Failure to Adjust CT Scanners to Pediatric Settings is a Major Cause of Unnecessary Radiation Exposure to Children
Article Information
Jianna J. Lin1*, Jeremy Zhang1, Lucille Anzia1, Laura L. Hayes1,2
1University of Central Florida College of Medicine, 6850 Lake Nona Blvd, Orlando, Florida, United States
2Nemours Children’s Health Florida, 13535 Nemours Pkwy., Orlando, Florida, United States
*Corresponding Author: Jianna J. Lin, University of Central Florida College of Medicine, 6850 Lake Nona Blvd, Orlando, Florida, United States
Received: 01 October 2023; Accepted: 10 October 2023; Published: 16 October 2023
Citation: Jianna J Lin, Jeremy Zhang, Lucille Anzia, Laura L Hayes. Failure to Adjust CT Scanners to Pediatric Settings is a Major Cause of Unnecessary Radiation Exposure to Children. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 210-217.
Share at FacebookAbstract
CT scans are an indispensable tool for evaluating head injuries and neurological symptoms, yet they are the leading contributor to medical radiation exposure in the United States. High levels of such exposure pose significant health risks for children, whose developing bodies are less resilient to radiation injury. Here we review mean radiation dose (Total Exam DLP) and CTDlvol from head CT scans of 149 cases to assess for factors thought to be potential contributors to excess radiation exposure. Such factors included scan indication (trauma, shunts, other head complaints), number of repeat scans, and the type of facility the scan was performed (adult vs. pediatric). Analyses revealed that among scans performed to evaluate head trauma or routine indications (e.g. headache, vomiting focal neurologic deficits), the mean radiation dose a administered was significantly higher in adults hospitals when compared to pediatric hospitals. Findings highlight the importance of ensuring appropriate dose settings to increase the safety of CT scans for children. Based on our results identifying suboptimal scanner settings as a fundamental cause of excess radiation exposure, the evidence supports adjusting protocols to appropriate settings as the most effective method of reducing excess radiation exposure to children receiving head CT scans.
Keywords
Computed tomography; Pediatric; Radiation; Children
Pediatric articles Pediatric Research articles Pediatric review articles Pediatric PubMed articles Pediatric PubMed Central articles Pediatric 2023 articles Pediatric 2024 articles Pediatric Scopus articles Pediatric impact factor journals Pediatric Scopus journals Pediatric PubMed journals Pediatric medical journals Pediatric free journals Pediatric best journals Pediatric top journals Pediatric free medical journals Pediatric famous journals Pediatric Google Scholar indexed journals Children articles Children Research articles Children review articles Children PubMed articles Children PubMed Central articles Children 2023 articles Children 2024 articles Children Scopus articles Children impact factor journals Children Scopus journals Children PubMed journals Children medical journals Children free journals Children best journals Children top journals Children free medical journals Children famous journals Children Google Scholar indexed journals Computed tomography articles Computed tomography Research articles Computed tomography review articles Computed tomography PubMed articles Computed tomography PubMed Central articles Computed tomography 2023 articles Computed tomography 2024 articles Computed tomography Scopus articles Computed tomography impact factor journals Computed tomography Scopus journals Computed tomography PubMed journals Computed tomography medical journals Computed tomography free journals Computed tomography best journals Computed tomography top journals Computed tomography free medical journals Computed tomography famous journals Computed tomography Google Scholar indexed journals Head injuries articles Head injuries Research articles Head injuries review articles Head injuries PubMed articles Head injuries PubMed Central articles Head injuries 2023 articles Head injuries 2024 articles Head injuries Scopus articles Head injuries impact factor journals Head injuries Scopus journals Head injuries PubMed journals Head injuries medical journals Head injuries free journals Head injuries best journals Head injuries top journals Head injuries free medical journals Head injuries famous journals Head injuries Google Scholar indexed journals Neurological disorders articles Neurological disorders Research articles Neurological disorders review articles Neurological disorders PubMed articles Neurological disorders PubMed Central articles Neurological disorders 2023 articles Neurological disorders 2024 articles Neurological disorders Scopus articles Neurological disorders impact factor journals Neurological disorders Scopus journals Neurological disorders PubMed journals Neurological disorders medical journals Neurological disorders free journals Neurological disorders best journals Neurological disorders top journals Neurological disorders free medical journals Neurological disorders famous journals Neurological disorders Google Scholar indexed journals Mammograms articles Mammograms Research articles Mammograms review articles Mammograms PubMed articles Mammograms PubMed Central articles Mammograms 2023 articles Mammograms 2024 articles Mammograms Scopus articles Mammograms impact factor journals Mammograms Scopus journals Mammograms PubMed journals Mammograms medical journals Mammograms free journals Mammograms best journals Mammograms top journals Mammograms