Esthetic Approach for Treatment of Molar Incisor Hypomineralization: A Case Report
Article Information
Renata Pereira*
Department of Restorative Dentistry, Piracicaba Dental School, University of Campinas, Piracicaba, Brazil
*Corresponding Author: Renata Pereira, Department of Restorative Dentistry, Piracicaba Dental School, University of Campinas, Piracicaba, SP 13.414-903
Received: 11 September 2019; Accepted: 27 September 2019; Published: 04 November 2019
Citation: Renata Pereira. Esthetic Approach for Treatment of Molar Incisor Hypomineralization: A Case Report. Dental Research and Oral Health 2 (2019): 062-072.
Share at FacebookAbstract
Stains and irregularities on tooth surfaces are factors that often lead patients to seek dental treatments to improve their smile aesthetics. Among these lesions, one may cite Molar Incisor Hypomineralization (MIH). MIH is a lesion of hypomineralization of systemic origin, in which up to four first permanent molars may be affected, concomitantly or not with incisors. This case report aims to describe the step-by-step of a treatment of MIH on left maxillary central incisor of a young patient. Accordingly, a direct restoration was performed with conventional composite resin, allowing the reestablishment of aesthetics and function, significantly influencing the self-esteem and quality of life of the patient.
Hypomineralization articles Hypomineralization Research articles Hypomineralization review articles Hypomineralization PubMed articles Hypomineralization PubMed Central articles Hypomineralization 2023 articles Hypomineralization 2024 articles Hypomineralization Scopus articles Hypomineralization impact factor journals Hypomineralization Scopus journals Hypomineralization PubMed journals Hypomineralization medical journals Hypomineralization free journals Hypomineralization best journals Hypomineralization top journals Hypomineralization free medical journals Hypomineralization famous journals Hypomineralization Google Scholar indexed journals ameloblasts articles ameloblasts Research articles ameloblasts review articles ameloblasts PubMed articles ameloblasts PubMed Central articles ameloblasts 2023 articles ameloblasts 2024 articles ameloblasts Scopus articles ameloblasts impact factor journals ameloblasts Scopus journals ameloblasts PubMed journals ameloblasts medical journals ameloblasts free journals ameloblasts best journals ameloblasts top journals ameloblasts free medical journals ameloblasts famous journals ameloblasts Google Scholar indexed journals amelogenesis articles amelogenesis Research articles amelogenesis review articles amelogenesis PubMed articles amelogenesis PubMed Central articles amelogenesis 2023 articles amelogenesis 2024 articles amelogenesis Scopus articles amelogenesis impact factor journals amelogenesis Scopus journals amelogenesis PubMed journals amelogenesis medical journals amelogenesis free journals amelogenesis best journals amelogenesis top journals amelogenesis free medical journals amelogenesis famous journals amelogenesis Google Scholar indexed journals enamel hypoplasia articles enamel hypoplasia Research articles enamel hypoplasia review articles enamel hypoplasia PubMed articles enamel hypoplasia PubMed Central articles enamel hypoplasia 2023 articles enamel hypoplasia 2024 articles enamel hypoplasia Scopus articles enamel hypoplasia impact factor journals enamel hypoplasia Scopus journals enamel hypoplasia PubMed journals enamel hypoplasia medical journals enamel hypoplasia free journals enamel hypoplasia best journals enamel hypoplasia top journals enamel hypoplasia free medical journals enamel hypoplasia famous journals enamel hypoplasia Google Scholar indexed journals mandibular molars articles mandibular molars Research articles mandibular molars review articles mandibular molars PubMed articles mandibular molars PubMed Central articles mandibular molars 2023 articles mandibular molars 2024 articles mandibular molars Scopus articles mandibular molars impact factor journals mandibular molars Scopus journals mandibular molars PubMed journals mandibular molars medical journals mandibular molars free journals mandibular molars best journals mandibular molars top journals mandibular molars free medical journals mandibular molars famous journals mandibular molars Google Scholar indexed journals periodontal articles periodontal