Factors and Strategies for Poor Pain Relief after Vertebroplasty: A Literature Review
Article Information
Binbin Tang, Kang Liu, Xiaolin Shi, Yuliang Huang*
Department of Orthopedics, The Second Affiliated Hospital of Zhejiang Chinese Medical University (Xinhua Hospital of Zhejiang Province), Hangzhou, China.
*Corresponding Author: Yuliang Huang, Department of Orthopedics, The Second Affiliated Hospital of Zhejiang Chinese Medical University (Xinhua Hospital of Zhejiang Province), Hangzhou, China.
Received: 31 October 2022; Accepted: 08 November 2022; Published: 02 December 2022
Citation:
Tang B, Liu K, Shi X, Huang Y. Factors and Strategies for Poor Pain Relief after Vertebroplasty: A Literature Review. Journal of Orthopedics and Sports Medicine 4 (2022): 309-316.
Share at FacebookAbstract
Study Design: Literatures review
Objective: To search and review the causes and measures to Poor Pain Relief (PPR) after vertebroplasty for Osteoporotic Vertebral Compression Fractures (OVCFs) in short period postoperatively.
Summary of Background Data: Vertebroplasty are more and more common for OVCF patients. However, various treatments on postoperative residual pain have been reported heavily. The PPR has been disturbing many doctors and affects the symptoms of patients. Therefore, we reviewed relevant articles in an attempt to obtain meaningful evidence on factors and strategies for PPR.
Methods: We set the priority of comparatively observational clinical study for review. PubMed, Web of Science, Embase, CNKI, WanFang, and VIP were searched for the treatment of OVCFs with vertebroplasty and to evaluate the clinical efficacy.
Results: 817 references were electronically retrieved, 48 full-text papers were screened, and 36 studies were included. Seventeen trials presented factors for PPR, mainly including bone cement-related, operation-related and patient-related factors. Nineteen studies showed strategies for PPR, including anti-osteoporosis treatments, surgical operation improvement and addition of other therapies. 15 prospective, 19 retrospective and 2 meta-analyses comprised the systematic review. The quality of included studies was generally low, especially in some controlled studies with an unclear risk of bias.
Conclusions: Bone cement distribution and operative errors are main causes of PPR after vertebroplasty. Many therapeutic methods are available to relieve this pain and restore function but with sparse evidence. We still value and implement
Keywords
Poor pain relief; Vertebroplasty; Osteoporotic vertebral compression fractures; Bone cement; Zoledronic acid
Vertebroplasty articles Vertebroplasty Research articles Vertebroplasty review articles Vertebroplasty PubMed articles Vertebroplasty PubMed Central articles Vertebroplasty 2023 articles Vertebroplasty 2024 articles Vertebroplasty Scopus articles Vertebroplasty impact factor journals Vertebroplasty Scopus journals Vertebroplasty PubMed journals Vertebroplasty medical journals Vertebroplasty free journals Vertebroplasty best journals Vertebroplasty top journals Vertebroplasty free medical journals Vertebroplasty famous journals Vertebroplasty Google Scholar indexed journals Orthopedics articles Orthopedics Research articles Orthopedics review articles Orthopedics PubMed articles Orthopedics PubMed Central articles Orthopedics 2023 articles Orthopedics 2024 articles Orthopedics Scopus articles Orthopedics impact factor journals Orthopedics Scopus journals Orthopedics PubMed journals Orthopedics medical journals Orthopedics free journals Orthopedics best journals Orthopedics top journals Orthopedics free medical journals Orthopedics famous journals Orthopedics Google Scholar indexed journals Bone Mineral Density articles Bone Mineral Density Research articles Bone Mineral Density review articles Bone Mineral Density PubMed articles Bone Mineral Density PubMed Central articles Bone Mineral Density 2023 articles Bone Mineral Density 2024 articles Bone Mineral Density Scopus articles Bone Mineral Density impact factor journals Bone Mineral Density Scopus journals Bone Mineral Density PubMed journals Bone Mineral Density medical journals Bone Mineral Density free journals Bone Mineral Density best journals Bone Mineral Density top journals Bone Mineral Density free medical journals Bone Mineral Density famous journals Bone Mineral Density Google Scholar indexed journals Magnetic Resonance Image articles Magnetic Resonance Image Research articles Magnetic Resonance Image review articles Magnetic Resonance Image PubMed articles Magnetic Resonance Image PubMed Central articles Magnetic Resonance Image 2023 articles Magnetic Resonance Image 2024 articles Magnetic Resonance Image Scopus articles Magnetic Resonance Image impact factor journals Magnetic Resonance Image Scopus journals Magnetic Resonance Image PubMed journals Magnetic Resonance Image medical journals Magnetic Resonance Image free journals Magnetic Resonance Image best journals Magnetic Resonance Image top journals Magnetic Resonance Image free medical journals Magnetic Resonance Image famous journals Magnetic Resonance Image Google Scholar indexed journals Osteoporotic articles Osteoporotic Research articles Osteoporotic review articles Osteoporotic PubMed articles Osteoporotic PubMed Central articles Osteoporotic 2023 articles Osteoporotic 2024 articles Osteoporotic Scopus articles Osteoporotic impact factor journals Osteoporotic Scopus journals Osteoporotic PubMed journals Osteoporotic medical journals Osteoporotic free journals Osteoporotic best journals Osteoporotic top journals Osteoporotic free medical journals Osteoporotic famous journals Osteoporotic Google Scholar indexed journals Spine deformities articles Spine deformities Research articles Spine deformities review articles Spine deformities PubMed articles Spine deformities PubMed Central articles Spine deformities 2023 articles Spine deformities 2024 articles Spine deformities Scopus articles Spine deformities impact factor journals Spine deformities Scopus journals Spine deformities PubMed journals Spine deformities medical journals Spine deformities free journals Spine deformities best journals Spine deformities top journals Spine deformities free medical journals Spine deformities famous journals Spine deformities Google Scholar indexed journals Post-vertebroplasty articles Post-vertebroplasty Research articles Post-vertebroplasty review articles Post-vertebroplasty PubMed articles Post-vertebroplasty PubMed Central articles Post-vertebroplasty 2023 articles Post-vertebroplasty 2024 articles Post-vertebroplasty Scopus articles