening and monitoring primarily due to emergent medication-induced effects that put them at increased risk of medical complications. They also indicated that this might be due to limited non-pharmacological interventions in this population or non-compliance to diet or exercise advice.
“Uncontrolled comorbid conditions may lead to increased mortality, so need to monitor, specially medications that cause weight gain” (Community Pharmacist)
“The diet of the patients is very poor; most of the patients are not compliant to the diet recommended by the physician” (Nurse)
3.1.3 Awareness of specific tests and screening needed to be monitored: Participants mentioned a variety of physical tests and screening parameters that should be measured or monitored in people with SMI in order to assess for emergent physical comorbidities. Specific monitoring/screening tests that were highlighted included: x-ray, full blood count, dental check, weight, body mass index, thyroid function, creatinine kinase, and troponin.
“CBC, electrolyte, renal function, liver function, lipid profile, vitamin D, B12, and thyroid function test should be done to all patients who are on psychotropic medications” (Hospital pharmacist)
“Vital signs (to monitor side effects), smoking status, x-ray exam, CBC, dental check and lipids profile usually done to monitor the patients’ health status” (Psychiatric nurse)
3.1.4 Awareness of clinical practice guidelines: Participants mentioned being aware of several clinical practice guidelines that they refer to for managing the physical comorbidities of people with SMI.
“We usually follow NICE, APA, ADA, AHA and the Canadian guidelines to recommend medications for patients with physical comorbidities” (Hospital pharmacist)
“There is no specific guideline for [monitoring and managing medical comorbidities in patients with mental illness], but we are following hospital clinical policies” (Nurse)
3.2 Theme 2: HCPs’ perceptions of current practice in relation to addressing the medical comorbidities among people with SMI
3.2.1 Patient self-awareness of wellness: Participants perceived that the patients’ age was related to their willingness to engage in wellness programs. Predominantly, participants perceived younger patients were more engaged than older patients. Patients with supportive families were also perceived as being more engaged with their physical care. Participants also perceived that many SMI patients feel hopeless and thus may negatively influence their motivation to access medical care.
“Patients are not [usually] followed by themselves or the healthcare providers.” (Psychiatric nurse)
“Young patients are more educated so most of them are caring about their health” (Nurse)
3.2.2 Responsibility for physical care: Participants perceived pharmacists and family members are best positioned to facilitate access to physical care while patients are living in the community. Once hospitalized, the psychiatric team (including nurses, pharmacists and doctors) are involved in their physical care and all patients are believed to have a physical examination upon admission, although some perceived that this was often inconsistent. Inpatient physicians tend to consult before starting any management strategies, although some start medications to treat medication-induced conditions (such as laxatives for antipsychotic-induced constipation). Nurses only perform vital signs assessments and pharmacists indicated they are not allowed to do any health assessments, so their role is mostly as advisor and to follow up patients at high risk for medication-induced physical comorbidities.
“Some of their physical problems can be discovered and managed when admitted to the psychiatric hospital. Family members and other medical doctors can be also involved” (Physician)
3.2.3 Referral system: Participants perceived primary health care as the most appropriate setting to refer SMI patients to manage their physical comorbidities. For more acute cases or exacerbations, patients are referred to emergency or general hospitals. Generally, HCPs perceived that psychiatrists should be referring patients rather than managing physical comorbidities in psychiatric settings.
“Like other people, [patients with mental illness should be accessing] PHCC* and emergency” (Nurse)
*Primary Health Care Center
3.2.4 Frequency of physical assessments: Participants perceived physical health assessments are done mostly when patients are admitted to hospitals, otherwise rarely or only if they are regularly checked in outpatient clinics, although they also perceived more frequent monitoring may be warranted (every 3 months if they have risk factors or if the patient is older, otherwise yearly).