Research articles periodontal review articles periodontal PubMed articles periodontal PubMed Central articles periodontal 2023 articles periodontal 2024 articles periodontal Scopus articles periodontal impact factor journals periodontal Scopus journals periodontal PubMed journals periodontal medical journals periodontal free journals periodontal best journals periodontal top journals periodontal free medical journals periodontal famous journals periodontal Google Scholar indexed journals incisor articles incisor Research articles incisor review articles incisor PubMed articles incisor PubMed Central articles incisor 2023 articles incisor 2024 articles incisor Scopus articles incisor impact factor journals incisor Scopus journals incisor PubMed journals incisor medical journals incisor free journals incisor best journals incisor top journals incisor free medical journals incisor famous journals incisor Google Scholar indexed journals gingival articles gingival Research articles gingival review articles gingival PubMed articles gingival PubMed Central articles gingival 2023 articles gingival 2024 articles gingival Scopus articles gingival impact factor journals gingival Scopus journals gingival PubMed journals gingival medical journals gingival free journals gingival best journals gingival top journals gingival free medical journals gingival famous journals gingival Google Scholar indexed journals
Article Details
1. Introduction
Several factors may compromise smile aesthetics, including molar incisor hypomineralization, which may alter the surface of dental enamel if its formation is interfered. Enamel formation, in brief, consists of 3 stages: matrix formation, when proteins involved in amelogenesis are produced; calcification, when mineral deposition occurs and most proteins are removed; and maturation, when the newly mineralized enamel finishes its calcification and the remaining protein is removed [1]. When some cause violently interferes with the metabolism of ameloblasts, they are severely disturbed and their functional activity is interrupted in that specific teeth formation stage [2-4]. The result is an expression of a pathological amelogenesis, in other words, an enamel development lesion. The main enamel development lesions are hypoplasia, hypocalcification or hypomineralization [5]. One may consider that hypoplasia occurs because of a disorder in the organic matrix formation. In this case, the lesion is manifested through pits, grooves or even total absence of enamel [4, 5]. Hypocalcification or hypomineralization, however, occurs due to disturbance in the maturation and calcification of enamel, expressing, therefore, as opaque areas on normal enamel surfaces, without loss of substrate volume [5].
Molar incisor hypomineralization was first defined by Weerheijm et al., as a lesion of hypomineralization of systemic origin, in which up to four first permanent molars are affected, concomitantly or not with incisors [6]. In such cases, opacities are usually limited to the occlusal/incisal third of the crown, most commonly on buccal surfaces [7]. Moreover, the enamel surface is generally soft and porous, once ameloblasts are affected during the early phase of amelogenic maturation [7, 8]. Although the etiological factors of molar incisor hypomineralization are not fully defined in the literature, studies suggest that troubles during pregnancy, natal and neonatal period, such as maternal illness, caesarean delivery, delivery complications, prematurity, and low birth weight may play an important role on molar incisor hypomineralization emergence [9, 10]. Likewise, illnesses on early childhood, including respiratory diseases, fever, hospitalization, and antibiotic therapy may represent causes for development of such lesion [9, 11]. A correct diagnosis of molar incisor hypomineralization, minding to etiological factor, excludes differential diagnoses, such as initial caries lesion, enamel hypoplasia, fluorosis or amelogenesis imperfecta. Additionally, an incisive diagnosis allows the correct management of the clinical case, restoring the patient's function and aesthetics, significantly influencing the patient’s overall oral health, self-esteem and quality of life. The aim of this case report is to describe an esthetic treatment with resin composite for a young patient diagnosed with molar incisor hypomineralization.