Post-vertebroplasty impact factor journals Post-vertebroplasty Scopus journals Post-vertebroplasty PubMed journals Post-vertebroplasty medical journals Post-vertebroplasty free journals Post-vertebroplasty best journals Post-vertebroplasty top journals Post-vertebroplasty free medical journals Post-vertebroplasty famous journals Post-vertebroplasty Google Scholar indexed journals Bone cement articles Bone cement Research articles Bone cement review articles Bone cement PubMed articles Bone cement PubMed Central articles Bone cement 2023 articles Bone cement 2024 articles Bone cement Scopus articles Bone cement impact factor journals Bone cement Scopus journals Bone cement PubMed journals Bone cement medical journals Bone cement free journals Bone cement best journals Bone cement top journals Bone cement free medical journals Bone cement famous journals Bone cement Google Scholar indexed journals Soft tissue injury articles Soft tissue injury Research articles Soft tissue injury review articles Soft tissue injury PubMed articles Soft tissue injury PubMed Central articles Soft tissue injury 2023 articles Soft tissue injury 2024 articles Soft tissue injury Scopus articles Soft tissue injury impact factor journals Soft tissue injury Scopus journals Soft tissue injury PubMed journals Soft tissue injury medical journals Soft tissue injury free journals Soft tissue injury best journals Soft tissue injury top journals Soft tissue injury free medical journals Soft tissue injury famous journals Soft tissue injury Google Scholar indexed journals Kyphoplasty articles Kyphoplasty Research articles Kyphoplasty review articles Kyphoplasty PubMed articles Kyphoplasty PubMed Central articles Kyphoplasty 2023 articles Kyphoplasty 2024 articles Kyphoplasty Scopus articles Kyphoplasty impact factor journals Kyphoplasty Scopus journals Kyphoplasty PubMed journals Kyphoplasty medical journals Kyphoplasty free journals Kyphoplasty best journals Kyphoplasty top journals Kyphoplasty free medical journals Kyphoplasty famous journals Kyphoplasty Google Scholar indexed journals Facet joint articles Facet joint Research articles Facet joint review articles Facet joint PubMed articles Facet joint PubMed Central articles Facet joint 2023 articles Facet joint 2024 articles Facet joint Scopus articles Facet joint impact factor journals Facet joint Scopus journals Facet joint PubMed journals Facet joint medical journals Facet joint free journals Facet joint best journals Facet joint top journals Facet joint free medical journals Facet joint famous journals Facet joint Google Scholar indexed journals Bone marrow edema articles Bone marrow edema Research articles Bone marrow edema review articles Bone marrow edema PubMed articles Bone marrow edema PubMed Central articles Bone marrow edema 2023 articles Bone marrow edema 2024 articles Bone marrow edema Scopus articles Bone marrow edema impact factor journals Bone marrow edema Scopus journals Bone marrow edema PubMed journals Bone marrow edema medical journals Bone marrow edema free journals Bone marrow edema best journals Bone marrow edema top journals Bone marrow edema free medical journals Bone marrow edema famous journals Bone marrow edema Google Scholar indexed journals Osteoporosis articles Osteoporosis Research articles Osteoporosis review articles Osteoporosis PubMed articles Osteoporosis PubMed Central articles Osteoporosis 2023 articles Osteoporosis 2024 articles Osteoporosis Scopus articles Osteoporosis impact factor journals Osteoporosis Scopus journals Osteoporosis PubMed journals Osteoporosis medical journals Osteoporosis free journals Osteoporosis best journals Osteoporosis top journals Osteoporosis free medical journals Osteoporosis famous journals Osteoporosis Google Scholar indexed journals Bone trabecular fractures articles Bone trabecular fractures Research articles Bone trabecular fractures review articles Bone trabecular fractures PubMed articles Bone trabecular fractures PubMed Central articles Bone trabecular fractures 2023 articles Bone trabecular fractures 2024 articles Bone trabecular fractures Scopus articles Bone trabecular fractures impact factor journals Bone trabecular fractures Scopus journals Bone trabecular fractures PubMed journals Bone trabecular fractures medical journals Bone trabecular fractures free journals Bone trabecular fractures best journals Bone trabecular fractures top journals Bone trabecular fractures free medical journals Bone trabecular fractures famous journals Bone trabecular fractures Google Scholar indexed journals Pain relief articles Pain relief Research articles Pain relief review articles Pain relief PubMed articles Pain relief PubMed Central articles Pain relief 2023 articles Pain relief 2024 articles Pain relief Scopus articles Pain relief impact factor journals Pain relief Scopus journals Pain relief PubMed journals Pain relief medical journals Pain relief free journals Pain relief best journals Pain relief top journals Pain relief free medical journals Pain relief famous journals Pain relief Google Scholar indexed journals
Article Details
Abbreviations:
PPR: Poor Pain Relief; OVCF: Osteoporotic Vertebral Compression Fracture; OP: Osteoporosis; PVP: Percutaneous Vertebroplasty; PKP: Percutaneous Kyphoplasty; BMD: Bone Mineral Density; MRI: Magnetic Resonance Image; ZOL: Zoledronic acid; PMMA: Polymethyl Methacrylate; MC-PMMA: Mineralized Collagen Polymethyl Methacrylate; ESWT: Extracorporeal Shock Wave Therapy
1. Introduction
The aging population is already a major social issue in the world today. The problem is mainly manifested by the increasing elderly people and following health problems. Osteoporosis (OP) is a common disease characterized by bone loss, bone strength decline and bone microstructure degeneration in the elderly. Osteoporotic Vertebral Compression Fracture (OVCF) is the most common complication and can lead to weight-bearing postures or spine deformities. This pain and deformity seriously affect their normal life. Conservative treatment or prolonged bed rest is not effective in relieving pain and sometimes even worsens it. With the development of spinal minimally invasive surgery, Percutaneous Vertebroplasty (PVP) and Percutaneous Kyphoplasty (PKP) have become useful and affective methods of treating OVCF. They can relieve pain immediately, facilitate functional activities and reduce other complications [1,2]. However, post-vertebroplasty patients with Poor Pain Relief (PPR) were frequently reported in literatures in the short period, usually three days after operation, even affecting their long-term follow-up.
