Healing of a Chronic Wound after Extensive Burn Injury in An Elderly Patient Using Marine Omega3 Wound Matrix and Split-Thickness Skin Micro-Grafts: A Case Report
Article Information
Christian Smolle1*, Judith C. Geißler1, Sebastian Nischwitz1, Hannah Luze1, Lars-Peter Kamolz1
1Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Austria
*Corresponding Author: Christian Smolle, Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Austria
Received: 02 July 2022; Accepted: 10 August 2022; Published: 29 June 2023
Citation: Christian Smolle, Judith C. Geißler, Sebastian Nischwitz, Hannah Luze, Lars-Peter Kamolz. Healing of a Chronic Wound after Extensive Burn Injury in An Elderly Patient Using Marine Omega3 Wound Matrix and Split- Thickness Skin Micro-Grafts: A Case Report. Archives of Clinical and Medical Case Reports. 7 (2023): 295-298.
Share at FacebookAbstract
Elderly burn patients are at increased risk for wound healing complications, as their injuries are more likely to become deep and wound healing is impaired. Furthermore, higher age is a known risk factor for burn wound infection. New biologic matrices are promising tools in the armamentarium of wound care specialists in application of hard-to-heal wounds. We present a case of an elderly burn patient with chronic wounds that were ultimately healed using marine omega3 wound matrix for wound conditioning and meek micrografting for closure. As the patient general health status did not allow surgery under general anaesthesia, skin grafting was performed bed-side under topical anaesthesia.
Keywords
Elderly; Burn; chronic wound; Fish skin; Meek micrograft; Wound healing
Article Details
1. Introduction
Elderly patients are prone to wound healing complications after burn injuries for various reasons: First, injuries are more likely to be deep, inter alia as the skin becomes thinner with increasing age and reaction time is usually slower in the event of injury resulting in prolonged exposure to the noxious agent. Second, wound healing progresses slower and thus the risk for adverse events such as wound infection is increased. Third, elderly patients usually present with a variety of comorbidities that may compromise wound healing [1-3]. For instance, malnutrition is a common condition adversely affecting tissue repair [4].
Over the past years a variety of novel wound dressings have been added to wound specialists’ toolboxes, one of which is marine Omega3 wound matrix (KerecisÒ, Isafjordur, Iceland) that is derived from decellularized Atlantic codfish skin. Not only can this third-generation biologic dressing be handled just as any regular skin graft due to its mechanical strength, but it also has anti-inflammatory and anti-infective properties. In addition, its structure is very similar to the human skin and ingrowth of fibroblasts and capillaries is enabled by its porous microstructure. Marine Omega3 wound matrix has been seen to heal wounds faster than porcine submucosa or human amnion [5-7]. First applications chronic wounds were promising as accelerated wound closure and enhanced formation of granulation tissue was seen [8].
Whenever rapid wound healing with minimal additional donor wound surface is the desired, MEEK micrografting is a useful alternative to conventionally meshed split-thickness skin grafts (STSG). With this method, 3mm small skin squares are cut out of the graft and transferred to the wound with a silken carrier sheet. The technique allows for higher expansion rates with consistent take rates and faster wound closure relative to expansion rate when compared with the mesh technique, preparation of the grafts is however more time consuming especially when large areas have to be covered [9-11].
We present a case of an elderly, severely frail patient with a chronic wound after burn injury that was successfully treated with wound conditioning using marine Omega3 wound matrix and MEEK micrografting.
2. Case Report
An 86-year-old male patient with a medical history of stroke, prostatectomy, cardiac pacemaker implantation, arterial hypertension, dementia and alcohol abuse had sustained extensive full-thickness burns to both thighs, the right side of the abdomen and right flank averaging 15% of total body surface area (TBSA) when trying to light a coal-driven stove and falling over into the embers. The patient survived the injury and the burn wounds were treated with early epifascial excision and conventionally meshed STSG from both lower legs. Superficial Pseudomonas aeruginosa infection resulted in partial graft loss leaving a wound surface of 8% TBSA which was left to heal using conservative wound management measures. During his stay at the ICU the patient furthermore developed Covid-19 pneumonia from which he ultimately recovered.