2. Case Report
A female patient, LFGF, 13 years old, attended a dental appointment at Piracicaba Dental School – University of Campinas, complaining about the esthetic of her left maxillary central incisor. During anamnesis, the patient's legal guardian mentioned that the patient was recently diagnosed with depression’s onset. Nevertheless, the patient did not use any medication. Except for depression, her overall health was stable, and her previous general health history indicated only throat and ear infections in early childhood. When questioned, the patient's legal guardian was unable to report other possible natal or neonatal diseases presented by the patient in her first year of life, as well as complications experienced by her mother during pregnancy or childbirth. Clinical exam revealed a yellowish white spot on the buccal surface of her left maxillary central incisor, disharmonizing her smile and drawing attention to the affected tooth (Figure 1). In lateral view, one may note that enamel’s texture of left maxillary central incisor did not change substantially, presenting only a discreet pit (Figure 2). Still in clinical exam, it was observed not only a spot on left maxillary central incisor, but also on buccal face of the right maxillary central incisor, as well as on mandibular incisors, canines, premolars, and maxillary and mandibular molars (Figure 3). Molar lesions strongly indicated molar incisor hypomineralization. Right maxillary first molar, specifically, presented a delimited yellowish groove, which began at the mesial buccal cusp and extended to the cervical third of the tooth. Right mandibular first molar, on the other hand, was restored. The composite restoration, badly adapted and with gaps, was located at occlusal third of the tooth, where possibly there was previously a hypomineralization lesion as well (Figure 4A). The molars of other hemiarch presented diffuse whitish lesions, but no loss of structure (Figure 4B). Radiographic images showed no periodontal, periapical or caries lesions. Additionally, mucosa was relatively healthy, as well as the other teeth.
After analyzing the patient's anamnesis and clinical examination, and after discussing all differential diagnoses of her lesions, the practitioners diagnosed the affected teeth as a case of molar incisor hypomineralization, although the lesions etiological factor was uncertain. To define the treatment plan, the depth of the spots was estimated by transillumination. A light emitting diode device (Radii-cal, SDI Limited, Bayswater, VIC, Australia) was placed on palatal surfaces of the affected teeth and the lesions darkening was analyzed, so that the more opaque the injury was, the deeper it was considered, and the greater the likelihood that the dentin was affected. As one may observe in (figure 5), the opacity of the left maxillary central incisor lesion confirmed the injury’s depth and the involvement of dentin tissue. Thus, more conservative treatments, such as bleaching and/or microabrasion, were discarded from the treatments’ possibilities. Considering the patient's age, the treatment offered to the patient was, then, direct restoration with composite resin. Since the patient had onset of depression, it was suggested that treatment began with restoration of left maxillary central incisor, in an attempt to possibly improve the patient's self-esteem and mental health.
Initially, with the teeth clean and moist, and under appropriate fluorescent light (5500 K), the enamel and dentin shade was selected with a color scale (Vita Classical, Vita Zahnfabrik, Bad Säckingen, Germany) (Figure 6). After shade selection, operatory field was properly isolated with rubber dam (Figure 7A). The left maxillary central incisor spot was then abraded 2 to 3 mm with a spherical carbide bur (#5, FG, Microdont, São Paulo, SP, Brazil) until the outermost surface of the stain was completely removed (Figure 7B). Then, in order to mask the interface between tooth and restoration, a bevel of approximately 2 mm was confectioned with a #3118F fine diamond bur (KG Sorensen, Cotia, SP, Brazil) (Figures 7C and 7D). Prior to composite restoration procedure, adjacent teeth were protected with polytetrafluorethylene-based tape (Isotape, TDV Dental, Pomerode, SC, Brazil) (Figure 8A). The cavity was then etched with 35% phosphoric acid (Ultra-Echt, Ultradent Products, South Jordan, UT, USA) up to 1 mm beyond the preparation margin (Figure 8B), for 20 seconds, washed for the same period (Figure 8C) and air dried, protecting dentin with a moist cotton wool. A layer of adhesive system (Adper Single Bond 2, 3M Oral Care, St. Paul, MN, USA) was applied to all cavity surfaces (Figure 8D), following manufacturer's instructions, and it was light activated for 10 seconds by light emitting diode device (Figure 8E). IPS Empress Direct composite system (Ivoclar Vivadent AG, Schaan, Liechtenstein) was used for restorative treatment (Figure 9). Shades A2E and A2DE were selected for enamel and dentin, respectively, and were applied to cavity through stratification technique. The opaque A2DE composite restored the affected dentin, reestablishing anatomical structures, such as dentin mamelons, while the translucent A2E composite was applied on the outer layer, replicating the enamel optical properties. Each composite increment was light activated for 20 seconds. Rubber dam was removed and initial finishing was performed with extra fine diamond burs.