free medical journals Mammograms famous journals Mammograms Google Scholar indexed journals Carcinogen articles Carcinogen Research articles Carcinogen review articles Carcinogen PubMed articles Carcinogen PubMed Central articles Carcinogen 2023 articles Carcinogen 2024 articles Carcinogen Scopus articles Carcinogen impact factor journals Carcinogen Scopus journals Carcinogen PubMed journals Carcinogen medical journals Carcinogen free journals Carcinogen best journals Carcinogen top journals Carcinogen free medical journals Carcinogen famous journals Carcinogen Google Scholar indexed journals Leukemia articles Leukemia Research articles Leukemia review articles Leukemia PubMed articles Leukemia PubMed Central articles Leukemia 2023 articles Leukemia 2024 articles Leukemia Scopus articles Leukemia impact factor journals Leukemia Scopus journals Leukemia PubMed journals Leukemia medical journals Leukemia free journals Leukemia best journals Leukemia top journals Leukemia free medical journals Leukemia famous journals Leukemia Google Scholar indexed journals CT imaging articles CT imaging Research articles CT imaging review articles CT imaging PubMed articles CT imaging PubMed Central articles CT imaging 2023 articles CT imaging 2024 articles CT imaging Scopus articles CT imaging impact factor journals CT imaging Scopus journals CT imaging PubMed journals CT imaging medical journals CT imaging free journals CT imaging best journals CT imaging top journals CT imaging free medical journals CT imaging famous journals CT imaging Google Scholar indexed journals Thyroid articles Thyroid Research articles Thyroid review articles Thyroid PubMed articles Thyroid PubMed Central articles Thyroid 2023 articles Thyroid 2024 articles Thyroid Scopus articles Thyroid impact factor journals Thyroid Scopus journals Thyroid PubMed journals Thyroid medical journals Thyroid free journals Thyroid best journals Thyroid top journals Thyroid free medical journals Thyroid famous journals Thyroid Google Scholar indexed journals Cancers articles Cancers Research articles Cancers review articles Cancers PubMed articles Cancers PubMed Central articles Cancers 2023 articles Cancers 2024 articles Cancers Scopus articles Cancers impact factor journals Cancers Scopus journals Cancers PubMed journals Cancers medical journals Cancers free journals Cancers best journals Cancers top journals Cancers free medical journals Cancers famous journals Cancers Google Scholar indexed journals Radiosensitivity articles Radiosensitivity Research articles Radiosensitivity review articles Radiosensitivity PubMed articles Radiosensitivity PubMed Central articles Radiosensitivity 2023 articles Radiosensitivity 2024 articles Radiosensitivity Scopus articles Radiosensitivity impact factor journals Radiosensitivity Scopus journals Radiosensitivity PubMed journals Radiosensitivity medical journals Radiosensitivity free journals Radiosensitivity best journals Radiosensitivity top journals Radiosensitivity free medical journals Radiosensitivity famous journals Radiosensitivity Google Scholar indexed journals Pediatric patients articles Pediatric patients Research articles Pediatric patients review articles Pediatric patients PubMed articles Pediatric patients PubMed Central articles Pediatric patients 2023 articles Pediatric patients 2024 articles Pediatric patients Scopus articles Pediatric patients impact factor journals Pediatric patients Scopus journals Pediatric patients PubMed journals Pediatric patients medical journals Pediatric patients free journals Pediatric patients best journals Pediatric patients top journals Pediatric patients free medical journals Pediatric patients famous journals Pediatric patients Google Scholar indexed journals CT scans articles CT scans Research articles CT scans review articles CT scans PubMed articles CT scans PubMed Central articles CT scans 2023 articles CT scans 2024 articles CT scans Scopus articles CT scans impact factor journals CT scans Scopus journals CT scans PubMed journals CT scans medical journals CT scans free journals CT scans best journals CT scans top journals CT scans free medical journals CT scans famous journals CT scans Google Scholar indexed journals Trauma articles Trauma Research articles Trauma review articles Trauma PubMed articles Trauma PubMed Central articles Trauma 2023 articles Trauma 2024 articles Trauma Scopus articles Trauma impact factor journals Trauma Scopus journals Trauma PubMed journals Trauma medical journals Trauma free journals Trauma best journals Trauma top journals Trauma free medical journals Trauma famous journals Trauma Google Scholar indexed journals
Article Details
1. Introduction
Computed tomography (CT) scans have become a cornerstone of modern medicine since their advent in the 1970s. The utilization of CT scans has increased an estimated 10% annually since the mid-1990’s [1]. Their capability to provide unparalleled visualization and detection of a variety of medical conditions has contributed to their widespread use in the current day and a dramatic increase in their use over the past decade [2-5]. In children, CT scans of the head are frequently obtained despite minimal suspicion or expectation for abnormalities on CT imaging, due to the significance of potential complications of head injuries and neurological disorders in children [6]. These include the fact that head trauma is the leading cause of mortality and morbidity in children [7]. Over 50% of children presenting to the emergency room with head injuries receive head CT scans - of these, an estimated 1 in 3 CT scans were unnecessary [8].
