Estimation of Disability-Adjusted Life Years among Patients Presenting with End-Stage Liver Disease
Article Information
Aizaz Khalid1, Umar Farooque2*, Tooba Laeeq1, Anoosh Farooqui3, Rizwan Farooque4, SM Ismail Shah5, Ali Mustafa1, Syed Adeel Hassan6, Mahwish Ahmed7, Nabeel Hussain8
1Department of Internal Medicine, Services Institute of Medical Sciences, Lahore, Pakistan
2Department of Neurology, Dow University of Health Sciences, Karachi, Pakistan
3Department of Internal Medicine, United Medical and Dental College, Karachi, Pakistan
4Department of Internal Medicine, Sindh Medical College, Karachi, Pakistan
5Department of Internal Medicine, Ziauddin Medical College, Karachi, Pakistan
6Department of Internal Medicine, University of Louisville, Louisville, USA
7Department of Internal Medicine, Islam Medical College, Sialkot, Pakistan
8Department of Basic Sciences, Saba University School of Medicine, Devens, USA
*Corresponding author: Umar Farooque, Department of Neurology, Dow University of Health Sciences, Karachi, Pakistan
Received: 12 February 2021; Accepted: 20 February 2021; Published: 1 March 2021
Citation:
Aizaz Khalid, Umar Farooque, Tooba Laeeq, Anoosh Farooqui, Rizwan Farooque, SM Ismail Shah, Ali Mustafa, Syed Adeel Hassan, Mahwish Ahmed, Nabeel Hussain. Estimation of Disability-Adjusted Life Years among Patients Presenting with End-Stage Liver Disease. Archives of Internal Medicine Research 4 (2021): 031-042.
Share at FacebookAbstract
Introduction: Disability-adjusted life years (DALYs) is a multidimensional metric utilized to quantify specific disease burdens. It has the potential to highlight both fatal and non-fatal outcomes of disease and thus help in policymaking and health resource allocation. Chronic liver disease, secondary to preventable causes, is one of the main contributors to morbidity and mortality. It demands the attention of researchers and policymakers alike. The primary aim of this study was to quantify the disease burden due to end-stage liver disease in terms of years of life lost (YLL), years lost to disability (YLD), and DALYs.
Materials and methods: This was a descriptive case-series study conducted over a period of six months between September 2019 and February 2020 at a tertiary care hospital in Lahore, Pakistan. All patients presenting with end-stage liver disease were interviewed. The YLL were predicted by using the Child-Pugh score’s estimation of years of life left. Chronic Liver Disease Questionnaire (CLDQ) was used to assess the disabilities of the patients along with disability weights from the Global Burden of Disease (GBD) study to calculate the YLD. All statistical analysis was conducted using Statistical Package for Social Sciences (SPSS) version 23.0.
Results: 18 patients who presented with end-stage liver disease had 32.8 (95% CI: 25.2-40.5) mean DALYs. The mean age of presentation was 51.1 (95%CI: 42.7-59.4) years. A significant negative correlation was found between age and DALYs (r=-0.94, p<0.001). The mean YLL was 31.5 (95%CI: 23.5-39.5) and the mean YLD was 1.34 (95%CI: 0.58-2.11). Most patients presented with decompensated chronic liver disease (DCLD) during the fifth and sixth decade of life. No significant correlation was found between gender and DALYs (r = 0.208, p=0.407).The most common adjusted disabilities were muscle cramps, fatigue, difficulty sleeping at night, h
Keywords
Disability-Adjusted Life Years, End-Stage Liver Disease, Years of Life Lost, Years Lost to Disability, Chronic Liver Disease
Disability-Adjusted Life Years articles; End-Stage Liver Disease articles; Years of Life Lost articles; Years Lost to Disability articles; Chronic Liver Disease articles
Article Details
1. Introduction
The disability-adjusted life years (DALYs) is a multidimensional metric that integrates the years of life lost (YLL) and the years lost to disability (YLD) due to mortality[1]. It can be effectively utilized to quantify the overall disease burden in society and helps to compare various diseases in addition to understanding the impact of demographics on the disease burden under investigation. It can be used to formulateglobal health policies and allocate resources efficiently by projecting and comparing various disease burdens. An internationally standardized form of the quality-adjusted life-years (QALYs) has been established for the global burden of disease names as the disability-adjusted life years (DALYs). DALYs can be used to express the years of lost to premature mortality and years lived with a disability of specified severity and duration. Hence, one DALY indicates one lost year of a healthy life. Premature mortality refers to death that takes place before the age to which the dying person could have expected to survive if they were a part of a standardized model population with a life expectancy at birth equal to that of the world’s longest-surviving population i.e. Japan[2].