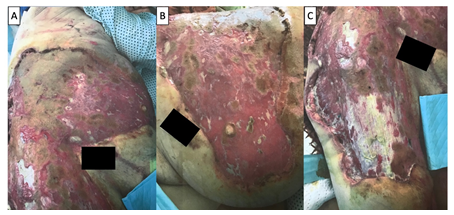
As the wounds had not healed two months after trauma, the patient was transferred to our department for further wound care. Upon admission the patient presented with extensive residual skin defects involving the right lower abdomen, flank, hip and thigh averaging 7% TBSA with scarce formation of granulation tissue and only slight regeneration of epithelium at the wound margins. The STSGs on the left thigh had otherwise healed well, however, most of the donor sites on the lower legs were not epithelialized (Figure 1). Wound swabs were still positive for multi-resistant Pseudomonas aeruginosa indicating wound colonization, which was treated with local antiseptics and i.v. Piperacillin/Tazobactam according to resistogram. After two months of continuous hospital care, the patient was bedridden, malnourished with serum protein levels as low as 5.7 g/dl (norm: 6.6-8.3) and serum albumin of 2.3 g/dl (norm: 3.5-5.3) and not fit for surgery.
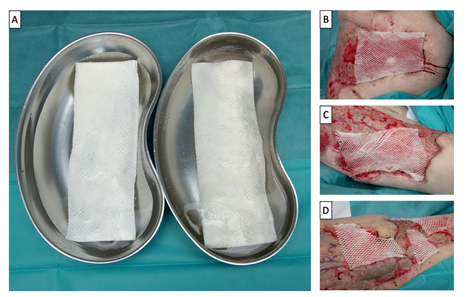
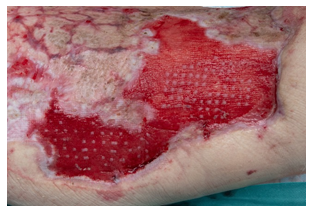
For this, conservative wound management was commenced in first place using hypochlorous acid as topical antiseptic. A high-protein diet was administered to enhance healing capacities. On day 9 after admission wound showed beginning granulation (Figure 2). Therefore, meshed marine Omega3 wound matrix was applied and fixed to the wound bed with fibrin glue and staples to enhance granulation tissue formation (Figure 3). Fatty gauze served as secondary dressing. After four days, the matrix had largely been incorporated into the wound (Figure 4). Dressing changes were commenced on a regular basis using fatty gauze and topical povidone-iodine. Throughout the following days, rapid progression of wound healing was noted, leaving only minor areas un-epithelialized on the right lower abdomen and thigh with sufficient granulation tissue formation. On day 23, there were no clinical signs of infection and the wound surface appeared ready for skin grafting. As the patient still was not fit for surgery due to his general condition, the STSG was taken bed-side from the left thigh under topical anaesthesia with eutectic mixture of lidocaine and prilocaine (EMLA). The MEEK micrografts were secured to the wound using skin staples and -100 mmHg topical negative pressure. Areas of healed skin were meanwhile protected with silver foam dressings (Mepilex AgÒ, Mölnlycke, Gothenburg, Sweden). Good graft take was seen on day 29 (Figure 5). As wound healing progressed, the patient could be transferred to his local hospital on day 38. He was eventually discharged to home care two months after admission to our department with almost completely healed wounds and only minor residual defects (Figure 6).
3. Discussion
Elderly burn patients are especially prone to wound healing complications. Recent evidence suggests that conversion of superficial burns to full thickness injuries requiring epifascial debridement becomes more likely with increasing age [2]. Higher age has furthermore been identified as independent risk factor for burn wound infection [12]. Chronic wounds differ in wound melee when compared to their non-chronic counterparts in various ways. There is a pathologic upregulation of matrix-metalloproteinases, leading to continuous breakdown of newly formed extracellular matrix thus impairing wound healing. This process can furthermore be nourished by bacterial proteinases that not only destruct extracellular matrix but also stimulate host cells to excrete proteinases themselves [13]. In our patient, secondary Pseudomonas aeruginosa wound infection and subsequent chronic colonization was the likely reason for graft loss and potentially a main culprit for development of a chronic wound. Malnutrition is a known risk factor [14] and was a further hindrance of wound healing. This was addressed by adaption of the diet towards a higher protein intake. Already with these measures, slight improvement of the wound status was evident.
Marine Omega3 wound matrix has high concentrations of long chain omega-3 fatty acids, that are largely preserved during the decellularization process. In vitro, these fatty acids have been seen to reduce bacterial growth and were even effective against several viruses, inter alia HIV and CMV [5, 6]. In their case study, Dorweiler et al. found Pseudomonas colonization as limitation of the matrix and observed premature absorption of it succeeded by enlargement of the wound surface [8]. In our patient, Pseudomonas wound colonization was addressed with application of topical antiseptics and intravenous antibiotics. Under these measures, the matrix had been largely incorporated by day 4 after application and there were no signs of absorption. We did not experience any increase of wound surface, much rather enhanced epithelialization from the wound edges and rapid formation of granulation tissue was noted.