Although CT scans are an integral tool in the diagnosis and evaluation of a wide variety of medical conditions, they the leading contributor to medical radiation exposure in the United States today [2,6,7]. Altogether, CT scans account for an estimated 75% of all medical radiation exposure [6]. This is suspected to be due to not only the increasing use of CT scans, but alsothe fact that CT scans inherently deliver much higher doses of radiation than other types of medical imaging, such as conventional radiographs or mammograms [8]. Radiation exposure poses an especially deleterious effect on children, whose developing bodies are more sensitive to radiation harm than those of adults [9].
CT scans are obtained using a rotating machine that emits X-rays, a form of ionizing radiation, through a patient’s body. This enables the capture of two-dimensional images of the body from multiple angles, which are digitally combined to create 3D cross-sectional images of the body’s internal structures. This process produces images of much greater detail than traditional x-rays, enabling greater detection and visualization of various medical conditions. However, because the process of obtaining CT scans involves repeated and prolonged exposure to radiation, the effective dose required to produce one head CT scan is equivalent to approximately 100 chest X-rays [10]. Although this exposure to ionizing radiation allows an unparalleled visualization of the body’s internal structures in high detail, excess exposure to ionizing radiation is known to cause harmful health consequences [11,12].
Ionizing radiation is a known carcinogen [10], as revealed by exposures from nuclear disasters in Hiroshima, Nagasaki [12,13], and Chornobyl [14]. Exposure to medical ionizing radiation has been known to cause significant harm to children. The first study that assessed the risk of cancer associated with a CT scan during childhood found a clear dose-dependent relationship between brain tumors and leukemia, with risk of both cancers increasing directly with cumulating radiation dose. Each 50 milligray or mGy (mGy is a unit of estimated dose of ionizing radiation absorbed) to the head was associated with a threefold increase in risk for brain tumors, while each 50 mGy dose to bone marrow was associated with a threefold increase in risk for leukemia [15]. The dependent relationship between cancer and pediatric CT scans has been recently reported in head CT scans as well [16].
Today, it is widely accepted that ionizing radiation has greater detrimental health effects for children than for adults, such as greater relative risk of cancers of brain, breast, skin, thyroid, and leukemia [17]. It is suspected that this increased susceptibility to the harms of ionizing radiation in children is due to greater radiosensitivity of developing organs and tissues [18,19]. Children and adolescents who received multiple CT scans have been found to have an increased risk for cancer [20-27]. Studies have shown that children who undergo multiple head CT scans are at a higher risk of developing leukemia and brain tumors than those who do not undergo any CT scans [2]. Children exposed to medical radiation of the head have also been found to suffer from long-term intellectual decline, attention difficulties, slowed thinking, and memory impairment [27]. Estimates of lifetime age-dependent cancer mortality risks associated with common CT examinations predict that of the roughly 600,000 abdominal and head CT scans performed annually in children under 15 years old, approximately 500 of these individuals will die from CT radiation-related cancer [28].
A certain level of radiation administration is required for image quality. However, during the CT scanning process, children sometimes receive a higher-than-necessary dose of radiation while being scanned [25]. Recent literature is filled with reports of cases of excessively high radiation dose [29,30].
Current efforts are being made to optimize radiation dose and decrease excessive radiation dose in pediatric patients. One such effort is the Image Gently and Think A-Head campaign, which was launched in 2008 and focuses on radiation safety in pediatric imaging. The campaign promotes the use of the ALARA (As Low As Reasonably Achievable) principle, which means that radiation doses should be kept as low as possible while still obtaining high-quality images [31]. Other initiatives, such as the Image Wisely campaign, focus on reducing radiation exposure in adult patients [32]. Although these efforts have been made, cases of higher-than-necessary radiation still exist. This calls for increased public attention to the need for optimizing radiation dose in pediatric head CT scans.
Attempts to elucidate the causes of excess radiation administration to children during the CT scanning process have revealed improper CT scanner settings that are inappropriate for a child’s smaller body size or for the indication the scan is being taken for as a potential contributor [29,33]. Due to their smaller size, children do not require as much radiation as adults for a head CT for the same indication, because the radiation dose required for appropriate image quality is directly related to patient size. Pediatric head CT protocols are often based on the patient’s age, and use lower tube currents and voltage settings to decrease the radiation dose without compromising image quality [29,33].
