Healthcare Disparities in the Treatment of Pediatric Distal Radius-Ulna Fractures: A Single-Institution Perspective
Article Information
Andrew Moon1, Thomas E Niemeier1, Charles Pitts1, Gerald McGwin2, Joseph Khoury3*
1Department of Orthopedic Surgery, University of Alabama, Birmingham, AL, USA
2Department of Epidemiology, University of Alabama, Birmingham, AL, USA
3Shriners Hospital for Children, Tampa, Florida, USA
*Corresponding Author: Joseph Khoury, Shriners Hospital for Children, Tampa, Florida, USA
Received: 02 July 2019; Accepted: 18 July 2019; Published: 22 July 2019
Citation:
Andrew Moon, Thomas E Niemeier, Charles Pitts, Gerald McGwin, Joseph Khoury. Healthcare Disparities in the Treatment of Pediatric Distal Radius-Ulna Fractures: A Single-Institution Perspective. Journal of Pediatrics, Perinatology and Child Health 3 (2019): 096-103.
Share at FacebookAbstract
Background: This study sought to identify variables associated with socioeconomic disparities in the treatment of distal forearm fractures in children.
Methods: A single-institution retrospective cohort study of patients less than 18 years of age with isolated fractures of the distal radius and ulna. Patient included underwent a closed reduction and casting under sedation by an orthopedic resident with outpatient, clinical follow up within two weeks of injury. Demographic data were collected. Primary outcomes evaluated were the final fracture alignment and rate of surgical treatment.
Results: 177 children included in this study, including 105 with private insurance and 72 with Medicaid or no insurance, 129 were white and 48 were minorities, and 51 were female while 126 were male. There were no statistically significant differences between patient groups when assessed for treatment outcome, mean fracture displacement, time to first clinic appointment, and duration of follow-up. Rates of surgical treatment between all groups tested were non-significant. Of patients that met institutional operative criteria, a lower percentage of non-white (p=0.03), male (p=0.07), and non-private insurance patients (p=0.08) received surgery when surgery was indicated compared to white female patients with insurance.
Conclusions: At a single institution, no clear disparities in the overall care and outcomes of children with distal radius and ulna fractures were identified. When surgery was indicated by institutional standards, a significantly greater percentage of white patients underwent surgery when compared to non-whites, but no significant difference in the percentage of good, fair, and poor outcomes between these groups was seen.
Keywords
Health Care Disparities, Forearm fractures, Children, Pediatrics
Article Details
1. Introduction
Healthcare disparities persist in the United States, particularly for the poor, the uninsured, and racial and ethnic minorities [1]. Despite efforts to close these gaps, socioeconomic and demographic factors continue to impact access to healthcare, quality of care, and treatment outcomes [2, 3]. In addition to ethical considerations, healthcare inequalities account for over $300 billion in excess health care expenditures, lost illness-related productivity, and premature deaths annually in the United States [4]. There is both a moral and economic impetus to address this issue in our society.
Healthcare disparities have been investigated in the management of anterior cruciate ligament injuries, fractures, arthritis, scoliosis, lumbar stenosis, and access to care. Pediatric orthopedic studies have shown that children with private insurance have better access to care when compared to those with Medicaid [5, 6]. Other studies have demonstrated racial disparities in the treatment of pediatric fractures, with minority patients likely to be managed differently than whites [7, 8].
Distal radius-ulna fractures are among the most common fractures seen in the pediatric population, usually caused by a fall onto an outstretched arm. Management of this type of injury is most commonly nonsurgical due to marked potential for remodeling. However, operative treatment is generally performed for fractures that fail closed management, open fractures or in the multiply injured patient. The primary aim of this study was to evaluate the relationship between socioeconomic and demographic variables with surgeon decision-making and patient outcomes in the management of displaced distal forearm fractures. The authors felt it was important to retrospectively examine our own behavior, as treating physicians, in order to uncover biases and make changes to our practice if needed. We also feel that this information will be helpful to other physicians with a similar practice profile.
2. Methods
An IRB (University of Alabama, Birmingham) approved by expedited review, retrospective cohort study was conducted at a single institution from January 1, 2010 to December 31, 2015 with patient identified from ICD 9-10 codes. The study cohort included patients less than 18 years of age who were seen in clinic within two weeks of discharge from the emergency department following an acute fracture of the distal one-third of the radius and ulna. All patients were seen by an orthopedic resident (second or third post graduate year) and underwent closed reduction and casting under sedation in the emergency room. Patients with ipsilateral upper extremity fractures, other long bone fractures, open fractures, incomplete records or cessation of follow up prior to radiographic union were not included. Less than 10% of patient sought follow up care outside of our system. Patients who presented to the emergency department on a delayed basis or those initially evaluate in the clinic were also excluded. In addition, patients who did not achieve an acceptable reduction in the emergency room were scheduled for operative treatment and excluded from analysis.