At present, there are few reports on the causes and measures of poor pain relief in patients after vertebroplasty. Therefore, we want to systematically review the relevant literatures and obtain more and better answers to this question. The purpose of this article is to analysis and discusses factors and strategies for PPR after vertebroplasty from relevant studies.
2. Methods
2.1 Search strategy
We searched 6 databases including PubMed, Web of Science, Embase, CNKI, WanFang, and VIP in order to obtain more comprehensive results. We set the search terms as "Osteoporotic Vertebral Compression Fractures or OVCF" and "postoperative pain" and the retrieved literature was journal literature. The publication region and country was not limited, the language was English or Chinese and the publication period was from January 2016 to September 2020.
2.2 Inclusion criteria
817 literatures were retrieved. Firstly, 769 duplicate and irrelevant articles were removed based their titles and abstracts. Secondly, we removed 12 articles, 4 of which were simple reviews and 8 of which didn’t have English titles and abstracts. Finally, 36 studies were used for date extraction and discussion of results. According to the information from these studies, factors and strategies were categorized into three types. 17 articles reported relevant factors (bone cement related: 10, operation related: 3 and patient related: 4). 19 articles reported new strategies (anti-osteoporosis treatments: 8, surgical operation improvement: 6 and addition of other therapies: 5). 15 prospective, 19 retrospective and 2 meta-analyses together comprised the systematic review. The flow chart below can be seen clearly (Figure 1).
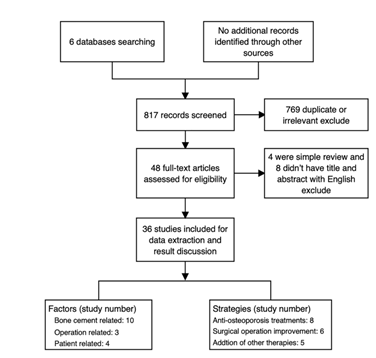
Figure 1: Flow chart of selection of related literatures review.
3. Results
3.1 Description of included studies
According to these 36 studies, we categorized and listed them in two Tables 1 and 2. In factor-related Tables 1 and 2, we set the items as Factor, Author/Year, Operation, Study Type and Better Pain Relief, which could be found in Table 1. The item of better pain relief is the probable cause of pain improvement. We set the items as Author/Year, Study Type, Test group, Control group and Better group, which could be found in Table 2. Better group means that better measure was taken.
3.2 Factors on Post-Vertebroplasty Poor Pain Relief (PPR)
The percentage of Post-Vertebroplasty Poor Pain Relief (PPR) ranges from 4-15% [3-5]. Considering elderly patients, only better pain and functional recovery will allow them to enjoy their late years. Several large-sample retrospective studies found that postoperative pain and bone mineral density, severe back soft tissue injury, bone cement features, lumbar facet joint violation, bone cement leakage or residual and others are mainly related [3-6], but no uniform understanding has been established. According to the current situation, we explored the causes of PPR mainly from three aspects: bone cement, operation and patient-related reasons from the literature search.