Differing indications for head CT scans require differing radiation doses for appropriate image quality. Head CT scans are commonly used for various indications, including evaluation of trauma, shunt dysfunction, and other routine indications. For instance, head CT scans performed for possible shunt malfunction do not require as much dose as trauma studies because the evaluation of ventricular size does not require as much detail.
2. Methods
In this study, we reviewed the radiation dose administered and number of repeat scans in head CT scan examinations across 8 hospitals within a healthcare system: 3 pediatric hospitals (serving pediatric patients exclusively) and 5 adult hospitals (serving patients of all ages) in the Atlantic region of the United States. All imaging reviewed was obtained by a radiologist through a random query for head CT scans performed between January 2021 through October 2021 on Picture Archiving and Reporting System (PACS), where the imaging data of patients receiving imaging at this healthcare system is stored.
All CT scans reviewed were performed in patients ≤ 18 years of age. Demographics and clinical data are reported in Table 1. The median age of the patients was 10 years (interquartile range: 4–15 years). Patients were 15.7% (20) Caucasian, 3.15% African American, 3.15% (4) Hispanic or Latino, 1.57% Other, and 51.2% unknown. Figure 1 illustrates the study methodology and sample sizes of all comparison groups. Of the 149 cases of head CT scans obtained through random query on PACS, 22 cases were excluded, n = 18 for inability to obtain radiation dose values, n = 2 for inability to view the imaging associated with the case on PACS, and n = 2 for the case not being a CT of the head, but rather, of the abdomen. The remaining 127 cases of head CT scans were included in the final analysis (Figure 1). Of these, we categorized each CT head exam into three groups: trauma (n = 56), shunt (n = 22), and routine (n = 49), due to the differences in radiation dose required for appropriate image quality of head CT scans obtained for different indications, as discussed above. Clinical data regarding head CT scan indication for each of the three indications are reported in Table 2.
|
Total |
Trauma group |
Shunt group |
Routine group |
|
|
n = 127 |
n = 56 |
n = 22 |
n = 49 |
|
|
Age, years |
10 (4 – 15) |
9.5 (3 – 15) |
3 (1.33 – 10) |
12 (5.5 – 15) |
|
Ethnicity |
||||
|
Caucasian |
20 |
12 |
1 |
7 |
|
Hispanic or Latino |
4 |
1 |
0 |
3 |
|
African American |
4 |
2 |
1 |
1 |
|
Other |
2 |
1 |
0 |
1 |
|
Unknown |
65 |
33 |
20 |
12 |
Table 1: Patient characteristics and indications for head CT scan. CT computed tomography. For age, median age and interquartile range are reported.
|
Trauma (n = 56) |
|
|
Blunt force trauma to craniofacial region |
38 |
|
Fall on craniofacial region |
12 |
|
Motor vehicle accident |
5 |
|
Assault |
1 |
|
Shunt (n = 22) |
|
|
Altered mental status in patient with IC or VP shunt |
13 |
|
IC or VP shunt assessment |
4 |
|
Bradycardia in patient with IC shunt |
2 |
|
Increased seizure activity in patient with IC shunt |
2 |
|
Ventricular size evaluation |
1 |
|
Routine (n = 49) |
|
|
Vomiting |
25 |
|
Altered mental status |
9 |
|
Focal neurologic deficits |
4 |
|
Seizures |
3 |
|
Abnormal head circumference |
2 |
|
Craniosynostosis (Trigonocephaly) |
2 |
|
Pupil dilation abnormalities |
2 |
|
Cerebral edema, hemorrhage |
2 |
Table 2: Clinical data for each head CT scan indication. IC intracerebral, VP ventriculoperitoneal, CSF cerebrospinal fluid.
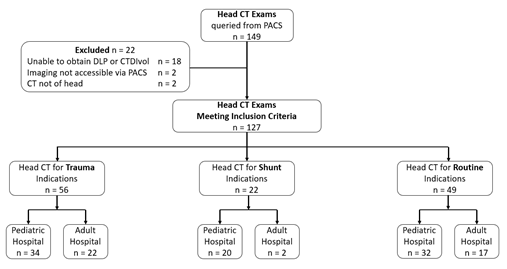
Figure 1: Flow chart of the project. DLP dose length product, CTDIvol CT dose-length product per unit volume.
For each of the three indications, CT head scans were categorized by the type of facility in which they were performed (adult vs. pediatric), resulting in six total comparison groups. Of the CT head scans performed for trauma, n = 34 were performed in pediatric hospitals and n = 22 were performed in adult hospitals; of those performed for cerebral shunts, n = 20 were performed in pediatric hospitals and n = 2 were performed in adult hospitals; of those performed for routine indications, n = 32 were performed in pediatric hospitals and 17 were performed in adult hospitals. For each case, the radiation dose in terms of Total Exam DLP and CT Dose Index in mGy/cm and mGy, respectively, patient weight, total number of scans taken, facility type (adult vs. pediatric), and scan indication were reviewed.