Chronic Liver Disease (CLD) refers to a group of hepatic disorders usually leading to liver cirrhosis. Cirrhosis leads to a number of abnormalities like deficiencies of several proteins like clotting and anticoagulation factors etc.[3]. According to the World Health Organization (WHO) estimates, chronic diseases contribute to 46% of the global disease and 59% mortality. The number of people dying due to chronic diseases is about 35 million and it is steadily increasing[4]. End-stage liver disease is one of the main contributors to the overall disease burden in both the developing and the developed world leading to about two million deaths every year mainly due to cirrhosis and hepatocellular carcinoma[5, 6]. According to research analysis of the Global Burden of Disease (GBD) 2010 Study, cirrhosis of the liver ranks 23rdin the leading causes of disability-adjusted life years. Its contribution to the global disease burden has increased from 24.3 million in 1990 to more than 31 million in 2010, which represents a 27% increase in DALYs[7]. Liver disease affects 300 million people in Chinaand is the 11thleading cause of death in white males in the United States (US) making up 1.5% of the total deaths[5, 8]. In the United Kingdom (UK), liver disease is the fifth most common cause of death, according to the Office for National Statistics[5]. The major causative agents which lead to the manifestation of end-stage liver disease, however, are hepatitis B virus (HBV), hepatitis C virus (HCV), alcoholic liver disease (ALD) and non-alcoholic liver disease (NALD) as well as hepatocellular carcinoma (HCC)[5, 7]. The country-level differences in the disease morbidity and mortality reflect variations in the prevalence of risk factors[9-11]. According to the WHO, the prevalence of hepatitis B and C are greater in South East Asia (2-5% population affected by HBV) as compared to western countries (less than 1% affected by HBV)[12].
End-stage liver disease stands to be one of the preventable causes of death worldwide. The primary objective of this study is to estimate the DALYs of end-stage liver disease in patients and make a comprehensive quantification of the disease burden in terms of years lost due to disability. It can be effectively utilized to educate the people regarding the year lost due to the early demise of a patient who develops decompensated chronic liver disease (DCLD) and the amount of time these patients lose due to disability. A secondary aim was to determine the most common adjusted disabilities among patients suffering from DCLD. This step may enable policymakers to understand the severity of the problem in a better way and encourage more efficient public spending on health and the prevention of disease.
2. Materials and Methods
2.1 Study setting and design
This was a descriptive cross-sectional study conducted over a period of six months between September 2019 and February 2020 at a 1700 bed tertiary care hospital in the city of Lahore, Pakistan.
2.2 Sample size, inclusion and exclusion criteria
Patients aged 12 years and older admitted in hospital medicine wards were approached and assessed, irrespective of sex. A total of 18 patients fulfilled the criteria and were enrolled in the study. Patients with primary liver disease were evaluated. Child-Turcotte-Pugh Score (child criteria) was used for scoring the progression of liver disease[13]. Patients having scores ranging from 6-15 were eligible. Patients with diabetes mellitus and acquired immunodeficiency syndrome (AIDS) as co-morbidities and non-compliant patients were excluded. Patients who were not fully investigated for Child’s score i.e. serum albumin, international normalized ratio (INR), total bilirubin, ascites, and hepatic encephalopathy were also excluded.
2.3 Sampling technique and data collection
A purposive sampling technique was employed to collect data from all patients. A semi-structured questionnaire was developed with closed-ended multiple-choice questions using the Chronic Liver Disease Questionnaire (CLDQ) to determine the YLD. To ascertain the YLL, the Child-Pugh Score table was used to estimate the years of life left. After obtaining informed consent, the Child-Pugh score was evaluated to fulfill the inclusion criteria. The Child-Pugh score was calculated as indicated in Table1. The determination of ascites and hepatic encephalopathy was made by examining the patient file or by a senior medical officer. The most recent test reports were used. Reports older than three days were not considered.
2.4 Statistical analysis
All statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 23.0. The DALYs were calculated as:DALYs = YLL + YLD.
YLL was calculated as = age-specific life expectancy - estimated years of life remaining.
YLD was calculated as = disability weight x duration of disability (years).