|
First Author/Year |
Operation |
Study Type |
Better Pain Relief |
Factor, No. |
|
Liu C [7], 2018 |
PVP |
Prospective |
Well distribution in the fracture line |
1 |
|
Ye L [8], 2018 |
PVP |
Retrospective |
Well distribution in the fracture line |
1 |
|
Liu H [9], 2019 |
PKP |
Retrospective |
Confluent distribution |
1 |
|
He S [10], 2019 |
PKP |
Retrospective |
“H” shape distribution |
1 |
|
Tan L [11], 2020 |
PVP |
Retrospective |
Distribution contacted both the upper and lower endplates |
1 |
|
Guo Z [12], 2017 |
PVP |
Prospective |
High viscosity |
2 |
|
Xu M [13], 2017 |
PVP |
Meta-analysis |
High viscosity |
2 |
|
F G [14], 2019 |
PVP |
Prospective |
No difference |
2 |
|
Li K [15], 2020 |
PVP |
Prospective |
No difference |
2 |
|
Miao F [16], 2020 |
PVP |
Prospective |
No difference |
2 |
|
Liu J [17], 2017 |
PVP |
Retrospective |
Low score in residual |
3 |
|
Yan S [18], 2017 |
PVP |
Retrospective |
Low score in residual |
3 |
|
Li Y [19], 2018 |
PKP |
Retrospective |
No violation |
4 |
|
Shen Y [20], 2016 |
PVP |
Retrospective |
Undeclined BMD |
5 |
|
Cao J [21], 2016 |
PVP |
Meta-analysis |
Normal BMD |
5 |
|
Peng K [22], 2018 |
PKP |
Retrospective |
No soft tissue injury on low back |
6 |
|
Xu W [23], 2018 |
PVP |
Prospective |
Moderate(25-75%)degree |
7 |
|
PVP: Percutaneous Vertebroplasty. PKP: Percutaneous Kyphoplasty. 1: Bone cement distribution 2: Bone cement viscosity 3: Pedicle Residual Bone Cement 4: Facet Joint Violation 5: Bone Mineral Density (BMD) 6: Soft Tissue Injury 7: Bone Marrow Edema |
||||
Table 1: Literatures List on the factors (bone cement-related, operation-related, patient-related) of poor pain relief.
|
Author/ Year |
Study type |
Test group |
Control group |
Better Group |
Strategy, No. |
|
Shi et al. [24], 2018 |
Retrospective |
PKP and ZOL |
PKP or ZOL |
Test group |
1 |
|
Huang et al. [25], 2019 |
Retrospective |
PKP and ZOL |
PKP Test group |
Test group |
1 |
|
Huang et al. [26], 2019 |
Prospective |
PKP and ZOL |
PKP |
Test group |
1 |
|
Zheng et al. [27], 2019 |
Prospective |
PKP and ZOL |
PKP |
Test group |
1 |
|
Hu et al. [28], 2020 |
Retrospective |
PVP, ZOL and Ca |
PVP and Ca |
Test group |
1 |
|
Huang et al. [29], 2020 |
Retrospective |
PVP,ZOL and VK2 |
PVP,Ca and VD |
Test group |
1 |
|
Li et al. [30], 2020 |
Retrospective |
PVP, ZOL and Rosuvastatin |
PVP and Ca |
Test group |
1 |
|
Kong et al. [31], 2019 |
Retrospective |
PKP and 12-month TPTD |
PKP, Ca and VD |
Test group |
1 |
|
Xu [32], 2018 |
Retrospective |
Bone filling bag vertebroplasty |
PKP |
No difference |
2 |
|
Yuan et al. [33], 2020 |
Prospective |
Low-dose targeted PVP |
Traditional PVP |
No difference |
2 |
|
Noriega et al. [34], 2019 |
Prospective |
TIVAD vertebroplasty |
PKP |
Test group |
2 |
|
Zhu et al. [35], 2019 |
Retrospective |
MC-PMMA cement PKP |
PMMA cement PKP |
Test group |
2 |
|
Wang et al. [36], 2018 |
Retrospective |
MC-PMMA cement PVP |
PMMA cement PVP |
No difference |
2 |
|
Jiang et al. [37], 2020 |
Retrospective |
MC-PMMA cement PVP |
PMMA cement PVP |
No difference |
2 |
|
Liu [38], 2019 |
Prospective |
Pregabalin |
/ |
Test group |
3 |
|
Li [39], 2020 |
Prospective |
ESWT |
Celecoxib Capsules oral |
Test group |
3 |
|
Du [40], 2019 |
Prospective |
Radiofrequency needle knife and Xianling Gubao capsules |
Radiofrequency needle knife |
Test group |
3 |
|
Li [41], 2019 |
Prospective |
Shentong Zhuyu decoction |
/ |
Test group |
3 |
|
Zhang [42], 2019 |
Prospective |
TCM five-tone therapy and Conventional treatment |
Conventional treatment |
Test group |
3 |
|
ZOL: Zoledronic acid. Ca: Calcium supplements. VK2: Vitamin K2. VD: Vitamin D. TPTD: Teriparatide. TIVAD: Titanium Implantable Vertebral Augmentation Device. PMMA: Polymethyl Methacrylate. MC: Mineralized Collagen. ESWT: Extracorporeal Shock Wave Therapy. TCM: Traditional Chinese Medicine. /: no therapy. 1: Improve osteoporosis. 2. Reform operation. 3. Add other therapies. |
|||||
Table 2: Literatures list on strategies (anti-osteoporosis treatments,surgical operation improvement and addition of other therapies) on poor pain relief.
3.3 Feasible strategies on Post-Vertebroplasty Poor Pain Relief (PPR)
By searching the literatures, we analyzed three main strategies on the pain relief after vertebroplasty. We discussed and analyzed them in terms of anti-osteoporosis treatments, surgical operation improvement and other therapies.