2.1 Radiation Dose Measurement and Calculation
Total exam dose length product (DLP) is a commonly used radiation dose metric in computed tomography (CT) imaging that represents the total amount of radiation delivered to a patient during an entire CT exam [34]. DLP is calculated by multiplying the CT dose index (CTDI) by the length of the scanned volume, which takes into account both the radiation intensity and the length of the scanned region. Essentially, DLP quantifies the radiation dose the patient receives over the course of the entire CT exam and is measured in units of milligray centimeters (mGy-cm) [35,36]. CTDLvol, or CT dose-length product per unit volume, is a relatively new metric that has been developed to provide a more accurate representation of the radiation dose received by a patient during a CT scan. It accounts for the fact that the dose is not evenly distributed throughout the body and varies depending on the specific area being scanned. CTDLvol is calculated by dividing the CT dose-length product (DLP) by the scan length and the volume of the scanned region [37].
The primary measures analyzed were Total Exam Dose Length Product (DLP) and CT Dose Index (CTDIvol), both of which are standard units used to measure radiation dose, as described earlier. For each case, both metrics were obtained from dose report data on PACS. PACS typically stores two types of information: the CT images themselves and the dose report data. The dose report data included exam DLP and CTDlvol for each CT head examination. In our study, Total Exam DLP and CTDIvol measures was calculated by summation of the Total Exam DLP and CTDIvol doses administered for all scans taken during the CT head examination. This included the CT head scans themselves and also scout scans, which are images taken as a part of the CT head examination process to aid in the planning and subsequent radiologist review of images. That is, the radiation dose associated with all scans performed during a CT head examination process were included in the calculation of both measures of radiation dose. Total exam DLP was then to assess the total radiation dose a patient received during the CT head examination process [3]. The number of repeat scans (and the reason for the repeat scan- usually patient motion during the scanning process) were collected from PACS dose report data as secondary measures.
2.2 Statistical analyses
Mean Total Exam DLP and mean CT Dose Index were calculated by taking the arithmetic mean of the total exam DLP and CT Dose Index, respectively, for each comparison group. t-tests for independent samples were utilized to compare mean Total Exam DLP and mean CTDIvol of head CT scans between pediatric and adult hospitals for CT scans performed for trauma and routine indications. This was done to determine if there was a significant difference in the amount of radiation exposure patients received between adult versus pediatric hospitals. A p-value < 0.05 was used to determine significant differences. No t-tests were performed for the CT head for cerebral shunts group as there were too few CT head examinations for the shunt indication completed in an adult hospital for any meaningful statistical analysis using independent t-test.
2.3 Ethics approval and patient consent
This was a HIPAA-compliant retrospective study with the approval of Nemours Children’s Health Institutional Review Board. Informed patient consent was waived by Nemours Children’s Health Institutional Review Board and all methods were performed in accordance with the ethical standards of Helsinki Declaration. The cases that were used for analysis were randomly selected from head CT scans from January 2021 through October 2021 and read by a radiologist affiliated with these hospitals.
3. Results
Radiation dose data (Mean Total Exam DLP, Mean CTDIvol), number of repeat scans, and P values from t-tests comparing Mean Total Exam DLP and Mean CTDIvol between adult and pediatric hospitals is reported in Table 3.
|
Head CT Scan Indication |
Variable |
Pediatric Hospital |
Adult Hospital |
P-value |
|
Trauma |
n = 32 |
n = 29 |
||
|
Mean Total Exam DLP (mGy/cm) |
302.9 |
406.1 |
0.009 |
|
|
Mean CTDlvol (mGy) |
16.7 |
24.8 |
0.002 |
|
|
Number of Repeat Scans |
1 |
0 |
||
|
Routine |
n = 31 |
n = 18 |
||
|
Mean Total Exam DLP (mGy/cm) |
407.1 |
391.7 |
0.002 |
|
|
Mean CTDlvol |
16.6 |
22.8 |
<0.001 |
|
|
Number of Repeat Scans |
0 |
0 |
Table 3: two-tailed t test for independent samples assuming equal variances comparing mean Total Exam DLP and mean CTDlvol between pediatric versus adult hospitals for CT head scans for trauma and routine indications.
3.1 Total Exam DLP
The primary variable mean Total Exam DLP was significantly different in head CT scans administered for trauma between adult (M = 406.1 mGy/cm) and pediatric (M = 302.9 mGy/cm) hospitals (p = 0.009), as illustrated in Figure 2A. Mean Total Exam DLP was also significantly different in head CT scans administered for routine indications between adult (M = 407.1 mGy/cm) and pediatric (M = 391.7 mGy/cm) hospitals (p = 0.002).