The data obtained from the questionnaire was quantified
to evaluate the YLD, by using the disability weights from the 2013 GBD study[14]. Disability weights, which represent the magnitude of health loss associated with specific health outcomes, were used to calculate years lived with disability for these outcomes in a given population. The weights were measured on a scale from zero to one, where zero equals a state of full health and one equals death. The Child-Pugh grade was used to estimate years of life leftand this number was subtracted from the ideal age-specific life expectancy to give the YLL[15]. The age-specific life expectancy of Japan was used as ithas the highest life expectancy. The life table of GBD 2015 was used[16]. All categorical variables were presented as percentages and frequency while all continuous variables were documented as mean and standard deviation. Lastly, the Pearson correlation was employed to evaluate the possible association between continuous variables.
|
Measure |
1 point |
2 points |
3 points |
Units |
|
Bilirubin (total) |
<2 |
2-3 |
>3 |
mg/dl |
|
Serum albumin |
>3.5 |
2.8-3.5 |
<2.8 |
g/l |
|
INR |
<1.7 |
1.71-2.20 |
>2.20 |
no unit |
|
Ascites |
None |
Mild (diuretic-responsive) |
Severe (diuretic-refractory) |
no unit |
|
Hepatic encephalopathy |
None |
Grade I-II (or suppressed with medication) |
Grade III-IV (or refractory) |
no unit |
INR-International Normalized Ratio
Table1: Evaluation of Child-Turcotte-Pugh Score.
3. Results
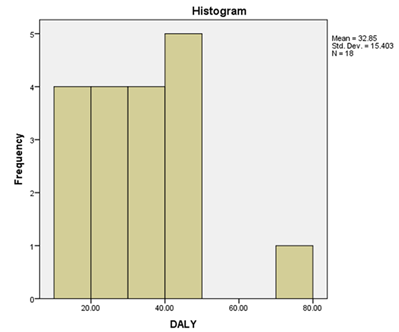
The mean DALYs of 18 patients was calculated. While there were large variations between the estimated DALY scores of the patients, the mean was 32.8 (95%CI: 25.2-40.5) with a standard deviation of 15.4. This means that every patient presented with end-stage liver disease symptomatology will lose around 32.8 (25.2-40.5) years of his life to the disease. The descriptive statistics of DALYs are presented in Table2. The total combined DALY of the 18 patients examined was estimated to be 591.22. The ideal life expectancy in Japan is reported to be 83.84. This implies that out of these 18 people, 7.05 lifetimes have been lost, which is 39.1%. If these values are projected as a percentage for better understanding, it means that if 100 people developed DCLD, it is as if 39 out of them never existed. Figure1shows that most of the DALY scores range between 10-50 years with a median of 34.08. The bar on the extreme right represents a case of decompensation at a very young agewhich has dramatically increased the DALY[17].
3.1 Composition of DALYs
DALYs were calculated as described by summing its two components, YLL and YLD. The relative share of these two variables was calculated in a total of 591.22 DALYs. The following results were obtained as shown in Table3. This indicates that most of the disease burden on the individual is due to the mortality associated with liver failure and not so much the morbidity. YLL constitutes 96% of the DALYs calculated. The total YLL from 18 patients was calculated as 567.07 whereas the mean YLL was 31.5 ± 3.8 (95% CI: 23.5-39.5). This means that patients presenting with DCLD lose a significant portion of their life due to their disease. The percentage share and the mean YLL also indicates that management of mortality should be the primary goal in the management of any patient that presents with symptoms of DCLD. The total YLD from 18 patients examined was 24.15 whereas the mean YLD was 1.34 (95% CI: 0.58-2.11) which means that each patient lost around 1.3 years as a consequence of their disease, according to the disability weights. As this constitutes around 4% of the total DALYs, it indicates the relatively mild nature of adjusted-disability as compared to other diseases. The GBD showed that the average contribution of YLD in DALY was 31.2%. The YLD for DCLD patients is far less than that average. The mean age of the patients was evaluated to be 51.1 ± 3.9 (95% CL: 42.7-59.4) years which means the clinical presentation of DCLD is common in the fifth and sixth decades of life.
