Fetal Imaging Findings in a Case of Schinzel Giedion Syndrome
Article Information
Julliet Ogu1 and Thierry A.G.M. Huisman1*
1Edward B. Singleton Department of Radiology, Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas, USA
*Corresponding Author: Thierry A.G.M. Huisman. Edward B. Singleton Department of Radiology, Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas, USA
Received: 28 April 2023; Accepted: 05 May 2023; Published: 19 May 2023
Citation: Julliet Ogu, Thierry A.G.M. Huisman. Fetal Imaging Findings in a Case of Schinzel Giedion Syndrome. Archives of Clinical and Medical Case Reports. 7 (2023): 212-215.
Share at FacebookAbstract
Schinzel Giedion Syndrome (SGS) is an extremely rare congenital malformation syndrome caused by de novo mutations in the SETBP1 gene. This condition is characterized by distinctive craniofacial dysmorphisms such as midface retraction, severe intellectual disability, increased risk of embryonal tumors, and multiple congenital anomalies, particularly cardiac, renal, and urogenital defects. Characteristic abnormalities can be identified in the prenatal period and confirmed using molecular genetics. We present the prenatal and matching postnatal imaging findings in a case of confirmed Schinzel Giedion Syndrome.
Keywords
Schinzel Giedion Syndrome; Prenatal imaging; Ultrasound; MRI
Schinzel Giedion Syndrome articles; Prenatal imaging articles; Ultrasound articles; MRI articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Schinzel Giedion Syndrome articles Schinzel Giedion Syndrome Research articles Schinzel Giedion Syndrome review articles Schinzel Giedion Syndrome PubMed articles Schinzel Giedion Syndrome PubMed Central articles Schinzel Giedion Syndrome 2023 articles Schinzel Giedion Syndrome 2024 articles Schinzel Giedion Syndrome Scopus articles Schinzel Giedion Syndrome impact factor journals Schinzel Giedion Syndrome Scopus journals Schinzel Giedion Syndrome PubMed journals Schinzel Giedion Syndrome medical journals Schinzel Giedion Syndrome free journals Schinzel Giedion Syndrome best journals Schinzel Giedion Syndrome top journals Schinzel Giedion Syndrome free medical journals Schinzel Giedion Syndrome famous journals Schinzel Giedion Syndrome Google Scholar indexed journals Prenatal imaging articles Prenatal imaging Research articles Prenatal imaging review articles Prenatal imaging PubMed articles Prenatal imaging PubMed Central articles Prenatal imaging 2023 articles Prenatal imaging 2024 articles Prenatal imaging Scopus articles Prenatal imaging impact factor journals Prenatal imaging Scopus journals Prenatal imaging PubMed journals Prenatal imaging medical journals Prenatal imaging free journals Prenatal imaging best journals Prenatal imaging top journals Prenatal imaging free medical journals Prenatal imaging famous journals Prenatal imaging Google Scholar indexed journals prostatectomy articles prostatectomy Research articles prostatectomy review articles prostatectomy PubMed articles prostatectomy PubMed Central articles prostatectomy 2023 articles prostatectomy 2024 articles prostatectomy Scopus articles prostatectomy impact factor journals prostatectomy Scopus journals prostatectomy PubMed journals prostatectomy medical journals prostatectomy free journals prostatectomy best journals prostatectomy top journals prostatectomy free medical journals prostatectomy famous journals prostatectomy Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Pathogenesis articles Pathogenesis Research articles Pathogenesis review articles Pathogenesis PubMed articles Pathogenesis PubMed Central articles Pathogenesis 2023 articles Pathogenesis 2024 articles Pathogenesis Scopus articles Pathogenesis impact factor journals Pathogenesis Scopus journals Pathogenesis PubMed journals Pathogenesis medical journals Pathogenesis free journals Pathogenesis best journals Pathogenesis top journals Pathogenesis free medical journals Pathogenesis famous journals Pathogenesis Google Scholar indexed journals MRI articles MRI Research articles MRI review articles MRI PubMed articles MRI PubMed Central articles MRI 2023 articles MRI 2024 articles MRI Scopus articles MRI impact factor journals MRI Scopus journals MRI PubMed journals MRI medical journals MRI free journals MRI best journals MRI top journals MRI free medical journals MRI famous journals MRI Google Scholar indexed journals
Article Details
1. Introduction
Schinzel Giedion Syndrome (SGS) is an extremely rare congenital malformation syndrome caused by de novo mutations in the SETBP1 gene [1]. To date, fewer than 100 cases have been reported worldwide. This condition is characterized by distinctive craniofacial dysmorphisms, severe intellectual disability, increased risk of embryonal tumors, and multiple congenital anomalies, particularly cardiac, renal, and urogenital defects. SGS is a progressive and fatal syndrome with most affected patients dying in early childhood. Major causes of morbidity and mortality include refractory seizures, recurrent infections, feeding difficulties and respiratory failure [2]. Diagnosis is typically based on the clinical identification of characteristic symptoms, followed by confirmation through genetic testing. Some prenatal abnormalities in patients with SGS can be identified during routine prenatal ultrasound (US) screenings, though these findings are seldom correlated with SGS given the rarity of this condition. The prenatal detection of SGS offers the potential for optimized management of the affected patient, as well as early preparation for severe clinical issues that may arise during the neonatal phase and beyond. In this report, we will present fetal MRI and U/S findings as well as matching postnatal imaging in a patient with confirmed Schinzel Giedion Syndrome.