3.2 CTDIvol
The other primary variable mean CTDIvol was significantly different in head CT scans administered for trauma indications between adult (M = 24.8 mGy) and pediatric (M = 16.7 mGy) hospitals (p = 0.002), as seen in Figure 2B. Mean CTDIvol was also significantly different in head CT scans performed for routine indications between adult (M = 22.8 mGy) and pediatric (M = 16.6 mGy) hospitals (p <0.001).
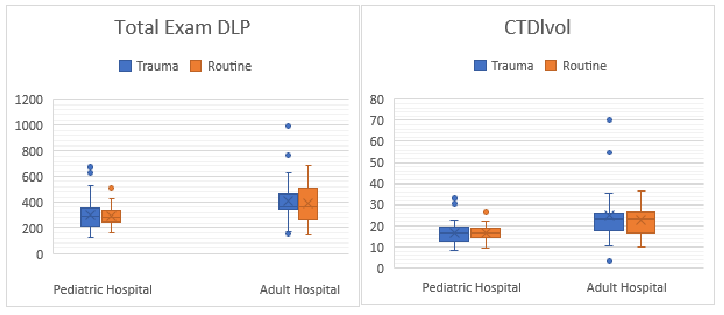
Figure 2 (A-B): DLP dose length product, CTDIvol CT dose-length product per unit volume.
3.3 Repeat Scans
There was no significant difference in the number of repeat scans, between adult and pediatric hospitals for either trauma or routine indications, as only one case required repeat scanning due to motion. The number of repeat scans was therefore also not associated with a significantly higher mean radiation dose.
4. Discussion
The results of this study demonstrate that pediatric patients who received head CT scans for trauma or routine indications at hospitals serving all ages received significantly higher radiation doses compared to those who received head CT scans at hospitals serving pediatric patients exclusively. This difference was observed across both radiation dose metrics studied, including total radiation dose (total exam DLP) and intensity of the radiation (CTDlvol). These results suggest that there exists a tendency towards excessive exposure of pediatric patients to radiation levels that exceed the dose required for an adequate head CT scan in adult hospital settings, irrespective of whether the scans are conducted for the evaluation of head trauma or routine indications.
Notably, our results suggest that repeat scanning is not a principal contributor to excessive radiation exposure in children undergoing head CT scans. In the CT head exams we reviewed, there was only one case of a repeat scan for motion artifact. Therefore, repeat scanning for motion may be ruled out as a significant contributor to unnecessarily high radiation exposure. This evidence excluding the possibility that repeat scanning is a contributor to significantly undue radiation exposure further underscores that excess radiation dose is primarily due to a lack of optimization of scan parameters for children. This finding further implicates the type of facility, pediatric versus adult, as the primary differentiator of rates of excess radiation dose in a hospital. A larger sample size would be helpful in further supporting this claim by showing insignificant contribution of increased radiation exposure due to repeat scanning.
Existing literature supports our findings that excessive radiation administration is related to flaws in CT scanning protocols and imaging technician fatigue. For instance, Van der Merwe et al. [38] found that CT scans occurring after-hours used higher radiation dosages than those during business hours, possibly suggesting technologist fatigue as a contributor to inappropriate radiation dose use. Our findings that repeat scanning for motion was not a cause for higher radiation exposure further underscore that the primary cause of unnecessarily high radiation dose usage involves errors or events during the CT scanning process.
Our results may also suggest that imaging technologist fatigue accounts for excessive radiation administration. This is because there is a greater range of radiation doses used in CT scanners in adult hospitals, meaning that the consequences of failing to adjust the radiation dose administered between patients is likely to have a greater chance of providing an inappropriate dose for the next patient when compared to pediatric hospitals. For this reason, if an imaging technician fails to change the radiation dose between patients due to fatigue, if they worked at an adult hospital, it is plausible that the consequences of their fatigue would be more likely to expose a pediatric patient to an unnecessarily high level of radiation than if they worked at a pediatric hospital. Imaging technician fatigue may therefore explain the observed differences in radiation dose between adult and pediatric hospitals in the present study.
Such errors during the CT scanning process that may serve as principal contributors to excessively high radiation exposure include inadequate training for medical imaging technologists, imaging technologist fatigue, and a lack of consistency or standardization of the CT scanning protocol across hospital facilities of all types. Consequently, emphasizing appropriate radiation doses in medical imaging technologist training curriculums and the employment of standardized CT scanning protocols involving appropriate adjustment of radiation dose and prevention of imaging technologist fatigue are promising strategies for reduction of occurrences of excess radiation exposure to children during the head CT scanning process. Our findings indicate that ensuring that technologists in adult hospitals are aware of the dangers of failing to adjust CT scanner settings for the patients age to ensure the lowest necessary dose of radiation is administered when scanning children is an effective method for ensuring children receive the appropriate dose of radiation.