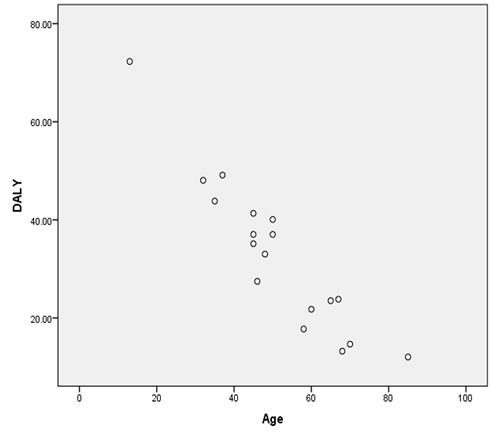
3.2 Association between age and DALYs
A significant negative relationship was found between
age and DALYs (r= -0.940)
3.3 Association between age, YLL and YLD
There is a significant negative correlation of age with YLL (r=-0.959, p<0.001) which means the years of life lost decrease as the age of presentation of DCLD increases. There is also a significant positive correlation of age with YLD (r=0.593, p=0.010) which means that the years lost due to disability increase as the age of presentation of DCLD increases. Lastly, a non-significant negative relationship was observed between YLD and YLL (r= -0.462, p=0.054).
3.4 Association between gender and DALYs
Out of the 18 patients, eight were male and 10 were females. No significant correlation was found between the DALYs and the gender of the patients (r = 0.208, p=0.407). This means that the disease affected both sexes equally in terms of the number of years affected by the disease.
3.5 Etiologies of liver disease among the patients
Out of the 18 patients that were evaluated, (n=16, 88.9%) were HCV positive while equal proportions (n=1, 5.6%) of patients were suffering from biliary cirrhosis and hepatitis A virus (HAV).
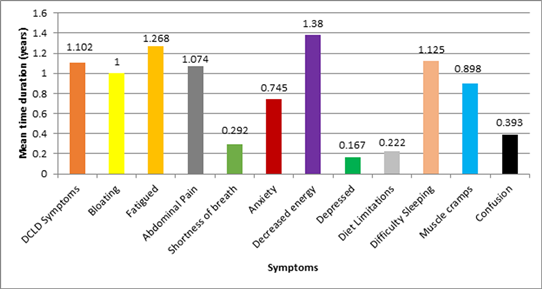
3.6 Frequency of duration of different clinical symptoms of DCLD
The patients were asked a total of 12 questions regarding the duration of their illness to determine the YLD. 11 patients out of 18 (61.1%) reported that they were suffering from symptoms of DCLD for less than one year as shown in Table4. The symptoms that they were inquired about were fluid in the abdomen, hematemesis, jaundice, or confusion associated with liver disease. The mean time duration of various clinical symptoms of DCLD is presented in Figure3. The disability was also ranked according to the meantime period of different clinical manifestations as shown in Table5. Symptomswere also ranked according to YLD as shown in Table6. The disability weight-adjusted ranking is different from the actual response ranking because disability weight ranking takes into account the intensity of symptoms and then generates the years of life lost due to disability accordingly. The top five contributors of mean YLD make 87.5% of the total mean YLD. The responses of our research questionnaire were correlated with the responses that were found upon the initial development of CLDQ[18]. There was a significant positive relationship between the proportion of patients complaining of symptoms in this study and the proportion of patients complaining of the same symptoms in the CLDQ study (r=0.751, p=0.020).
|
Measure |
Statistic |
Standard error |
|
Mean |
32.8454 |
3.63041 |
|
95% confidence interval for mean |
25.1859 (Lower) |
|
|
40.5049 (Upper) |
||
|
Median |
34.0808 |
|
|
Variance |
237.238 |
|
|
Standard deviation |
15.40253 |
|
|
Range |
60.24 |
|
|
Interquartile range |
21.19 |
Table2: Descriptive statistics of disability-adjusted life years.
DALY- Disability-Adjusted Life Year
|
Sum |
Percentage of DALY |
|
|
YLD |
24.15 |
4% |
|
YLL |
567.07 |
96% |
|
DALY |
591.22 |
100% |
YLD- Years Lost to Disability
YLL- Years of Life Lost
DALYs- Disability-Adjusted Life Years
Table 3: The relative share of YLD and YLL in total DALYs.
