Efficacy of Initiating the Right Complementary Feeding at Right Time - Bridge the Knowledge Gap Between Mother and the Caregiver in Bangladesh
Article Information
Md. Abdul Wahed1*, Md. Mashiur Rahman2, Md. Ferdous Rahman3, S.M. Quamrul Hassan4, Ahmed Ferdous5, Md. Abdus Sattar6, Murad Md. Shamsher Tabris Khan7, Gazi Mohammad Imranul Haque8
1Rangpur Mother and Child Hospital, Rangpur, Bangladesh
2Department of Pediatrics, M Abdur Rahim Medical College & Hospital, Dinajpur, Bangladesh
3Department of Pediatrics, Prime Medical College & Hospital, Rangpur, Bangladesh
4Department of Pediatrics, Shaheed M. Monsur Ali Medical College and Hospital, Sirajgonj, Bangladesh
5Department of Pediatrics, Shaheed Ziaur Rahman Medical College and Hospital, Bogura, Bangladesh
6Department Pediatric Surgery, Naogaon Medical College and Hospital, Naogaon, Bangladesh
7Deputy Program Manager, National Nutrition Services, Dhaka, Bangladesh
8Neonatal Unit, Department of Pediatrics, MH Somorita Medical College & Hospital, Dhaka, Bangladesh
*Corresponding Author: Professor Dr. Md. Abdul Wahed, Chairman, Rangpur Mother and Child Hospital, Rangpur, Bangladesh
Received: 28 August 2022; Accepted: 06 September 2022; Published: 21 November 2022
Citation: Md. Abdul Wahed, Md. Mashiur Rahman, Md. Ferdous Rahman, SM. Quamrul Hassan, Ahmed Ferdous, Md. Abdus Sattar, Murad Md. Shamsher Tabris Khan, Gazi Mohammad Imranul Haque. Efficacy of Initiating the Right Complementary Feeding at Right Time - Bridge the Knowledge Gap Between Mother and the Caregiver in Bangladesh. Journal of Food Science and Nutrition Research 5 (2022): 724-733.
Share at FacebookAbstract
Health professionals who have received nutrition training may assist to lower child undernutrition. By regularly advising caregivers on diet, qualified health professionals may specifically help achieve this goal. The risk of undernutrition among children of advised caregivers may be decreased as a result of bettering child-feeding behaviors. From six months of age forward, when breast milk alone is no longer adequate to cover all of their nutritional needs and supplemental feeding should be begun, infants and young children are at an elevated risk of malnutrition. To realize every person's full potential, appropriate nutrition throughout the first two years of life is essential. This time frame is still regarded today as being crucial for fostering healthy development, growth, and development. The health, nutritional status, growth and development of children at this period of life are thus affected by sufficient eating, not only in the short term but also in the medium and long term. For people who look after children throughout this period of life, this document offers complementary feeding (CF) guidelines that are expressed as questions or statements. Examples include when to introduce complementary feedings, when to introduce foods in order, and when to consider how the consistency of foods changes as a child's nervous system matures. Quantities for each meal; inadequate complementary feeding practices; myths and reality of complementary feeding; number of days to assess acceptability and tolerance to new foods; developmental milestones; practice of vegetarianism or baby-led weaning.