Study variables included age, sex, race, payer status, time from injury to a clinic appointment, time of cast immobilization, total number of clinic appointments and treatment (surgical versus non-surgical) were recorded. AP and lateral radiographs at the time of bony union were evaluated for residual fracture angulation. All measurements were performed independently by two authors who were blinded to patient clinical data, including race, sex, and insurance status with the exception of date of birth which is listed on radiographs. The mean value between the two reviewers was used for data analysis. Previous work has demonstrated that weighted kappa agreement between observers for common radiographic measurements about the distal radius are over 0.84 (excellent reliability) [9].
Primary outcomes were classified as either a good, acceptable, or poor based on fracture angulation at the time of bony union. A good outcome was defined as less than 10 degrees of angulation regardless of age. An acceptable outcome less than 20 degrees in patients 9 years-old or older, and less than 30 degrees in patients younger than 9 years-old. A poor outcome was defined as greater than 20 degrees in patients 9 years-old or older, and greater than 30 degrees in patients younger than 9 years-old. Coronal plane angulation was not found to be a variable that contributed to poor outcomes or decision for surgery in this cohort and was therefore excluded from analysis.
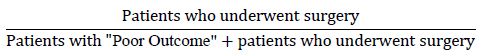
Statistical analysis was performed to compare white versus minority patients, private insurance versus Medicaid and/or no insurance, and male versus female in the study cohort. Secondary outcomes included percentage of patients who underwent surgery, average and standard deviation of displacement, average time to first clinic appointment and average total number of clinic appointments. Patients who were classified as having a “poor outcome” were considered by institutional standards to meet surgical indications. All patients with a poor outcome and no patients with a good or acceptable outcome were offered surgical treatment. The percentage of patients who met surgical indications and underwent surgery was calculated with the following equation:
A t-test was calculated for two independent means. A p-value less than 0.05 was considered significant.
3. Results
During the study period, 177 patients with distal forearm fractures who met inclusion criteria were identified. One hundred and five (59.3%) had private insurance, and 72 (40.7%) had Medicaid insurance or no insurance. Private insurance and Medicaid and/or no insurance groups showed a similar mean and median post-treatment angulations, as well as similar good, acceptable, and poor outcome percentages, none of which were statistically significant (Table 1). There was no difference in length of time to first clinic visit, number of clinic visits, and overall duration of follow up (Table 1).
|
Mean angulation +/- SD |
Private insurance (n=105) |
Medicaid and/or none (n=72) |
P value |
|
9.6 +/- 8.1 |
9.3 +/- 7.9 |
- |
|
|
Median angulation |
8 |
7 |
- |
|
% with good outcome (<10) |
53.3% (56/105) |
55.6% (40/72) |
0.25 |
|
% with acceptable outcome |
42.9% (45/105) |
40.2% (29/72) |
0.29 |
|
% with poor outcome |
3.8% (4/105) |
4.2% (3/72) |
0.4 |
|
% undergoing surgery |
9.5% (10/105) |
6.9% (5/72) |
0.39 |
|
Time to first clinic apt |
6.6 days |
6.8 days |
- |
|
# of clinic visits |
4.0 visits |
4.0 visits |
- |
|
Duration of follow up |
53.7 days |
52.9 days |
- |
|
% Surg/Surg+poor outcome |
71.4% (10/14) |
62.5% (5/8) |
0.08 |
Table 1: Health outcomes by insurance status.
There were 129 (72.9%) white patients and 48 (27.1%) non-white patients in the study population (Table 2). The length of time to first clinic visit, number of clinic visits, and overall duration of follow up were also similar between both groups. White patients had a higher mean and median angulation versus the non-white population but fewer patients with poor outcomes (p 0.03) (Table 2). When surgical indications were met, white patients were more likely to have undergone surgery than minority patients (p=0.03).
|
Mean angulation +/- SD |
White (n=129) |
Non-white (n=48) |
P value |
|
10.0 +/- 8.3 |
8.2 +/- 7.0 |
- |
|
|
Median angulation |
8 |
6 |
- |
|
% with good outcome (<10) |
52.7% (68/129) |
58.3% (28/48) |
0.1 |
|
% with acceptable outcome |
34.9% (45/129) |
29.2% (14/48) |
0.13 |
|
% with poor outcome |
12.4% (16/129) |
12.5% (6/48) |
0.3 |
|
% undergoing surgery |
9.3% (12/129) |
6.3% (3/48) |
0.27 |
|
Time to first clinic apt |
6.8 days |
6.3 days |
- |
|
# of clinic visits |
4.0 visits |
4.0 visits |
- |
|
Duration of follow up |
51.6 days |
58.4 days |
- |
|
% Surg/Surg+poor outcome |
75.0% (12/16) |
50.0% (3/6) |
0.03 |
Table 2: Health outcomes by race.