Finally, in the subsequent session, restoration surfaces were polished with aluminum oxide polishing discs (Sof-Lex contouring and polishing discs, 3M Oral Care) (Figures 10A and 10B), abrasive silicone tips (Optimize, TDV Dental, Pomerode, SC, Brazil), and felt discs with diamond paste (Diamond Excel, FGM Produtos Odontológicos, Joinville, SC, Brazil) (Figure 10C). Also, finishing strips (Sof-Lex Finishing Strips, 3M Oral Care) were applied to mesial surface in order to remove any composite excess, improve the contour and polish proximal area of restoration (Figure 10D). As a result, the tooth’s natural structure was successfully reproduced (Figure 11). The patient was pleased with the result of restoration and new smile obtained. After completion of left maxillary central incisor restoration, the rest of the treatment consisted of restoring the right maxillary and mandibular molars also with conventional composite resin. The patient's family, however, preferred to continue the treatment at a private clinic, once Piracicaba Dental School was located far from her residence. Although the treatment was not completed, the concern about the aesthetics of the patient's smile was solved, positively affecting the patient's self-esteem and mental health.
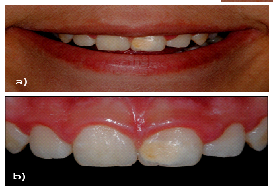
Figure 1: Preoperative images. (a) Patient’s initial smile; (b) Anterior maxillary teeth.
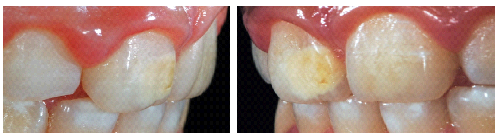
Figure 2: Lateral view of left maxillary central incisor, revealing a discreet pit on tooth’s incisal third.

Figure 3: General intraoral view, revealing white spots on buccal surface of several teeth.
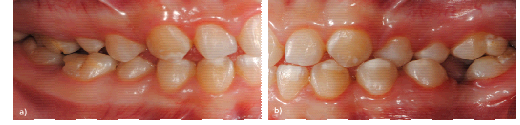
Figure 4: Lateral view of occluded teeth, revealing enamel defects on molars. (a) Right hemiarch presenting yellowish lesions on the buccal surface of molars; (b) Left hemiarch presenting diffuse whitish lesions on the buccal surface of molars.
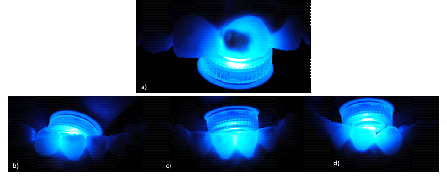
Figure 5: Transillumination of enamel defects. (a) Transillumination of left maxillary central incisor, revealing a deep depth lesion; (b) Transillumination of right mandibular canine and lateral incisor, revealing a medium depth lesion; (c) Transillumination of mandibular central incisors, revealing a shallow depth lesion; (d) Transillumination of left mandibular lateral incisor and canine, revealing a shallow depth lesion.

Figure 6: Shade selection.
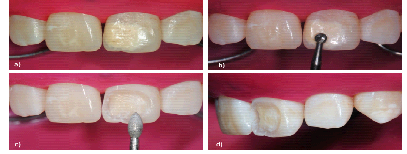
Figure 7: Cavity preparation procedure. (a) Isolation of operator field; (b) Abrasion of enamel defect on left maxillary central incisor; (c) Bevel confection; (d) Lateral view of cavity prepared.