4. Discussion
4.1 Bone cement affecting pain relief
The mechanism by which the bone cement produces its effect is as follows. Bone trabecular fractures in the vertebral body are stabilized by the diffusion of bone cement to form a riveting effect, the axial pressure can be supported by filled bone cement, and the pain nerve endings will be damaged by thermal energy come from bone cement. Therefore, it is speculated that there is a possible relationship between the distribution of bone cement and postoperative residual pain. From 2018 to 2020, 5 articles [7-11] (1 prospective and 4 retrospective) with 2024 cases were retrieved for in-depth research about bone cement distribution. While the level of evidence in five articles is relatively low, important information has been extracted from these studies. More than 50% of vertebral bodies in the area of bone cement distribution get better pain and functional scores on the day after PVP [7]. Bone cement did not diffuse to the upper facture line, resulting in poor pain relief for 26 (11.6%) patients, which was reported by Ye et al [8]. One large samples study found that bone cement confluent distribution provided better pain relief than separated distribution if doctor used bilateral operation [9]. Similarly, He et al. [10] also found “H-shaped” distribution gained lower pain scores than "O-shaped" distribution. The distribution that touched upper and lower endplates showed better pain relief as well [11]. These above studies have explained that the distribution of bone cement is related to postoperative residual pain. More careful observation on the fracture line can ensure optimal bone cement diffusion.
In addition to the bone cement distribution, does the viscosity of bone cement affect the pain relief after vertebroplasty? Low viscosity is considered to be a main factor contributing to the leakage of bone cement, resulting in serious complications such as acute spinal cord or nerve root compression, paraplegia, cemented pulmonary embolism, and intervertebral disc degeneration [12-14]. It was reported that high-viscosity bone cement could reduce leakage and upgraded efficacy. While many studies have published results, it is unclear whether different bone cement viscosity affects pain relief after vertebroplasty. In recent years, four prospective studies [12,14-16] and one meta-analysis [12] on viscosity has been published with a high level of evidence. Of the 4 prospective studies, three articles came to the same conclusion that there was no significant difference in pain between high or low viscosity bone cement [14,15,16], and only one article concluded that higher viscosity bone cement resulted in better pain relief [12]. A meta-analysis of 6 RCT studies showed that high-viscosity bone cement was superior in terms of pain improvement, functional recovery and bone cement leakage, but not to the extent that pain relief developed. Therefore, high-viscosity bone cement cannot help pain better according to the current evidence. In a word, we believe that pain relief after vertebroplasty is closely related to the distribution of vertebral body. There is a controversy regarding the viscosity of the bone cement.
4.2 Operational way affecting pain relief
There were some literatures discussing the relationship between surgical operation and pain relief after vertebroplasty. At present, it has been demonstrated there is no difference between PKP and PVP in terms of pain relief and function recovery. And unilateral or bilateral percutaneous has no significance in the short term. Then, we found that improper operation probably affect the pain relief after vertebroplasty. In these studies, pedicle residual bone cement and facet joint violation were the two main factors affecting the pain relief [17-19]. Residual bone cement internal and external of pedicle was positively associated with pain relief in OVCF cases with vertebroplasty [17]. Facet joint invasion was found in patients who underwent unilateral PKP, and these patients had higher pain and dysfunction scores at a short-term follow-up of 1 month [19]. Pedicles rupturing were reported in earlier articles, as surgeon overdid the puncture angle, resulting in bone cement residue or leakage. Bone cement residual in the vicinity of fractured pedicle can lead to poor pain relief, which should be paid attention to. Puncturing repeatedly may damage the facet joint violation and other surrounding normal tissues, which should be avoided and considered as one reason for poor pain relief.
Another factor is the timing of surgery, but there is controversy at present. Yan et al. [18] believed pain relief was better when operation was performed within 1-3 weeks than when it was longer than 3 weeks [43], but another study found that no significant difference between operation within and beyond 4 weeks [44].
4.3 Patient-related reasons affecting pain relief
Four studies of Shen et al., Cao et al., Ke-jun, Xu et al. [20-23] reported the patient’s Bone Mineral Density (BMD), soft tissue injury and bone marrow edema were related to pain relief after vertebroplasty. BMD is the main factor affecting pain relief in the short or medium period. Lower BMD t value often represents higher visual analog scales of back pain [20,21]. The situation of soft tissue injury to the back or lumbar region can be found on MRI when vertebral compression fractures occur. Severe soft tissue injury has become an important factor affecting early pain relief. Peng K et al. reported the effect of soft tissue injury on pain relief and spine movement [22]. Xu W et al. reported that the best pain relief was obtained in 25-75% of bone marrow edema range on MRI [23]. However, we cannot obtain clear results from few reports.
4.4 Anti-osteoporosis treatment improving PPR
There have been few reports of unsatisfactory postoperative pain relief due to low bone density in recent years. However, many researchers regarded the zoledronic acid (ZOL) as the treatment for patients with severe osteoporosis who have residual pain after vertebroplasty. Zoledronic acid could inhabit osteoclasts differentiate and proliferate, regulate bone metabolism and reduce bone loss. Through searching, there were 6 retrospective studies [24-31] and 2 prospective studies [26,27]. 7 studies [24-29,31] reported the effect of ZOL and one study [31] reported the effect of Teriparatide.1416 cases, 574 cases in test group and 842 cases in control group, who had postoperative PPR were observed. The level evaluation of the 8 articles indicated relatively low evidence because of more retrospective studies. PVP combined with ZOL for postmenopausal OVCF patients showed better postoperative pain relief, BMD and osteocalcin expression than either PKP alone or ZOL alone [24-28]. On the basis of PVP and ZOL, osteosynthetic drugs, such as vitamin K2 [29], Statins [45,46] and Teriparatide [31] were also effective, with patients in the test group achieving better pain ease, functional recovery and fewer fractures. However, these studies were conducted with long-term follow-up results in the absence of postoperative pain score. Whether ZOL or other anti-osteoporosis drugs can improve the PPR after operation remains a question.