There were 51 (28.8%) female patients and 126 (71.2%) male patients in the study population (Table 3). There were no differences in length of time to first clinic visit, the number of clinic visits, and overall duration of follow up. Female patients had a slightly higher mean and median angulation than male patients, but fewer patients with poor outcomes. Overall, male patients were less likely (7.9% versus 9.8%) to undergo surgery in comparison to female (p 0.29). When surgical indications were met, 100% of female patients underwent surgery when they met surgical indications compared with just 58.8% of male patients (p=0.07).
|
Mean angulation +/- SD |
Female (n=51) |
Male n=(126) |
P value |
|
9.6 +/- 7.7 |
9.4 +/- 8.2 |
- |
|
|
Median angulation |
8 |
7 |
- |
|
% with good outcome (<10) |
52.9% (27/51) |
54.8% (69/126) |
0.1 |
|
% with acceptable outcome |
47.1% (24/51) |
39.6% (50/126) |
0.17 |
|
% with poor outcome |
0.0% (0/51) |
5.6% (7/126) |
0.29 |
|
% undergoing surgery |
9.8% (5/51) |
7.9% (10/126) |
0.29 |
|
Time to first clinic apt |
6.9 days |
6.5 days |
- |
|
# of clinic visits |
4.0 visits |
4.0 visits |
- |
|
Duration of follow up |
52.4 days |
53.8 days |
- |
|
% Surg/Surg+poor outcome |
100.0% (5/5) |
58.8% (10/17) |
0.07 |
Table 3: Health outcomes by sex.
4. Discussion
The primary aim of our study was to evaluate differences in surgical decision-making and treatment outcomes in children treated for acute distal forearm fractures based on insurance status, gender, and race. Our aim was not to highlight flaws in a single medical practice, but rather to bring to light inconsistencies in our non-standardized health system. These results showed few statistically significant differences when comparing these groups. This injury pattern was chosen for investigation due to a relatively standardized algorithm of management. Although there is a minor disagreement regarding the threshold for operative versus non-operative treatment, there are fairly general, objective parameters for the management of these injuries. Closed reduction and casting under sedation was attempted in all patients before deciding on surgical or non-surgical treatments, unless the fracture was extremely displaced and necessitated operative intervention. Surgical patients underwent open reduction and internal fixation or closed reduction with percutaneous pin fixation. Non-surgical patients were casted after closed reduction and had wedges placed if necessary to ensure proper alignment. All patients were instructed to be seen in clinic within seven days of the initial injury (Tables 1-3). Average duration of follow up was 51 to 59 days, and the average number of clinic visits was four across all patients.
Patients with private insurance were 2.6% more likely to undergo surgery than those with Medicaid or no insurance. This was not a statistically significant difference in this study. It would be interesting to look at the difference in a study with a larger sample size. The same holds true for good, acceptable, and poor outcome differences between groups. Non-whites were 3.2% more likely to have a poor outcome than whites, but patient numbers may have been too small to demonstrate significance.
Although many results did not reach statistical significance, some interesting trends were observed. Patients who were privately insured, white, or female were more likely to undergo surgical treatment. Interestingly, non-white patients were more likely to have either a good outcome or a poor outcome than white patients. Some of these trends could be explained by the severity of the initial fractures, adequacy of initial reductions, or by the healthcare disparities faced by certain socioeconomic demographics, as demonstrated in other studies. Also, as females approach skeletal maturity before males, angulation is less likely to remodel which may influence the decision to recommend surgery.