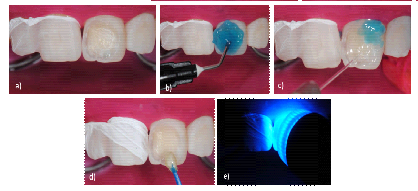
Figure 8: Pre-restorative procedure. (a) Protection of adjacent teeth; (b) Cavity etching; (c) Washing of cavity; (d) Adhesive application; (e) Light activation of adhesive.
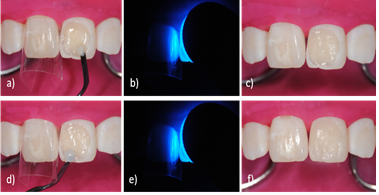
Figure 9: Restorative procedure. (a) Insertion of an opaque composite increment; (b) Light activation of a first composite increment; (c) Reestablishment of anatomical structures, such as dentin mamelons; (d) Insertion of a translucent outer composite increment; (e) Light activation of a second composite increment; (f) Reestablishment of enamel optical properties and restoration procedure finished.
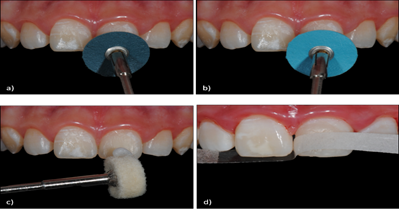
Figure 10: Finishing and polishing of composite restoration. (a) Application of medium aluminum oxide polishing disc; (b) Application of fine aluminum oxide polishing disc; (c) Application of felt discs with diamond paste; (d) Application of finishing strip.

Figure 11: Postoperative image of anterior maxillary teeth, revealing the result of the composite restoration.
3. Discussion
Molar incisor hypomineralization may be the result of different factors. As stated by Cunha Coelho and colleagues, the potential factors involved in the occurrence of MIH are uncertain [11]. In the present case report, after complete anamnesis, we concluded that the lesions of the patient emerged due to repetitive throat and ear infections accompanied by fever in early childhood. These may represent important risk factors for the development of defective lesions on surface of first molars and incisors [6, 9, 11, 12]. Other possible causes could not be determined, once the patient's legal guardian did not have much contact with the patient during her first years of life.
Although molar incisor hypomineralization lesions manifest clinically in permanent first molars and incisors, qualitative enamel defects in permanent canines, premolars and second molars cusps may also be found [11, 12]. In the clinical case here reported, enamel defects were present on buccal surface of right maxillary and mandibular first molars, left maxillary first molar, left mandibular second molar, maxillary central incisors, mandibular incisors, and to a lesser extent on canines and premolars. The spots presented clearly defined opacities, ranging from white to yellowish white, most irregularly shaped. One may note that enamel had normal thickness, except for the left maxillary central incisor, which presented a discreet pit, and the right maxillary first molar, which presented a delimited yellowish groove. In the latter case, one may infer that occlusal mechanical stresses over the fragile enamel, with lower mineral content, may have played a role to increase the substrate wear.
Enamel developmental defects, especially when located on anterior teeth, may influence the patient's social life, since they alter the smile aesthetics 13]. In case of young patients, who are entering the adolescence phase, in which social acceptance is extremely relevant, the injury may still cause behavioral and psychological changes. The present case report addressed the treatment of a patient who had depression’s onset. In such cases, aesthetic treatment should be even more relevant. Still considering the patient’s age and the enamel developmental defects presented by her, great care should be taken with cosmetic treatments. More invasive treatments should preferably be postponed. The use of ceramic laminates, for instance, is contraindicated, because of immature gingival contour of the adolescent patient. The technique requires, moreover, greater dental wear when compared to a direct restoration, which may represent a risk for pulp inflammation development [14]. Furthermore, the oral hygiene required by a ceramic laminate-based treatment, considering a possible intrasulcular cervical finishing line, should be extremely thorough and cautious. An adolescent patient is rarely responsible enough to maintain proper plaque control by daily well flossing and teeth brushing as recommended in such cases [15].