DALY- Disability-Adjusted Life Year
|
Question symptom |
Duration of symptom |
Frequency (n) |
Percent (%) |
|
DCLD |
2-6 months |
11 |
61.1 |
|
≥1 year |
7 |
38.9 |
|
|
Abdominal bloating |
None |
2 |
11.1 |
|
2-6 months |
11 |
61.1 |
|
|
≥1 year |
5 |
27.8 |
|
|
Fatigue |
None |
2 |
11.1 |
|
2-6 months |
9 |
50.0 |
|
|
≥1 year |
7 |
38.9 |
|
|
Abdominal pain |
None |
5 |
27.8 |
|
2-6 months |
10 |
55.6 |
|
|
≥1 year |
3 |
16.7 |
|
|
Shortness of breath |
None |
10 |
55.6 |
|
2-6 months |
7 |
38.9 |
|
|
≥1 year |
1 |
5.5 |
|
|
Anxiety |
None |
7 |
38.9 |
|
2-6 months |
7 |
38.9 |
|
|
≥1 year |
4 |
22.2 |
|
|
Decreased energy levels |
None |
1 |
5.6 |
|
2-6 months |
11 |
61.1 |
|
|
≥1 year |
6 |
33.3 |
|
|
Depression |
None |
7 |
38.9 |
|
2-6 months |
11 |
61.1 |
|
|
≥1 year |
0 |
0 |
|
|
Diet limitation |
None |
5 |
27.8 |
|
2-6 months |
13 |
72.2 |
|
|
≥1 year |
0 |
0 |
|
|
Sleeping difficulty |
None |
3 |
16.7 |
|
2-6 months |
11 |
61.1 |
|
|
≥1 year |
4 |
22.2 |
|
|
Muscle cramps |
None |
8 |
44.4 |
|
2-6 months |
6 |
33.3 |
|
|
≥1 year |
4 |
22.2 |
|
|
Trouble concentrating |
None |
13 |
72.2 |
|
2-6 months |
5 |
27.8 |
|
|
≥1 year |
0 |
0 |
DCLD- Decompensated Chronic Liver Disease
Table4: Frequency of duration of different clinical symptoms.
DCLD- Decompensated Chronic Liver Disease
|
Ranking |
Question symptom |
Mean duration (years) |
|
1st |
Decreased level of energy |
1.380 |
|
2nd |
Tired and fatigued |
1.268 |
|
3rd |
Difficulty sleeping at night |
1.125 |
|
4th |
Symptoms of DCLD |
1.102 |
|
5th |
Abdominal pain |
1.074 |
|
6th |
Bloating |
1.000 |
|
7th |
Muscle cramps |
0.898 |
|
8th |
Felt anxious |
0.745 |
|
9th |
Concentration problems |
0.393 |
|
10th |
Shortness of breath |
0.292 |
|
11th |
Limitations of diet |
0.222 |
|
12th |
Unhappy or depressed |
0.167 |
DCLD- Decompensated Chronic Liver Disease
Table 5: Ranking of symptoms according to mean time duration.
|
Ranking |
Question symptom |
Mean YLD |
|
1st |
Muscle cramps |
0.285 |
|
2nd |
Tired and fatigued |
0.278 |
|
3rd |
Difficulty sleeping at night |
0.246 |
|
4th |
Symptoms of DCLD |
0.196 |
|
5th |
Abdominal pain |
0.155 |
|
6th |
Limitations of diet |
0.054 |
|
7th |
Decreased Level of energy |
0.043 |
|
8th |
Unhappy or depressed |
0.024 |
|
9th |
Felt anxious |
0.022 |
|
10th |
Concentration problems |
0.017 |
|
11th |
Bloating |
0.011 |
|
12th |
Shortness of breath |
0.011 |
YLD- Years Lost to Disability
DCLD- Decompensated Chronic Liver Disease
Table 6: Ranking of questions according to YLD.
4. Discussion
DALYs provide a quantitative understanding of the loss suffered by liver disease patients that eventually end up with a decompensated liver disease.The mean DALY lost in our study was 32.8 (95% CI: 25.2-40.5), which makes up a large proportion of a patient’s life. At the same time, hepatitis C infection was found in 88.9% of our patients. Chronic hepatitis C makes up 40% of the global deaths due to cirrhosis in the Asia-pacific region[19]. High rates of infection are due to therapeutic injections, re-usable syringes, and unscreened blood transfusions in the healthcare setup. Chronic hepatitis C patients are mostly asymptomatic and are found to be HCV-positive when screened for blood donation. In one cross-sectional study on 959,281 donors, 695 had anti-HCV, which showed evidence of HCV infection. 74% of those with anti-HCV were ribonucleic acid (RNA)[20].YLL contributes an overwhelming 96% of the total DALY.
In 2017, one study on the global burden of disability estimated 62.16million DALYs from the chronic liver disease[21]. The significant loss of life that is attributed to DCLD can be effectively reduced by ensuring universal vaccination of hepatitis B and taking precautions to prevent the spread of HCV such as screening of blood donors at a national level, provision of new needles and syringes, treating substance use, etc. Health interventions to decrease and control viral hepatitis would cut down the burden of DCLD and reduce the total life years lost to this disease by the community.