Skin grafting with MEEK micrografts was performed to cover the residual skin defects two weeks after matrix application. As the patient was not deemed fit for surgery due to his general medical condition, skin harvest was performed under topical anaesthesia. Lumenta et al. demonstrated increased patient survival and more rapid wound closure in extensive burns when using the MEEK technique [9]. In addition, there is evidence that scar quality after healing is better when compared to conventional mesh-grafts, and the risk of infection seems to be lower [11,15]. In our patient, the MEEK technique was used mainly to limit the amount of donor area needed while a large wound surface could be treated with a relatively small graft. In case of graft failure, the procedure could easily have been repeated after another cycle of wound conditioning, possibly even using the same donor site if healed.
This case shows, that even in patients with low wound healing capacities, treatment can be successful with a holistic approach. Considering the patient’s medical history, wound situation and general condition, a stepwise procedure consisting of dietary management, wound conditioning and skin grafting under topic anaesthesia was successful. It furthermore demonstrates the potentials of currently available wound conditioning matrices in combination with well-established techniques to achieve closure of hard-to-heal wounds.
Conflict of Interest
None.
References
- Eggert E, Huss F. Medical and biological factors affecting mortality in elderly residential fire victims: a narrative review of the literature. Scars Burn Heal. Dezember 3 (2017): 2059513117707686.
- Machens HG, Pabst A, Dreyer M, et al. C3a levels and occurrence of subdermal vascular thrombosis are age-related in deep second-degree burn wounds. Surgery 139 (2006): 550-555.
- Esechie A, Bhardwaj A, Masel T, et al. Neurocognitive sequela of burn injury in the elderly. J Clin Neurosci. Januar 59 (2019): 1-5.
- Demling RH. The incidence and impact of pre-existing protein energy malnutrition on outcome in the elderly burn patient population. J Burn Care Rehabil. Februar 26 (2005): 94-100.
- Magnússon S, Baldursson BT, Kjartansson H, et al. Decellularized fish skin: characteristics that support tissue repair]. Laeknabladid. Dezember 101 (2015): 567-573.
- Baldursson BT, Kjartansson H, Konrádsdóttir F, et al. Healing rate and autoimmune safety of full-thickness wounds treated with fish skin acellular dermal matrix versus porcine small-intestine submucosa: a noninferiority study. Int J Low Extrem Wounds. März 14 (2015): 37-43.
- Kirsner RS, Margolis DJ, Baldursson BT, et al. Fish skin grafts compared to human amnion/chorion membrane allografts: A double-blind, prospective, randomized clinical trial of acute wound healing. Wound Repair Regen. Januar 28 (2020): 75-80.
- Dorweiler B, Trinh TT, Dünschede F, et al. The marine Omega3 wound matrix for treatment of complicated wounds: A multicenter experience report. Gefasschirurgie 23 (2018): 46-55.
- Lumenta DB, Kamolz LP, Frey M. Adult burn patients with more than 60% TBSA involved-Meek and other techniques to overcome restricted skin harvest availability--the Viennese Concept. J Burn Care Res 30 (2009): 231-242.
- Singh M, Nuutila K, Collins KC, et al. Evolution of skin grafting for treatment of burns: Reverdin pinch grafting to Tanner mesh grafting and beyond. Burns. September 43 (2017): 1149-1154.
- Noureldin MA, Said TA, Makeen K, et al. Comparative study between skin micrografting (Meek technique) and meshed skin grafts in paediatric burns. Burns. 29 (2022): S0305-4179.
- Ladhani HA, Young BT, Posillico SE, et al. Risk Factors for Wound Infection in Outpatients With Lower Extremity Burns. Am Surg 87 (2021): 1118-1125.
- McCarty SM, Cochrane CA, Clegg PD, et al. The role of endogenous and exogenous enzymes in chronic wounds: a focus on the implications of aberrant levels of both host and bacterial proteases in wound healing. Wound Repair Regen 20 (2012): 125-136.
- Molnar JA, Vlad LG, Gumus T. Nutrition and Chronic Wounds: Improving Clinical Outcomes. Plast Reconstr Surg. September 138 (2016): 71S-81S.
- Lee SZ, Halim AS. Superior long term functional and scar outcome of Meek micrografting compared to conventional split thickness skin grafting in the management of burns. Burns. September 45 (2019): 1386-1400.