By contrast to indirect restorations, minimally invasive treatments are preferable. Among all conservative treatments of enamel developmental defects, microabrasion and bleaching are two of the most indicated ones. While microabrasion removes defects trough combined abrasion and chemical erosion [11], dental bleaching alters the tooth shade, due to the action of oxygen free radicals released by hydrogen peroxide [16] The great limitation of microabrasion, however, is that deeper defects, which reach dentin, cannot be removed with microabrasion [11, 17]
Bleaching, on the other hand, should be pondered in this particular clinical case, once the patient was 13 years old. In young patients, pulp chamber is relatively large and pulp horns may be high, close to dentin, which represents a potential risk of developing severe sensitivity [18]. Yet, depending on each specific case, radiographic examinations should be performed for a more accurate analysis of the relationships between dental structures. In the event of a positive decision on bleaching treatment in young patients, its protocol should be decided by the practitioner within an individualized careful context, as recommended by the American Academy of Pediatric Dentistry [19].
Direct restoration with composite resin is a conservative and satisfactory alternative treatment that can be performed with minimal intervention, still providing excellent mechanical, aesthetic and functional properties [13, 14]. In the present clinical case, from previous analysis of three color dimensions (hue, chroma and value) of patient's tooth, stratification technique was performed. The opaque composite restored the affected dentin, reestablishing anatomical structures, such as dentin mamelons, while a translucent composite was applied to the outer layer, replicating the enamel optical properties. Although it is known that young teeth normally present a thick, dense, slightly translucent, bright and reflective enamel [20], as well stated by Carvalho and colleagues, difference of refractive index between composite and the natural tooth may reduce the restoration value [13]. Thus, in present clinical report, during composites stratification, the enamel composite increment was thinner than the natural enamel structure. This prevented the restoration to become grayish. As a result, natural color and precise enamel and dentin thicknesses were achieved, successfully replicating the optical properties of the tooth.
As every treatment has its pros and cons, composite restoration is no exception. The major obstacle associated with the use of composite resin in enamel development lesions is its adhesion to the dental surface [11] Assunção et al explain that altered prismatic enamel morphology may interfere with material adhesion, leading to possible failures [21]. Indeed, previous studies reported lower adhesion of composite resin to hypomineralized enamel [22, 23] Other authors, however, correlated successful composite restorations to complete removal of affected enamel [13,24]. In the present case report, approximately 70% of all affected enamel were removed. Considering the age of the patient, the remaining lesion was preserved, assuming that a deeper prepare could wound the dentin, causing sensibility to pulpal tissues. Herein, it is noteworthy that practically all cavosurface margins were kept in healthy enamel (Figure 7), which possibly enhanced the adhesion.
4. Conclusion
Molar incisor hypomineralization represents an enamel developmental defect, which may directly affect smile aesthetics and therefore the self-esteem and personal relationship processes of a patient. Its treatment should be based on a concise diagnosis, and planned according to the lesion’s extent, age and history of the patient. From all of the evidence given above, it is clear that, when correctly indicated and following restorative principles, composite direct restoration may be the treatment of choice in cases of molar incisor hypomineralization.
Disclosure Statement
The authors declare no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Seow WK. Clinical diagnosis of enamel defects: pitfalls and practical guidelines. Int Dent J 47 (1997): 173-82
- Benusis KP, Pueschel SM, Hum C. Enamel hypop1asia in children with galactosemia associated with periods of poor control. ASDC J Dent Child 45 (1978): 73-75.
- Via WF Jr. Enamel defects induced by trauma during tooth formation. Oral Surg Oral Med Oral Pathol 25 (1968): 49?54.
- Kanchan T, Machado M, Rao A, Krishan K, Garg AK. Enamel hypoplasia and its role in identification of individuals: A review of literature. Indian J Dent 6 (2015): 99-102.
- Kumar GS. Enamel. In: Orban’s oral histology and embryology (1990): 66-87.