4.4 Surgical operation improvement improving PPR
While the operation of PKP or PVP combined with injection of Polymethyl Methacrylate (PMMA) bone cement has become an essential technique for surgeons, every technique needs to be improved for better clinical outcomes. Bone filled bag vertebroplasty, which is basically the same as PKP operation, is more effective in relieving pain [32]. Good bone cement distribution is considered as an important condition on good pain relief. Thus, Targeted puncture and low-dose bone cement was a new method proposed by Yuan L et al. [33], but there was no significant difference in pain relief at present stage in his study. SpineJack device technology was also a new operation reported by Noriega et al. [47] in 2015. Multi-center RCTs told us that this device had lower pain scores during follow-up 6 months after surgery and no earlier results [34]. We hope that more studies involving this device can give us meaningful results. Certainly, the improvements also have occurred with bone cement. It is reported that mineralized collagen Polymethyl Methacrylate (MC-PMMA) bone cement has better bioresorbability and biocompatibility [35-37]. In terms of pain relief after operation, MC-PMMA bone cement was not significantly different from regular bone cement [36,37]. Observing the 1-year follow-up, Zhu J et al. [35] found the Mineralized bone cement showed better pain relief and functional improvement. Other methods to improve short-term pain relief include the following. Vertebral anesthesia (into the vertebral body), reported by Mao G et al. [48] was better than conventional local anesthesia (to the surface of the periosteum) in terms of pain relief at 12h and 24h after operation. Ying et al. [49] considered the relationship between setting temperature of bone cement and residual pain, but there was insufficient evidence of pain relief.
4.5 Addition of other therapies improving PPR
This part aims to improve the PPR after vertebroplasty with a number of effective treatments. These included various therapies from western medicine and Chinese medicine, but the level of evidence is generally low. Pregabalin is an analgesic that provides good pain relief after PVP treatment with relative safety and certain efficacy [38]. Extracorporeal Shock Wave Therapy (ESWT) is an effective and physically acceptable treatment for postoperative pain, which was reported by Li et al. in 62 cases with PPR [39]. Chinese Medicine theory and therapy also play a significant role in the residual pain after vertebroplasty in OVCF patients, as demonstrated in the following studies. Xianling Gubao capsule is a proprietary Chinese medicine that improves bone density, promotes fracture healing, and effectively relieves osteoporotic pain. Du et al. [40] reported that Xianling Gubao capsules can effectively and quickly relieve lumbar and back pain. Another Chinese decoction called Shentong Zhuyu decoction was created by Wang Qingren, a famous doctor in the Qing Dynasty. Relative studies reported that Shentong Zhuyu decoction can accelerate the recovery from pain after operation by promoting the body’s absorption of blood stasis [41]. Chinese Medicine five-tone therapy organically combines the theory of the yin and yang and the five elements of TCM with music. It can regulate the patient's spirit, improve the function of patient’s internal organs and reduce pain after vertebroplasty [42,50,51]. All of these therapies mentioned above have shown beneficial clinical efficacy.
5. Conclusions
Although vertebroplasty has become the standard of the treatment for OVCF, postoperative pain relief varies among different patients. With the increase in OVCF and vertebroplasty, the issue of poor pain relief has attracted more attention. Therefore, this article reviewed and analyzed relevant factors and improvement strategies. It aims to summarize the latest research results and give guidance to doctors. We reviewed three common factors, including bone cement, surgical operation and patient’s problem. PPR is related to the distribution of bone cement. It is believed that the distribution of bone cement in the fracture region could relieve pain after operation. However, the nature of bone cement is not a factor.
Pedicle residual bone cement and facet joint violation should be aroused more attention during puncture. We believe that PPR in some patients stems from inappropriate technique.
Correspondingly, we reviewed three useful strategies, including improving osteoporosis, reforming surgical operation and adding other therapies. Currently, the application of anti-osteoporosis drugs, especially ZOL, has a positive effect on pain relief with fewer adverse effects, but it was not known for short-term pain. According to the studies on operational improvement, more follow-up is needed to confirm this and thus provide more evidence. As for other therapies, physical therapy and Chinese medicine treatment, etc. all has shown some efficacy. In our opinion, post-vertebroplasty poor pain relief is still a common problem. It is indispensable to first consider the cause of residual pain and then to choose a better strategy. In the end, we firmly believe that minimally invasive spine surgery should lead to better clinical efficacy in the near future.
Funding
This systematic review was supported by Zhejiang Province Natural Science Foundation (Grant No. LBY22H270005) and National Natural Science Foundation of China (Grant No. 82104891 and 82204829).
Conflict of Interest
Binbin Tang, Kang Liu, Xiaolin Shi and Yuliang Huang declare that they have no conflict of interest.
References
- Cao P, Hao W, Zhang L, et al. Safety and Efficacy Studies of Vertebroplasty with Dual Injections for the Treatment of Osteoporotic Vertebral Compression Fractures: Preliminary Report. Academic Radiology 27 (2020): e224-e231.
- Cheng J, Muheremu A, Zeng X, et al. Percutaneous vertebroplasty vs. balloon kyphoplasty in the treatment of newly onset osteoporotic vertebral compression fractures: A retrospective cohort study. Medicine 98 (2019): e14793.
- Wang K, Hai-yong Z, Wang Y, et al. Three methods for reducing back pain in older adult patients with age-related osteoporotic vertebral compression fractures of the thoracolumbar spine: protocol for a 2-year follow-up non-randomized controlled trial and preliminary results. Chinese Journal of Tissue Engineering Research 22 (2018): 3000-3004.