Keywords
Complementary feeding, Breastfeeding practices, Healthy infants, Guidelines
Complementary feeding articles; Breastfeeding practices articles; Healthy infants articles; Guidelines articles
Complementary feeding articles Complementary feeding Research articles Complementary feeding review articles Complementary feeding PubMed articles Complementary feeding PubMed Central articles Complementary feeding 2023 articles Complementary feeding 2024 articles Complementary feeding Scopus articles Complementary feeding impact factor journals Complementary feeding Scopus journals Complementary feeding PubMed journals Complementary feeding medical journals Complementary feeding free journals Complementary feeding best journals Complementary feeding top journals Complementary feeding free medical journals Complementary feeding famous journals Complementary feeding Google Scholar indexed journals Breastfeeding practices articles Breastfeeding practices Research articles Breastfeeding practices review articles Breastfeeding practices PubMed articles Breastfeeding practices PubMed Central articles Breastfeeding practices 2023 articles Breastfeeding practices 2024 articles Breastfeeding practices Scopus articles Breastfeeding practices impact factor journals Breastfeeding practices Scopus journals Breastfeeding practices PubMed journals Breastfeeding practices medical journals Breastfeeding practices free journals Breastfeeding practices best journals Breastfeeding practices top journals Breastfeeding practices free medical journals Breastfeeding practices famous journals Breastfeeding practices Google Scholar indexed journals Healthy infants articles Healthy infants Research articles Healthy infants review articles Healthy infants PubMed articles Healthy infants PubMed Central articles Healthy infants 2023 articles Healthy infants 2024 articles Healthy infants Scopus articles Healthy infants impact factor journals Healthy infants Scopus journals Healthy infants PubMed journals Healthy infants medical journals Healthy infants free journals Healthy infants best journals Healthy infants top journals Healthy infants free medical journals Healthy infants famous journals Healthy infants Google Scholar indexed journals baby-led weaning articles baby-led weaning Research articles baby-led weaning review articles baby-led weaning PubMed articles baby-led weaning PubMed Central articles baby-led weaning 2023 articles baby-led weaning 2024 articles baby-led weaning Scopus articles baby-led weaning impact factor journals baby-led weaning Scopus journals baby-led weaning PubMed journals baby-led weaning medical journals baby-led weaning free journals baby-led weaning best journals baby-led weaning top journals baby-led weaning free medical journals baby-led weaning famous journals baby-led weaning Google Scholar indexed journals vegetarianism articles vegetarianism Research articles vegetarianism review articles vegetarianism PubMed articles vegetarianism PubMed Central articles vegetarianism 2023 articles vegetarianism 2024 articles vegetarianism Scopus articles vegetarianism impact factor journals vegetarianism Scopus journals vegetarianism PubMed journals vegetarianism medical journals vegetarianism free journals vegetarianism best journals vegetarianism top journals vegetarianism free medical journals vegetarianism famous journals vegetarianism Google Scholar indexed journals complementary feeding articles complementary feeding Research articles complementary feeding review articles complementary feeding PubMed articles complementary feeding PubMed Central articles complementary feeding 2023 articles complementary feeding 2024 articles complementary feeding Scopus articles complementary feeding impact factor journals complementary feeding Scopus journals complementary feeding PubMed journals complementary feeding medical journals complementary feeding free journals complementary feeding best journals complementary feeding top journals complementary feeding free medical journals complementary feeding famous journals complementary feeding Google Scholar indexed journals nutritional status articles nutritional status Research articles nutritional status review articles nutritional status PubMed articles nutritional status PubMed Central articles nutritional status 2023 articles nutritional status 2024 articles nutritional status Scopus articles nutritional status impact factor journals nutritional status Scopus journals nutritional status PubMed journals nutritional status medical journals nutritional status free journals nutritional status best journals nutritional status top journals nutritional status free medical journals nutritional status famous journals nutritional status Google Scholar indexed journals child-feeding articles child-feeding Research articles child-feeding review articles child-feeding PubMed articles child-feeding PubMed Central articles child-feeding 2023 articles child-feeding 2024 articles child-feeding Scopus articles child-feeding impact factor journals child-feeding Scopus journals child-feeding PubMed journals child-feeding medical journals child-feeding free journals child-feeding best journals child-feeding top journals child-feeding free medical journals child-feeding famous journals child-feeding Google Scholar indexed journals undernutrition articles undernutrition Research articles undernutrition review articles undernutrition PubMed articles undernutrition PubMed Central articles undernutrition 2023 articles undernutrition 2024 articles undernutrition Scopus articles undernutrition impact factor journals undernutrition Scopus journals undernutrition PubMed journals undernutrition medical journals undernutrition free journals undernutrition best journals undernutrition top journals undernutrition free medical journals undernutrition famous journals undernutrition Google Scholar indexed journals