It is important to consider factors in pediatric hospitals makes them less prone to administering excess radiation dose when compared to adult hospitals, and what factors in adult hospitals make them more prone to administering unnecessarily high radiation doses to pediatric patients. Pediatric and adult hospitals have two main differences in regard to head CT examinations. First, in pediatric hospitals, the range of radiation doses required is generally lower due to the smaller size of the patients, and CT scanning protocols are specifically designed for children. In contrast, adult hospitals typically have a wider range of radiation doses required, as they treat patients of varying sizes and may be more apt to not use the specialized protocols for pediatric patients and rather rely on automatic scanner settings.
Following standardized CT examination protocols for children will likely decrease radiation dose, according to our results. Across hospital systems, protocols for the CT scanning process vary. A study that reviewed CT head scans across 151 hospitals in seven countries and found that radiation doses between hospitals differed. The authors concluded that institutional decisions regarding technical parameters and operating procedures for CT scanners were important factors contributing to the level of radiation administered to patients [39]. CTDlvol can be used to optimize scan protocols and minimize patient radiation exposure while maintaining diagnostic image quality. Together, total exam DLP and CTDlvol measures are valuable indicators of radiation dose a patient is exposed to during the CT scanning process, and therefore, monitoring and comparing these metrics for CT scans performed within and between different institutions is of utmost importance in efforts targeted towards minimizing patient radiation exposure while maintaining diagnostic image quality.
Limitations of our study include focusing the review on head CT scans performed within hospital facilities in the Eastern United States. Specifically, all scans included in the study were performed within 8 hospitals within the same enterprise. All of the locations were supposed to be using the same age-based protocols. Although there were scans performed at multiple hospitals included in the study, it is possible that facilities in other regions of the nation have distinct head CT scanning protocols. Additionally, due to the lack of national standardization of head CT protocols, it is possible that the differences in radiation dose between adult and pediatric hospitals discovered in the present study are not present in other hospital systems. Further research is needed to better understand the factors contributing to the observed differences in radiation dose administration between adult and pediatric hospitals, and to develop strategies to mitigate the risk of excess radiation exposure in all healthcare settings.
In conclusion, the present study provides compelling evidence that pediatric patients undergoing CT head scans for both trauma and routine indications are at heightened risk for exposure to unnecessarily high radiation dose in adult hospitals compared to pediatric hospitals. The observed discrepancies have significant implications for the safety and health of children. To mitigate this risk and increase the safety of head CT scans for children, we recommend that institutions utilize standardized, age-based head imaging protocols for every child. The implications of these findings underscore the urgent need to address the issue of unnecessary radiation exposure to children in clinical practice. We hope the results of this study contribute to increased safety of head CT scans for children across the nation and beyond.
Data availability
The data gathered and analyzed in this study are available from the corresponding author on reasonable request.
Author contributions
J.L and L.H conceived the project, L.H performed a query to obtain CT head scans from PACS, J.Z, L.A., and L.H reviewed CT head scans and associated dose reports, J.L analyzed the results. All authors reviewed the manuscript.
Competing interests
The authors declare no competing interests.
References
- Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA 307 (2012): 2400-2409.
- Smith-Bindman R, Kwan ML, Marlow EC, et al. Trends in Use of Medical Imaging in US Health Care Systems and in Ontario, Canada, 2000-2016. JAMA 322 (2019): 843-856.
- Government Accountability Office. Report to congressional requesters: Medicare Part B imaging services: rapid spending growth and shift to physician offices indicated need for CMS to consider additional management practices [GAO-08-452]. https://www.gao.gov/new.items/d08452.pdf. Accessed June 3, 2019.
- Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA 307 (2012): 2400-2409.
- American College of Radiology. White Paper on Radiation Dose in Medicine. J Am Coll Radiol 4 (2007): 272-284.
- Quayle KS, Jaffe DM, Kuppermann N, et al. Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated? Pediatrics 99 (1997): E11.
- Perry TA, Ben-Yosef R, Kassirer JP. When patients decline recommended care. West J Med 144 (1986): 736-738.
- Sjöström S, Andersson T, Karlsson SA, et al. Attitudes towards radiological examinations and radiation risk among general practitioners in a Swedish county. Radiat Prot Dosimetry 148 (2011): 282-287.
- National Cancer Institute. Kids and radiation safety. https://www.cancer.org/latest-news/kids-and-radiation-safety.html. Accessed June 3, 2019.