“Mostly upon admission or when they go to emergency for an incident, otherwise, very rare” (Nurse)
“It should be done every 3 months unlike general population (every 6 months)” (Community pharmacist)
“Tests done to monitor the physical comorbidities usually depends on the case. Physical health checks done yearly if the patient has no comorbidity, and every 3 or 6 months if the patient has physical comorbidity” (Psychiatrist)
3.3 Theme 3: HCPs perceived barriers to the provision of medical care to people with SMI
3.3.1 Patient factors: Participants perceived the patients’ lack of knowledge or concern about their risk for medical comorbidities as a barrier to care. This barrier was linked to various factors including: the impact of the mental illness itself, their insight into their illness, poor compliance with treatments, and their self-awareness of wellness. Lack of patient education and lack of family engagement were also perceived as barriers to care.
“Those patients ... the challenge is how to convince them to see a specialist before taking what [they were prescribed] wants from [their visit to] the pharmacy” (Community pharmacist)
3.3.2 Societal factors: Stigma-related to mental health was brought up by some participants as a barrier to care. Some perceived families of people with SMI are ashamed and thus do not seek help or advice. Some participants also indicated that some issues surrounding mental illness in the unique multinational society of Qatar can possibly influence the depth of physical care provided to these patients.
“There is a lack of patient education and family engagement to increase compliance” (Primary care physician)
3.3.3 Treatment-emergent adverse effects: Participants raised concerns on medication inappropriateness leading to metabolic effects which adversely affect these patients physical health.
“Psychiatric medication may change the metabolism of other drugs that may lead to complications” (Community Pharmacist)
3.3.4 Health care system: Several health-care system barriers to addressing the medical comorbidities among people with SMI were identified, including problems with accessing services (eg. scheduling, scattered care provision by diverse HCPs), scope of practice among HCPs (eg. pharmacists and nurses not being allowed to manage medical comorbidities), lack of time (particularly physicians), training in the part of HCPs and difficulties implementing recommendations as all need the approval of physicians.
“I can monitor minor medical conditions that will [not] affect the psychiatric condition or [when] medications will [not] interact with psychiatric medications. The system in Middle East is not allowing pharmacists to manage medical conditions. Pharmacists are not [allowed] to manage medical comorbidities in pharmacies” (Community pharmacist)
3.4 Theme 4: Possible solutions expressed by HCPs towards addressing the barriers related to the provision of medical care for patients with SMI
3.4.1 Shared responsibility: Participants perceived that the assessment and management of the medical comorbidities of people with SMI should be a multidisciplinary responsibility, and that it should be shared between primary and secondary care. Having a specialized clinic, a general physician in the outpatient service, or a psychiatry unit within a general hospital to follow up the physical health of SMI patients upon hospital discharge were suggested to ensure an integrated and multidisciplinary approach. Also, participant pharmacists perceived to have an important role assessing the appropriateness of medications that can further contribute to increased risk of medical comorbidities in this population. This integration and multidisciplinary approach should be facilitated through the availability of shared electronic records and communication systems.
• Make the decision of treating the patient multidisciplinary” (Psychiatry medical resident)
• Now in the psychiatric hospital they are planning to initiate a [multidisciplinary] clinic that [will be] responsible about physical health check-up tests” (Psychiatric nurse)
• We are in a high need for a general physician to be available in the outpatient clinics” (Psychiatric nurse)
• To have a psychiatry hospital physically a part of a general hospital” (Psychiatry medical resident)
• They should open the space more for pharmacists to intervene with the treatment plan of the patients” (Hospital pharmacist)
• Electronic medical profile should be available at the pharmacy because it will help me to identify medications use period, diagnosis duration, and medication interactions. Also, it will help me to continue care rather than starting from scratch” (Community pharmacist)
3.4.2 Patient and family education: Participants suggested that patients and their families should receive adequate health education from HCPs particularly in regards to promoting healthy behaviors, medication-related side effects and how to prevent or manage them, on the availability of services and overall health education.
“The physical comorbidities could be better managed and controlled when the health care providers contact the caregivers and educate the patients about the comorbidities and the importance of the adherence to the following up tests” (Hospital pharmacist)
3.4.3 Staff education and training: There was an acknowledgment among participants that HCPs need to develop or enhance their skills on physical health care. Participants indicated these skills were primarily addressed through continuing education programs offered either live or through the internet, and practice-site based multidisciplinary professional education programs.