2. Case Report
At 27 weeks of gestation, a 32-year-old primigravida received a routine fetal US which identified multiple fetal abnormalities, including an absent nasal bone, abnormal ears, bilateral rocker bottom feet, and bilateral dilatation of the upper renal poles consistent with duplicated renal systems (Figure 1).
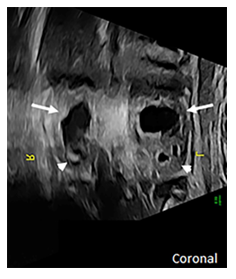
Figure 1: Coronal prenatal US of the fetal abdomen shows bilateral dilatation of the upper poles of both kidneys (arrows) while the lower poles are only mildly prominent (arrowheads) suggestive of a duplicated renal system with upper pole obstruction.
Additionally, the fetus was found to have ambiguous external genitalia although its’ internal genitalia suggested the presence of a uterus and vagina. The pregnancy was also complicated by intrauterine growth restriction and polyhydramnios. Family history was notable for the mother and the child’s father being third cousins. Following referral for genetic counseling, an amniocentesis was performed which revealed a normal 46 XX karyotype with normal results on FISH, CMA, and negative infectious panel. Whole exome sequencing results were pending at the time but would later confirm that the fetus was heterozygous for a pathogenic variant of SETBP1 which is consistent with a diagnosis of Schinzel Giedion Syndrome. The fetal ultrasound findings were confirmed on a fetal MRI performed at 30 weeks (Figure 2).
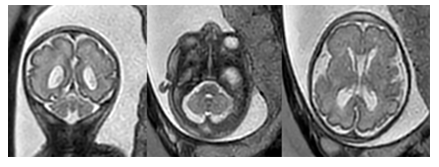
Figure 2a: Coronal and axial T2-weighted fetal MR images show mild cerebellar and vermian hypoplasia. No additional focal abnormalities noted.
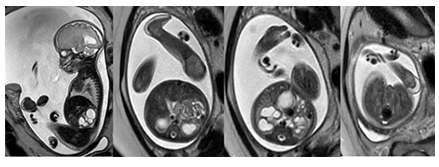
Figure 2b: Sagittal and axial T2-weighted fetal MR images show midfacial hypoplasia with an absent nasal bone as well as dilatation of the renal pelvis and prominent bilateral rocker bottom feet. Mild polyhydramnios is also noted.
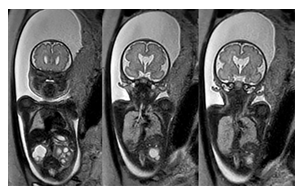
Figure 2c: Coronal T2-weighted fetal MR images confirm bilateral upper pole dominant dilatation of the collecting system of both kidneys. In addition, low set, malformed and malrotated ears are noted. A prominent cavum septum pellucidum is noted which is a typical early prenatal finding.
Additional findings on fetal MRI included urine within the fetal vagina concerning for vesicoureteral reflux or abnormal insertion of the ureter(s) into the vagina. The fetus was also noted to have folded ears and thickening of the skin over the forehead. Furthermore, the cerebellar vermis and horns, as well as the pons, were small for gestational age.
At 37 weeks, the mother was scheduled for induction of labor and delivered a female infant via vaginal delivery with initial apgar scores of 8 and 9 at one and five minutes, respectively. The early neonatal period was complicated by respiratory distress necessitating placement on 4L high-flow nasal cannula. On physical examination, the infant exhibited several notable features, including ocular hypertelorism, a retracted midface with a prominent forehead and absent nasal bridge, a high-arched cleft palate, low-set and posteriorly rotated ears with folded helixes, and hypoplastic labia majora with prominent labia minora. Additionally, the patient was found to have significant external rotation of both feet and bilateral talipes calcaneovalgus. An MRI brain (Figure 3) performed at one week of age depicted hypoplasia of the pons and cerebellum and a postnatal renal ultrasound (Figure 4) noted bilateral hydroureteronephrosis, both findings consistent with the original prenatal imaging findings. Furthermore, a voiding cysto-urethrogram was performed which excluded vesico-ureteral reflux as well as a skeletal survey which assessed the patient’s foot deformity (Figure 5).
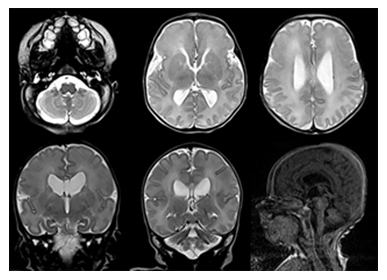
Figure 3: Postnatal brain MR images (upper row: axial T2-weighted MRI, lower row: coronal T2-weighted and sagittal T1-weighted MRI) confirm mild cerebellar and vermian hypoplasia, shallow pontine belly and mild ventriculomegaly.