- Weerheijm KL, Jalevik B, Alaluusua S. Molar incisor hypomineralization. Caries Res 35 (2001): 390-391.
- Sapir S, Shapira J. Clinical solutions for developmental defects of enamel and dentin in children. Pediatr Dent 29 (2007): 330-336.
- Van Amerongen W, Kreulen C. Cheese molar: a pilot study of the etiology of hypocalcifications in first permanent molars. ASDC J Dent Child 62 (1995): 288-289.
- Fatturi AL, Wambier LM, Chibinski AC, Assunção LRDS, Brancher JA, et al. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent Oral Epidemiol 47 (2019): 407-415.
- Wu X, Wang J, Li YH, Yang ZY, Zhou Z. Association of molar incisor hypomineralization with premature birth or low birth weight: systematic review and meta-analysis. J Matern Fetal Neonatal Med 29 (2018): 1-9.
- da Cunha Coelho ASE, Mata PCM, Lino CA, Macho VMP, Areias CMFGP, et al. Dental hypomineralization treatment: A systematic review. J Esthet Restor Dent 31 (2019): 26-39.
- Denis M, Atlan A, Vennat E, Tirlet G, Attal JP. White defects on enamel: diagnosis and anatomopathology: two essential factors for proper treatment (part 1). Int Orthod 11 (2013): 139-65.
- Carvalho LD, Bernardon JK, Bruzi G, Andrada MA, Vieira LC. Hypoplastic enamel treatment in permanent anterior teeth of a child. Oper Dent 38 (2013): 363-368.
- Wray A, Welbury R. UK National Clinical Guidelines in Paediatric Dentistry: Treatment of intrinsic discoloration of permanent anterior teeth in children and adolescents. Int J Paediatr Dent 11 (2001): 309-315.
- Erbe C, Klees V, Ferrari-Peron P, Ccahuana-Vasquez RA, Timm H, et al. A comparative assessment of plaque removal and toothbrushing compliance between a manual and an interactive power toothbrush among adolescents: a single-center, single-blind randomized controlled trial. BMC Oral Health 18 (2018): 130.
- Silva BG, Nunes Gouveia TH, Pereira da Silva MA, Bovi Ambrosano GM, Baggio Aguiar FH, et al. Evaluation of home bleaching gel modified by different thickeners on the physical properties of enamel: An in situ study. Eur J Dent 12 (2018): 523-527.
- Pini NI, Sundfeld-Neto D, Aguiar FH, Sundfeld RH, Martins LR, et al. Enamel microabrasion: An overview of clinical and scientific considerations. World J Clin Cases 3 (2015): 34-41.
- Li Y. Safety controversies in tooth bleaching. Dent Clin North Am 55 (2011): 255-263.
- Nadim Z Baba, Shane N White, George Bogen. Policy on the Use of Dental Bleaching for Child and Adolescent Patients. Pediatr Dent 39 (2017): 90-92.
- Vanini L. Conservative composite restorations that mimic nature: a step-by-step anatomical stratification technique. Journal of Cosmetic Dentistry. Fall 26 (2010): 80-98.
- Assunção CM, Girelli V, Sarti CS, Ferreira ES, Araujo FB, et al. Molar incisor hypomineralization (MIH): case report and restorative treatment follow-up. Rev. Assoc. Paul. Cir. Dent 68 (2014).
- de Souza JF, Fragelli CB, Jeremias F, Paschoal MAB, Santos-Pinto L, e al. Eighteen-month clinical performance of composite resin restorations with two different adhesive systems for molars affected by molar incisor hypomineralization. Clin Oral Investig 21 (2017): 1725-1733.
- William V, Burrow MF, Palamara JE, Messer LB. Microshear bond strength of resin composite to teeth affected by molar hypomineralization using 2 adhesive systems. Pediatr Dent 28 (2006): 233-241.
- Sönmez H, Saat S. A clinical evaluation of deproteinization and different cavity designs on resin restoration performance in MIH-affected molars: two-year results. J Clin Pediatr Dent41 (2017): 336-342.