“I maintain myself up-to-date by checking medical and informational resources that HMC employees has access to, such as UpToDate, Lexicomp, Medscape and books” (Primary care physician)
4. Discussion
The findings of this study provide insights into the views of HCPs on their role in addressing the medical comorbidites of people with SMI. HCPs in Qatar viewed people with SMI as a population with an increased risk of medical comorbidities and at an increased need for more regular health/disease screening and treatment monitoring services than what are currently being provided. Despite this, an important theme that emerged from the interviews was that of an overall inadequacy in accessing general medical care for people with mental illness when compared to the general population. This finding is consistent with findings from similar studies which highlight that people with SMI are less likely to receive preventive services such as immunizations, cancer screening, and smoking cessation counseling than the general population [18-20]. Local research from an assessment of the medical charts of outpatients attending follow up appointments at a psychiatric hospital in Qatar found that monitoring of comorbidity-associated risk factors and other relevant physical assessment parameters (such as blood pressure, weight, hemoglobin A1c [HbA1c], blood glucose and lipids) were documented in less than 50% of patients [10].
When exploring the theme on the current practice surrounding the physical health care provision for people with SMI, HCPs perceived that people with mental illness do not care about their own physical health. This negative perception about the mentally ill has been reported in the literature, including in one study in Qatar that reported mental health nurses perceived service-users with mental illness were not interested in improving their physical health and were not motivated to exercise [21-24]. These type of negative perceptions could account for the suboptimal provision of physical care to this population, as they can influence not only HCPs involvement with people with SMI, but also induce a negative attitude from the patient’s perspective, that can lead to suboptimal engagement with healthcare services [24-26]. There were also varied opinions among the HCPs participating in this study regarding who should be the key provider. Studies have reported that most psychiatrists acknowledge the importance of physical examination of their patients, but that few routinely undertake these assessments, either because they believe the patient’s physical health is being assessed by another HCP or they do not feel competent to perform such an examination [27-29]. In this study, the participating psychiatrists believed that it is more appropriate for them to refer patients rather than managing their physical comorbidities themselves, which has been also reported in previous studies [1, 6, 29].
Several barriers were identified by the HCPs for the provision of physical healthcare to people with SMI. Patient-related factors such as treatment-emergent adverse effects, risky lifestyle factors among patients with SMI such as substance use, poor diet, lack of exercise and obesity, and the effects of mental illness on cognition. Societal factors, such as lack of family support, self-neglect, social isolation, and difficulties in communicating health needs were also highlighted. All of these barriers have been repetitively identified in numerous international studies [4-7, 29, 30]. However, an important and somehow distinctive barrier that emerged from the HCPs interviews in the current study was at the provider level, in relation to the existing mental health care structure in Qatar, where healthcare services to people with mental illness are heavily centralized to specialized settings. The HCPs in this study highlighted that there are limited personnel in mental health hospitals to address the medical problems of patients with SMI. There is also appointment scheduling and capacity problems to monitor outpatients. The literature has reported that under-resourcing of mental health services compared with other healthcare facilities exists, and that many mental healthcare providers are already stretched in attempting to manage the mental health of their patients [4, 21, 31]. In this study participants also viewed that this expanded role for HCPs who look after people with mental illness needs to be accompanied by investments and resourcing models that recognize the time requirement associated with this expanded role.
HCPs in this study also suggested strategies to overcome some of the barriers identified for delivering medical care to patients with SMI. The solutions reported emphasized on shared responsibility among family members and educating the patients and their families about the disease and the likely comorbidities in this population. These perceptions may reflect some of the country’s response to the release of the Qatar NMHS in 2013, which places a strong focus on raising public awareness of mental health illnesses in order to reduce stigma and transforming the way mental illness is perceived and treated in the country [16]. Nevertheless, how family support can improve the physical health care of people with SMI has not been thoroughly investigated in Qatar. A more exhaustive understanding of home-based family care of people with SMI through increased research in all disciplines can facilitate the documentation of progress and obstacles in family care as well as the redirection of resources. It has also been suggested that one possible approach to addressing the sequelae of SMI is to provide healthcare skills training for patients [32, 33].