- International Atomic Energy Agency. Radiation protection and safety of radiation sources: international basic safety standards. https://www-pub.iaea.org/MTCD/publications/PDF/Pub1136_web.pdf. Accessed June 3, 2019.
- Mettler FA Jr, Thomadsen BR, Bhargavan M, et al. Medical radiation exposure in the U.S. in 2006: preliminary results. Health Phys 95 (2008): 502-507.
- Ozasa K, Shimizu Y, Suyama A, et al. Studies of the mortality of atomic bomb survivors, report 14, 1950-2003: an overview of cancer and noncancer diseases. Radiat Res 177 (2012): 229.
- Kamiya K, Ozasa K, Akiba S, et al. Long-term effects of radiation exposure on health. Lancet 386 (2015): 469-478.
- Brenner AV, Tronko MD, Hatch M, et al. I-131 dose response for incident thyroid cancers in Ukraine related to the Chornobyl accident. Environ. Health Perspect 119 (2011): 933-939.
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources, Effects and Risks of Ionizing Radiation: United Nations Scientific Committee on the Effects of Atomic Radiation: UNSCEAR 2013 Report to the General Assembly with Scientific Annexes. UNSCEAR; Vienna, Austria (2013).
- Miglioretti DL, Johnson E, Williams A, et al. Population health burden of pediatric head CT examinations: Potential implications for policymakers. Pediatrics 137 (2016): e20154535.
- Karlsson P, Holmberg E, Lundell M, et al. Intracranial tumors after exposure to ionizing radiation during infancy: A pooled analysis of two Swedish cohorts of 28,008 infants with skin hemangioma. Radiat Res 150 (1998): 357-364.
- Khong PL, Ringertz H, Donoghue V, et al. ICRP publication 121: Radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP 42 (2013): 1-63.
- O'Connor JP, Aboagye EO, Adams JE, et al. Imaging biomarker roadmap for cancer studies. Nat Rev Clin Oncol 14 (2017): 169-186.
- Brenner DJ, Hall EJ. Computed tomography — An increasing source of radiation exposure. N Engl J Med 357 (2007): 2277-2284.
- Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361 (2009): 849-857.
- Cumulative radiation exposure and cancer risk from CT scans obtained during childhood and adolescence. Lancet Public Health 7 (2022): e188-e195.
- Radiation-induced DNA damage in pediatric patients undergoing CT scans. PLOS ONE 16 (2021): e0245346.
- Long-term cancer risk of children undergoing multiple CT scans: a national cohort study from Australia. BMJ Open 11 (2021): e042082.
- Pediatric CT and the associated risk of radiation-induced cancer: a systematic review and meta-analysis. J Radiol Prot 41 (2021): 555-576.
- Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380 (2012): 499-505.
- Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131 (2016): 803-820.
- Frush DP, Applegate KE. Radiologic imaging in pediatrics: justification, dose optimization, and risk communication. Radiology 259 (2011): 657-664.
- Santelli L, Baroncini S, D’Elia C, et al. Radiation doses and cancer risk in children undergoing interventional cardiology procedures. Int J Cardiol 303 (2020): 41-48.
- Paterson A, Frush DP, Donnelly LF. Helical CT of the body: Are settings adjusted for pediatric patients? Am J Roentgenol 176 (2001): 297-301.
- Image Gently. About Image Gently. https://www.imagegently.org/. Accessed April 26 (2023).
- Strauss KJ, Goske MJ. Image gently: a national education and communication campaign in radiology using the science of social marketing. J Am Coll Radiol 7 (2010): 969-974.
- Lee JH, Lim JS, Lee KS, et al. Optimization of pediatric head CT: decreased radiation dose without loss of image quality using iterative reconstruction. Am J Roentgenol 204 (2015): 397-402.
- Nigrovic LE, Schunk JE, Foerster A, et al. The effect of observation on cranial computed tomography utilization for children after blunt head trauma. J Am Coll Radiol 11 (2014): 971-978.
- Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361 (2009): 849-857.
- Mettler FA Jr, Bhargavan M, Faulkner K, et al. Radiologic and Nuclear Medicine Studies in the United States: Frequency and Radiation Dose. Radiology 253 (2009): 520-531.
- Dixon S. CT dose indices: understanding them, reducing them. Journal of Radiological Protection 36 (2016): R99-R116.
- Van der Merwe W, Pienaar R, Toit Hdu. After-hours CT examinations: Radiation dose and imaging quality. South African Journal of Radiology 23 (2019): a1635.
- Why do radiation doses for CT differ across hospitals and countries? (Professional Abstract). (2013). Available at: https://www.pcori.org/research-results/2013/why-do-radiation-doses-ct-differ-across-hospitals-and-countries#section_professional_abstract. (Accessed: 27th April 2023).