The most noteworthy results of this study were observed with the percentage of patients in each group that met surgical indications and underwent surgery, which was calculated by the ratio of patients who underwent surgery to patients who underwent surgery plus patients with poor final angulation without surgical intervention. By this metric, 71.4% of privately insured patients underwent surgery when surgical treatment was indicated, while fewer (62.5%) Medicaid and/or non-insured patients underwent surgery when it was indicated. This relationship neared statistical significance (p=0.08). When comparing female and male patients, 100.0% of female patients underwent surgery when indicated, while only 58.8% of male patients did. Of note, the female group was relatively small (n=51) and only 5 female patients received operative intervention, which likely contributed to the lack of statistical significance (p=0.07). We had originally hypothesized that insurance status was likely the largest factor influencing treatment decision. However, the data revealed a significant difference when comparing white and non-white patients, particularly in the frequency of patients in each group who underwent surgery when indicated. In white patients, 75.0% underwent surgery when indicated, while only 50.0% of non-white patients underwent surgery when indicated (p=0.03). Whether this difference represents patient or provider bias is not clear. Again, the number of patients overall who underwent surgery or had a poor outcome in each group was quite small, so this comparison is not particularly strong. Additionally, there is likely overlap between racial groups and insurance status.
A study by Skaggs et al., showed a notable disparity in accessing community orthopedic follow up care in California between those with private insurance and those with California Medicaid. Of the offices polled in this study, only 2% received Medicaid patients, demonstrating a significant disparity in healthcare access [5, 6]. Another study by Newman et al., showed an increase in time to ACL repair surgery for adolescents with non-private insurance compared with private insurance [10]. Furthermore, studies on the use of internal fixation in Medicare populations has shown a significant disparity in treatment types among socioeconomic groups [11, 8]. Similar discrepancies have been demonstrated between different socioeconomic groups in fields outside of orthopedics [12]. Directions for future studies within orthopedics may include more specialized procedures and practices, such as management of severe cervical spine injury.
There are several limitations to this study. First, it was a retrospective study and subject to the limitations inherent to such a study design. We were not able to assess functional and subjective outcomes, such as rotation and activity, as well as patient and surgeon tolerance of residual deformity. Furthermore, we were unable to gather BMI or hand dominance on all patients, which are important variables to consider in such an injury. Of note, fracture angulation in the coronal plane was not measured, as no patient had an isolated coronal plane deformity. Although our results reveal some interesting trends, more patient numbers are needed to establish statistical significance.
5. Conclusion
Although no definitive conclusions can be drawn from the results of this study, results suggest that treatment disparities are likely to exist in this field. Follow-up studies with larger cohorts may further elucidate potential disparities in these patient groups. More research is needed to clarify existing healthcare disparities in our field with the goal of providing universally equal treatment regardless of socioeconomic factors.
Conflicts of Interest
None of the authors have any conflicts of interest with respect to the submission of this work.
Funding
Departmental funding was used to fund statistical analysis. There were no other sources of funding.
References
- 2016 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality, Rockville, MD (2017).
- Adepoju OE, Preston MA, Gonzalez G. Health Care Disparities in the Post-Affordable Care Act Era. Am J Public Health 105 (2015): 665-667.
- Ayanian JZ. The Costs of Racial Disparities in Health Care. NEJM Catalyst (2016).
- Laviest TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv 41 (2011): 231-238.
- Skaggs DL, Clemens SM, Vitale MG, et al. Access to orthopedic care for children with Medicaid versus private insurance in California. Pediatrics 107 (2001): 1405-1408.
- Skaggs DL, Lehmann CL, Rice C, et al. Access to orthopaedic care for children with Medicaid versus private insurance: results of a national survey. J Pediatr Orthop 26 (2006): 400-404.
- Ravi P, Sood A, Schmid M, et al. Racial/ethnic disparities in perioperative outcomes of major procedures. Annals of Surgery 262 (2015): 955-964.
- Slover J, Gibson J, Tosteson T, et al. Racial and economic disparity and the treatment of pediatric fractures. J Pediatr Orthop 25 (2005): 717-721.
- Bozentka DJ, Beredjiklian PK, Westawski D, et al. Digital Radiographs in the Assessment of Distal Radius Fracture Parameters. Clin Orthop Rel Res 397 (2002): 409-413.
- Newman JT, Carry PM, Terhune EB, et al. Delay to reconstruction of the adolescent anterior cruciate ligament: the socioeconomic impact on treatment. The Orthopaedic Journal of Sports Medicine 2 (2014): 2325967114548176.
- Chung KC, Shauver MJ, Yin H, et al. Variations in the use of internal fixation for distal radial fracture in the United States Medicare population. J Bone Joint Surg Am 93 (2011): 2154-2162.
- Okafor PN, Stobaugh DJ, Wong Kee Song LM, et al. Socioeconomic inequalities in the utilization of colorectal stents for the treatment of malignant bowel obstruction. Dig Dis Sci 61 (2016): 1669-1676.