- Yang J-S, Liu J-J, Chu L, et al. Causes of Residual Back Pain at Early Stage After Percutaneous Vertebroplasty: A Retrospective Analysis of 1,316 Cases. Pain Physician 22 (2019): E495-E503.
- Li Y, Yue J, Huang M, et al. Risk factors for postoperative residual back pain after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. European Spine Journal (2020).
- Yang Junsong CH, Peng L, Tuanjiang L, et al. Causes of residual back pain at early stage after percutaneous vertebroplasty. Chin J Orthop 40 (2020): 625-634.
- Liu CZ, Ren CH, Jia BX, et al. Effect of bone cement distribution on aged osteoporotic vertebral body compression fractures. Journal of the American Geriatrics Society 66 (2018): S509.
- Ye LQ, Liang D, Jiang XB, et al. Risk factors for the occurrence of insufficient cement distribution in the fractured area after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Pain Physician 21 (2018): E33-E42.
- Liu H, Zhang J, Liang X, et al. Distribution Pattern Making Sense: Patients Achieve Rapider Pain Relief with Confluent Rather Than Separated Bilateral Cement in Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures. World Neurosurgery 126 (2019): E1190-E1196.
- He S, Zhang Y, Lv N, et al. The effect of bone cement distribution on clinical efficacy after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Medicine 98 (2019).
- Tan L, Wen B, Guo Z, et al. The effect of bone cement distribution on the outcome of percutaneous Vertebroplasty: a case cohort study. BMC Musculoskeletal Disorders 21 (2020).
- Guo Z, Wang W, Gao W, et al. Comparison the clinical outcomes and complications of high-viscosity versus low-viscosity in osteoporotic vertebral compression fractures. Medicine 96 (2017).
- Xu M, Zhang HS, Wang J, et al. A meta-analysis on percutaneous vertebroplasty with high-viscosity and low-viscosity bone cement for osteoporotic vertebral compression fractures. Chinese Journal of Tissue Engineering Research 21 (2017): 5571-5576.
- Genqiang F, Zhengli Z, Xianhui J, et al. Clinical efficacy of high viscosity bone cement vertebroplasty for treating osteoporotic vertebral compression fractures. Chinese Journal of Tissue Engineering Research 23 (2019): 3475-3480.
- Li K, Feng H, Luo D, et al. Efficacy and safety of high-viscosity cement in percutaneous vertebroplasty for treatment of Osteoporotic vertebral compression fractures: A retrospective cohort study. Medicine 99 (2020).
- Miao F, Zeng X, Wang W, et al. Percutaneous vertebroplasty with high- versus low-viscosity bone cement for osteoporotic vertebral compression fractures. Journal of Orthopaedic Surgery and Research 15 (2020).
- Liu J, Zhao Z, Li W. Analysis of correlation between the scores of residual bone cement and low back pain after percutaneous vertebroplasty in osteoporotic compression fractures. Biomedical Research-India 28 (2017): 7629-7632.
- Yan S, Wang X, Di J, et al. The study on the possible relationship between the residual bone cement in vertebral pedicle and the prognosis of osteoporotic vertebral compression fractures. International Journal of Clinical and Experimental Medicine 10 (2017): 9476-9481.
- Li Y, Huang M, Chen J, et al. The Impact of Facet Joint Violation on Clinical Outcomes after Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures. World Neurosurgery 119 (2018): E383-E388.
- Shen Y, Feng ML, Xu J, et al. Research of the effect of bone mineral density and fracture site of the vertebrae on low back pain in elderly patients with osteoporotic vertebral compression fractures. Zhonghua Yi Xue Za Zhi 96 (2016): 1818.
- Cao J, Kong L, Meng F, et al. Risk factors for new vertebral compression fractures after vertebroplasty: a meta-analysis. Anz Journal of Surgery (2016): 549-554.
- Ke-jun P. Influence of soft tissue injury on the pain relief and the time of exercise after PKP for thoracolumbar osteoporotic vertebral compression fractures. The Journal of Cervicodynia and Lumbodynia 39 (2018): 606-609.
- Xu W, Wang S, Chen C, et al. Correlation analysis between the magnetic resonance imaging characteristics of osteoporotic vertebral compression fractures and the efficacy of percutaneous vertebroplasty: a prospective cohort study. BMC Musculoskeletal Disorders 19 (2018).
- Shi C, Zhang M, Cheng AY, et al. Percutaneous kyphoplasty combined with zoledronic acid infusion in the treatment of osteoporotic thoracolumbar fractures in the elderly. Clinical Interventions in Aging 13 (2018): 853-861.
- Huang S, Zhu X, Xiao D, et al. Therapeutic effect of percutaneous kyphoplasty combined with anti-osteoporosis drug on postmenopausal women with osteoporotic vertebral compression fracture and analysis of postoperative bone cement leakage risk factors: a retrospective cohort study. Journal of Orthopaedic Surgery and Research 14 (2019).
- Huang Z-F, Xiao S-X, Liu K, et al. Effectiveness Analysis of Percutaneous Kyphoplasty Combined with Zoledronic Acid in Treatment of Primary Osteoporotic Vertebral Compression Fractures. Pain Physician 22 (2019): 63-68.
- Zheng H, Li H, Zhang J, et al. The effect of zoledronic acid combined with percutaneous kyphoplasty on the treatment of osteoporotic vertebral body compression fractures in patients. Journal of Biomaterials and Tissue Engineering 9 (2019): 1008-1013.