The management of almost all patients with DCLD is conservative in nature. Early diagnosis and treatment should help reduce the disease burden and prevent its progression. Liver transplantation is a definite life-saving treatment option[22]. Research shows significant improvements in the survival of patients that receive liver transplantation after they have entered later stages of DCLD[23]. Muscle cramps, fatigue, difficulty sleeping at night, hematemesis, jaundice, fluid in the abdomen, and abdominal pain constitute about 90% of the disability associated with decompensated liver disease. Effectively managing these symptoms will go a long way towards improving the quality of life of patients of DCLD and reducing the disability associated with the disease. If the medical treatment is geared towards managing and reducing the most debilitating symptoms along with slowing and reversing the progress of the disease, it would have an impact on the YLD and ultimately, the DALY of these patients. Composite indicators, such as DALY is a multipurpose tool for health planning that allows more transparency in showing the impacts of mortality and morbidity of diseases. Thus, health outcomes are potentially highlighted with the aim of making better health-related decisions. Developing countries can have an increased burden of chronic diseases; therefore, an awareness of the gaps in health information is probable with the use of DALY, posing new challenges for the national health system[24].
5. Conclusions
The CLDQ was originally intended to calculate the quality of life in the short term (two weeks). However, in this study, the patients complained of nine disability parameters in similar percentages to the original CLDQ study. It, therefore, shows that the CLDQ is not only accurate in predicting short-term but also long-term disability.
References
- Bonita R, Beaglehole R, Kjellstrom T. Basic epidemiology. World Health Organization (2006).
- Murray, Christopher JL, Lopez, et al. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020 : summary. Christopher JL, Murray, Alan D, Lopez, World Health Organization (ed). Harvard School of Public Health on behalf of the World Health Organization and the World Bank, Boston, MA (1996).
- Omer Sultan M, Farooque U, Inam Khan M, et al. Frequency of venous thromboembolism in patients with liver cirrhosis. Cureus 12 (2020): e9594.
- Bengmark S. Curcumin, an atoxic antioxidant and natural NFκB, cyclooxygenase-2, lipo-oxygenase, and inducible nitric oxide synthase inhibitor: a shield against acute and chronic diseases. JPEN J Parenter Enteral Nutr 30 (2006): 45-51.
- Wang FS, Fan JG, Zhang Z, et al. The global burden of liver disease: the major impact of China. Hepatology 60 (2014): 2099-2108.
- Tauseef A, Zafar M, Rashid B, et al. Correlation of fasting lipid profile in patients with chronic liver disease: a descriptive cross-sectional study in tertiary care hospital. Cureus 12 (2020): e11019.
- Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 380 (2012): 2197-2223.
- Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep 65 (2016): 1-96.
- Office for National Statistics. Release calendar (2016).
- Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet 367 (2006): 52-56.
- Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 12 (2014): 145.
- World Health Organization. Hepatitis B (2020).
- The World Bank. The World Bank in Pakistan (2020).
- World Health Rankings. Health Profile: Pakistan (2018).
- Pakistan: WHO and UNICEF estimates of immunization coverage: 2015 revision (2015).
- Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 98 (2003): 1209-1228.
- World Health Rankings. Pakistan: Life Expectancy (2018).
- Younossi Z, Guyatt G, Kiwi M, et al. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut 45 (1999): 295-300.
- Sarin SK, Kumar M, Eslam M, et al. Liver diseases in the Asia-Pacific region: a lancet gastroenterology & hepatology commission. Lancet Gastroenterol Hepatol 5 (2020): 167-228.
- Murphy EL, Fang J, Tu Y, et al. Hepatitis C virus prevalence and clearance among U.S. blood donors, 2006-2007: associations with birth cohort, multiple pregnancies and body mass index. J Infect Dis 202 (2010): 576-584.
- Paik JM, Golabi P, Younossi Y, et al. The growing burden of disability related to non-alcoholic fatty liver disease: data from global burden of disease 2007-2017. Hepatol Commun (2020).
- Ekpanyapong S, Reddy KR. Hepatitis C virus therapy in advanced liver disease: outcomes and challenges. United European Gastroenterol J 7 (2019): 642-650.
- Merion RM, Schaubel DE, Dykstra DM, et al. The survival benefit of liver transplantation. Am J Transplant 5 (2005): 307-313.
- Hyder AA, Morrow RH. Applying burden of disease methods in developing countries: a case study from Pakistan. Am J Public Health 90 (2000): 1235-1240.