Several of the other suggestions to address the barriers highlighted by HCPs were similar to those reported in the literature, including offering training programs to HCPs, distribution of clinical practice guidelines, and on-site
awareness campaigns to address the physical care needs of people with SMI [4, 5, 21, 29, 30]. Studies have reported on the use of care managers for liaison with primary care physicians, which was associated with significant improvements in the quality and outcomes of the physical needs of people with SMI. This may be a feasible strategy worth exploring in Qatar [4, 34].
Limitations of this study are mostly related to those incurred when conducting qualitative research, where the findings may be subjective to the individual’s interpretation of experiences and perceptions more easily influenced by the researcher's personal biases and idiosyncrasies [35]. It was also not possible to invite the participants to check the identified themes; being able to do so would have strengthened the findings. However, the sample size was adequate for a qualitative study, which allowed achieving full thematic saturation to generate meaningful insights from the data collected [36]. In addition, the inclusion of physicians, pharmacists, and nurses enabled to gain insight into the varying ways their roles are enacted in different practice settings to manage the medical comorbidities of people with SMI.
5. Conclusion
Results of this study suggest that HCPs in Qatar perceive that people with SMI receive suboptimal standard levels of care for their medical comorbidities. Current services for people with mental illness appear to be heavily centralized to mental health hospitals, which was identified as an important barrier to the provision of an integrated model of physical and mental healthcare. Shared responsibility that includes family members and patients themselves was strongly recommended to improve the physical health of people with SMI.
Acknowledgement
We would like to thank all healthcare practitioners (physicians, pharmacists and nurses) who participated in the interviews.
Statement of Ethics
This study complies with established guidelines for human in accordance with the World Medical Association Declaration of Helsinki as evidenced by having approval of the Institutional Review Board (IRB) at Qatar University (reference number: 18-060-3-016) and at Hamad Medical Corporation, Medical Research Center (reference number: 16023/16).
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was made possible by a UREP grant (UREP18-060-3-016) for undergraduate research from the Qatar National Research Fund (a member of Qatar Foundation).
Author Contributions
MZ contributed to the conception, design, and research protocol, in addition to being involved in all aspects of data analysis and manuscript revisions for intellectual content. SA, NI and FZ contributed to study design, conducted interviews, analysed and interpreted data, and wrote the first draft of the manuscript. YE contributed in generating the research protocol, participant recruitment and critically revising the manuscript. All authors approved the submission of the manuscript and agreed to be accountable for all aspects of the work. The findings achieved herein are solely the responsibility of the authors.
References
- De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10 (2011): 52-77.
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 72 (2015): 334-341.
- Schinnar AP, Rothbard AB, Kanter R, et al. An empirical literature review of definitions of severe and persistent mental illness. Am J Psychiatry 147 (1990): 1602-1608.
- Lawrence D, Stephen K. Inequalities in health care provision for people with severe mental illness. J Psychopharmacol 24 (2010): 61-68.
- De Hert M, Cohen D, Bobes J, et. al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 10 (2011): 138-151.
- Dunbar L, Brandt T, Wheeler A, et al. Barriers and solutions to implementing metabolic risk assessment in a secondary mental health service. Australas Psychiatry 18 (2010): 322-325.
- Bauer MS, Williford WO, McBride L, et al. Perceived barriers to health care access in a treated population. Int J Psychiatry Med 35 (2005): 13-26.
- Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70(3):22-29.
- Schulman-Marcus J, Goyal P, Swaminathan RV, et al. Comparison of trends in incidence, revascularization, and in-hospital mortality in ST-elevation myocardial infarction in patients with versus without severe mental illness. Am J Cardiol 117 (2016): 1405-1410.
- Zolezzi M, Abdulrhim S, Isleem N, et al. Medical comorbidities in patients with serious mental illness: A retrospective study of mental health patients attending an outpatient clinic in Qatar. Neuropsychiatr Dis Treat 13 (2017): 2411-2418.
- Happell B, Platania-Phung C, Scott D. Physical health care for people with mental illness: Training needs for nurses. Nurse Educ Today 33 (2013): 396-401.
- Gray R, Brown E. What does mental health nursing contribute to improving the physical health of service users with severe mental illness?? A thematic analysis. Int J Mental Health Nurs 26 (2017): 32-40.