- Hu W, Wang H, Shi X, et al. Effect of Preoperative Zoledronic Acid Administration on Pain Intensity after Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fractures. Pain Research & Management 2020 (2020).
- Huang Y, Wu D. Clinical application of zoledronic acid combined with vitamin K2 in percutaneous vertebroplasty for multi-segment osteoporotic vertebral compression fractures. Zhongguo gu shang = China Journal of Orthopaedics and Traumatology 33 (2020): 820-826.
- Li H, Wang Y, Wang R, et al. Effects of rosuvastatin and zoledronic acid in combination on the recovery of senile osteoporotic vertebral compression fracture following percutaneous vertebroplasty. The Journal of International Medical Research 48 (2020).
- Kong M, Zhou C, Zhu K, et al. 12-Month Teriparatide Treatment Reduces New Vertebral Compression Fractures Incidence And Back Pain And Improves Quality of Life After Percutaneous Kyphoplasty In Osteoporotic Women. Clinical Interventions in Aging 14 (2019):1693-1703.
- Xu B, Wang X-F, Ye X-Y, et al. Observation of the clinical efficacy of the bone filling bag vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Zhongguo gu shang = China Journal of Orthopaedics and Traumatology 31 (2018): 993-997.
- Yuan L, Bai J, Geng C, et al. Comparison of targeted percutaneous vertebroplasty and traditional percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures in the elderly. Journal of Orthopaedic Surgery and Research 15 (2020).
- Noriega D, Marcia S, Theumann N, et al: A prospective, international, randomized, noninferiority study comparing an implantable titanium vertebral augmentation device versus balloon kyphoplasty in the reduction of vertebral compression fractures (SAKOS study). Spine Journal 19 (2019): 1782-1795.
- Zhu J, Zhang K, Luo K, et al. Mineralized Collagen Modified Polymethyl Methacrylate Bone Cement for Osteoporotic Compression Vertebral Fracture at 1-Year Follow-up. Spine 44 (2019): 827-838.
- Wang X, Kou JM, Yue Y, et al. Clinical outcome comparison of polymethylmethacrylate bone cement with and without mineralized collagen modification for osteoporotic vertebral compression fractures. Medicine 97 (2018).
- Jiang W, Geng W, Xu Y, et al. Application of mineralized collagen modified bone cement in the treatment of osteoporotic vertebral compression fractures. Chinese Journal of Tissue Engineering Research 24 (2020): 2381-2386.
- Yi LBZ. Therapeutic effect of pregabalin for the treatment of poor pain relief after percutaneous vertebroplasty. J Trauma Surg 21 (2019): 535-538.
- Xunbing LZNGZ. Experience of extracorporeal shock wave therapy for residual low back pain after vertebroplasty. Journal of North China University of Science and Technology (Health Sciences Edition) 22 (2020): 291-295.
- Xueyuan DXZ. Clinical observation of radiofrequency acupotomy combined with Xianling Gubao capsule for the treatment of senile osteoporotic vertebral compression fracture PVP postoperative pain. Tianjin Journal of Traditional Chinese Medicine 35 (2018): 590-593.
- Wuji LHX. Clinical observation on residual pain after PVP in the treatment of osteoporotic vertebral compression fracture with Jiawei Shentong Zhuyu decoction. Shanxi Chinese Medicine 40 (2019): 1545-1547.
- Benfu ZBT. The treatment of 35 cases of postoperative pain of vertebral compression fracture of osteoporosis with TCM five-tone therapy. Clinical Journal of Chinese Medicine 11 (2019): 123-126.
- Song-hai YJ-tYC-hZ. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fracture surgery and postoperative pain relief: retrospective study. Journal of Clinical and Experimental Medicine 16 (2017): 1832-1834.
- Zhou X, Meng X, Zhu H, et al. Early versus late percutaneous kyphoplasty for treating osteoporotic vertebral compression fracture: A retrospective study. Clinical Neurology and Neurosurgery 180 (2019): 101-105.
- Wang Z, Li Y, Zhou F, et al. Effects of Statins on Bone Mineral Density and Fracture Risk: A PRISMA-compliant Systematic Review and Meta-Analysis. Medicine (2016).
- Sendyk DI, Zindel Deboni MC, Mendes Pannuti C, et al. The influence of statins on osseointegration: a systematic review of animal model studies. Journal of Oral Rehabilitation (2016).
- David N, Gianluca M, Christian R, et al. Clinical Performance and Safety of 108 SpineJack Implantations: 1-Year Results of a Prospective Multicentre Single-Arm Registry Study. BioMed Research International 2015 (2015): 1-10.
- Mao G, Alemayehu DG, Yang Y, et al. The Effect of Intraoperative Vertebral Anesthesia on Osteoporotic Fractures Treated With Percutaneous Kyphoplasty A Prospective Cohort Study. Clinical Spine Surgery 32 (2019): E289-E296.
- Huiheng YJTTHBS. The effect of the application of artificial bone repair materials during percutaneous kyphoplasty operation on the bone cement setting temperature and postoperative. China Medicine 15 (2020): 1288-1291.
- Wang B, Zhao CP, Song LX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: A meta-analysis and systematic review. Journal of Orthopaedic Surgery and Research 13 (2018).
- Chen YC, Zhang L, Li EN, et al. Unilateral versus bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures in elderly patients: A meta-analysis. Medicine 98 (2019): e14317.