Figure 4: Postnatal renal US (axial and sagittal) depicts moderate bilateral widening of the renal pelvis as well as moderate hyper-echogenicity of the renal parenchyma. The bladder appears normal.

Figure 5: Lateral X-ray of the left foot and ankle show the severe foot deformity.
3. Discussion
Schinzel Geidion Syndrome, first described in 1978 by Albert Schinzel and Andreas Giedion, is characterized by distinctive craniofacial deformities such as severe midface retraction, multisystem congenital abnormalities, an increased risk of neuroepithelial tumors, seizures, and global developmental delay [3, 4]. SGS is caused by heterozygous de novo mutations in the SETBP1 gene located on chromosome 18. The physiological function of the SETBP1 gene remains incompletely understood. However, the disease mechanism is believed to be secondary to a gain of function mutation that leads to the accumulation of the SETBP1 protein. The protein product has demonstrated involvement in gene expression regulation and exhibits ubiquitous expression, including disruption of the normal embryonic development of multiple organs suggesting a correlation with the multisystemic effects associated with the condition [5].
Prior to the discovery of the SETBP1 gene as the genetic cause for this condition, the diagnosis of SGS was based on the presence of key clinical features. Lehman et al proposed clinical criteria for diagnosis based on the presence of developmental delay and a distinctive facial phenotype (midface retraction, prominent forehead, nasal hypoplasia, dysplastic ears, and hypertelorism) associated with hydronephrosis and skeletal/limb malformations [3, 6]. Patients with SGS also commonly suffer from cardiac and genital abnormalities, seizures, severe intellectual disability, progressive neurodegeneration and difficulties with swallowing and breathing [3, 7-10]. Other symptoms may include vision and hearing problems, sleep apnea, choanal stenosis, macroglossia, abnormal dentition and hypotonia. Individuals affected by this condition typically do not survive past early childhood (18 months-4 years), with feeding difficulties, respiratory failure, recurrent infections, and refractory seizures being the most common causes of death [7-10]. SGS is a severe and progressive syndrome. The goals of treatment are focused on addressing the patient’s symptoms and improving their quality of life.
With the introduction of high-resolution prenatal US and MRI, characteristic prenatal abnormalities can be identified on fetal imaging and confirmed through molecular genetics. This report presents the prenatal imaging findings of a patient with SGS, revealing characteristic features such as hydronephrosis, skeletal/ limb abnormalities, nasal hypoplasia, a prominent forehead, dysplastic ears, and ambiguous genitalia. These findings were then confirmed on postnatal imaging. Given the rarity of SGS, clinical suspicion may be low in patients with multiple congenital anomalies on fetal imaging. When these characteristic fetal imaging findings are observed, Schinzel Giedion Syndrome should be considered as a potential diagnosis.
Conflicts of Interest
We have no conflicts of interest to disclose.
References
- A Hoischen et al. De novo mutations of SETBP1 cause Schinzel-Giedion syndrome. Nat Genet 42 (2010): 483-5
- A Takeuchi et al. Progressive brain atrophy in Schinzel-Giedion syndrome with a SETBP1 mutation. Eur. J. Med. Genet 58 (2015): 369-371.
- A M Lehman, D McFadden, D Pugash, et al. Schinzel-Giedion syndrome: Report of splenopancreatic fusion and proposed diagnostic criteria. Am. J. Med. Genet. A 146 (2008): 1299-1306.
- L J Anyanwu et al. Schinzel-Giedion syndrome: a case with sacrococcygeal teratoma and cor-triatriatum dexter. Pan Afr. Med. J 26 (2017).
- A Hoischen et al. De novo mutations of SETBP1 cause Schinzel-Giedion syndrome. Nat. Genet 42 (2010): 483-5.
- Y Herenger et al. Long term follow up of two independent patients with Schinzel-Giedion carrying SETBP1 mutations. Eur. J. Med. Genet 58 (2015): 479-487.
- Bulut, Z Ince, U Altunoglu, et al. Schinzel-Giedion Syndrome with Congenital Megacalycosis in a Turkish Patient: Report of SETBP1 Mutation and Literature Review of the Clinical Features. Case Rep. Genet 4 (2017): 1-4
- P Labrune et al. Three new cases of the Schinzel-Giedion syndrome and review of the literature. Am. J. Med. Genet 50 (1994): 90-93.
- R Acuna-Hidalgo et al. Overlapping SETBP1 gain-of-function mutations in Schinzel-Giedion syndrome and hematologic malignancies. PLoS Genet 13 (2017): e1006683.
- J M Ko et al. Distinct neurological features in a patient with Schinzel-Giedion syndrome caused by a recurrent SETBP1 mutation. Childs Nerv. Syst 29 (2013): 525-529.