- Druss BG. Improving medical care for persons with serious mental illness: Challenges and solutions. J Clin Psychiatry 68 (2007): 40-44.
- Wheeler A, Harrison J, Homes Z. Cardiovascular risk assessment and management in mental health clients: Perceptions of mental health and general practitioners in New Zealand. Journal of Primary Health Care 1 (2009): 11-19.
- Blythe J, White J. Role of the mental health nurse towards physical health care in serious mental illness: An integrative review of 10 years of UK Literature. International Journal of Mental Health Nursing 21 (2012): 193-201.
- Qatar National Mental Health Strategy. Changing Minds, Changing Lives 2013-2018. General Secretariat, Supreme Council of Health , Doha, Qatar (2013).
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 3 (2006): 77-101.
- Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: Systematic review of comparative studies. Br J Psychiatry 194 (2009): 491-499.
- Balon R. Fundamentals of Preventive Care. In: McCarron RM, Xiong GL, Keenan CR, Nasrallah HA, editors. Preventive Medical Care in Psychiatry: A Practical Guide for Clinicians. 1st ed. Annals of Clinical Psychiatry (2015).
- Druss BG, Walker ER. Mental disorders and medical comorbidity. The Synthesis project. Research synthesis report (2011): 4-15.
- Bressington D, Badnapurkar A, Inoue S, et al. Physical health care for people with severe mental illness: the attitudes, practices, and training needs of nurses in three Asian countries. Int J Environ Res Public Health 15 (2018): 343.
- Reavley NJ, Mackinnon AJ, Morgan AJ, et al. Stigmatising attitudes towards people with mental disorders: a comparison of Australian health professionals with the general community. Aust N Z J Psychiatry 48 (2014): 433-441.
- Hanafiah AN, Bortel TV. A qualitative exploration of the perspectives of mental health professionals on stigma and discrimination of mental illness in Malaysia. Int J Ment Health Syst 9 (2015): 10.
- Smith JD, Mittal D, Chekuri L, et al. A Comparison of provider attitudes toward serious mental illness across different health care disciplines. Stigma and Health 2 (2017): 327-337.
- Corrigan PW, Mittal D, Reaves CM, et al. Mental health stigma and primary health care decisions. Psychiatr Res 218 (2014): 35-38.
- Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: Worse physical health care for people with mental illness. Acta Psychiatr Scand 118 (2008): 169-171.
- Morden NE, Mistler LA, Weeks WB. Health care for patients with serious mental illness?: Family medicine’s role. J Am Board Fam Med 22 (2009): 187-195.
- Burton A, Osborn D, Atkins L, et al. Lowering cardiovascular disease risk for people with severe mental illnesses in primary care?: A focus group study. PLoS One 10 (2015): 0136603.
- Wheeler AJ, Harrison J, Mohini P, et al. Cardiovascular risk assessment and management in mental health clients: whose role is it anyway? Community Ment Health J 46 (2010): 531-539.
- McKibbin CL, Kitchen KA, Wykes TL, et al. Barriers and facilitators of a healthy lifestyle among persons with serious and persistent mental illness: Perspectives of community mental health providers. Community Ment Health J 50 (2013): 566-576.
- Sartorius N. Physical illness in people with mental disorders. World Psychiat 6 (2007): 3-4.
- Juan-Porcar M, Guillamón-Gimeno L, Pedraz-Marcos A, Palmar-Santos AM. Family care of people with severe mental disorders: an integrative review. Rev Lat Am Enfermagem 23 (2015): 352-360.
- Folsom D. Improving physical health care for patients with serious mental illness. In: Meyer J, Nasrallah H, ed. by. Medical Illness and Schizophrenia. 2nd ed. American Psychiatric Publishing (2009).
- Druss BG, Von Esenwein SA, Compton MT, et al. A randomized trial of medical care management for community mental health settings: The primary care access, referral, and evaluation (PCARE) study. Am J Psychiatry 167 (2010): 151-159.
- Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ 74 (2010): 141.
- Palinkas LA, Horwitz SM, Green CA, et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health 42 (2015): 533-544.