Article Details
Introduction
Under-nutrition including stunting and suboptimal breastfeeding accounts for 45% of all childhood deaths. Bangladesh has the second-highest prevalence of child under-nutrition in the world, and it is believed that 70% of the world's stunted children reside in Asia [1,2]. Complementary feeding is described by the WHO as "the process beginning when breast milk alone is no longer adequate to cover the nutritional needs of newborns, and additional meals and liquids are consequently required, in addition to breast milk" [3]. Therefore, the goal of complementary feeding is to ease the progressive shift from family-wide consumption of solid foods with nursing to between 6 and 24 months of exclusive breastfeeding. Poor CFP has been associated with a higher risk of gastrointestinal and respiratory infections as well as death [4,5]. Only 71% of Bangladeshi newborns eat the proper complementary meals by the time they are 6 to 8 months old, and once CF starts, many of them "slip off the development curve" [2,6]. As a result, it's critical that the WHO's guidelines on CF be broadly embraced [7]. The availability of enough food in the home and the use of proper nutritional expertise by caregivers are necessary for appropriate CF [8]. While BF techniques have been the subject of several research, CF has received less attention. Infants should be breastfed exclusively during the first six months of life in order to attain optimum growth, development, and health, according to the 2010 WHO Infant and Young Children Feeding (IYCF) recommendations, an internationally recognized framework implemented in Bangladesh [9]. After then, when nursing is continued for up to or beyond 2 years of age, babies should be given safe and nutritionally appropriate supplementary meals. In low- and lower-middle-income nations, under-nutrition is more common and is the cause of more than one-third of child fatalities worldwide [1]. Children's low nutritional condition in these areas has continued to be significantly influenced by poverty [3,4]. It has been named as a contributing factor to food insecurity [5,6] low maternal education [7,8] unreliable access to healthcare [7,8] and the burden of illness [8] all of which are associated with poor child nutrition status. The bad feeding habits of caregivers toward their infants may also be influenced by their socioeconomic disadvantage [9,10]. Low nutritional variety, infrequent feedings, and excessive calorie consumption are examples of poor feeding practices [11-13]. Poor eating habits may be related to social issues, such as caregivers' lack of nutrition education and their ignorance of the variety of foods available in their surroundings [17]. These elements may cause kids to eat less often, with less variety in their diets, and with less food overall. Nutrition education for caregivers may increase their general nutrition knowledge and aid to dispel cultural and traditional beliefs [18]. As a result, feeding habits may be improved if experienced healthcare professionals treat patients, advise them on good feeding techniques, and regularly monitor their development [19]. Naturally, when they are accessible, dieticians and nutritionists may provide this kind of advice [20-22]. But in many poor nations, there may not be enough health professionals with these specific abilities to provide regular care [23,24] therefore these services are instead handled by health professionals with just a broad understanding of nutrition. The research that is currently available suggests that health professionals who get nutrition training may reduce child undernourishment by modifying feeding habits. Higher levels of nutrition knowledge and counseling behavior were discovered in previous randomized controlled trials (RCTs) among health professionals who had undergone nutrition training [19,26,27]. When caregivers often sought advice from health professionals who had undergone nutrition training, their nutritional knowledge also increased [19]. Caregiver knowledge of food preparation and appropriate feeding practices were also enhanced by nutrition counseling [28,29]. Caregivers had a higher propensity to increase their kids' feeding frequency [31] dietary variety [22] protein intake [28,33] and calorie intake [23]. To improve children's nutritional status, these feeding practices must be implemented [24,15]. In the current health care systems, opportunities for regular dietary counseling may be found. In 2012, 50% of new moms visited a medical institution after giving birth, compared to 88% of pregnant women worldwide who had at least one prenatal visit [26]. These potential possibilities offer themselves for qualified healthcare professionals to provide dietary guidance. When their infants were born, just 57% of moms had a trained attendant [16]. For these women, nevertheless, there is also place for at-home nutrition counseling provided by peers or community health experts with the necessary knowledge and training.
Breastfeeding practice
Breastfeeding is a fundamental pillar of child nutrition, with important implications for the health welfare due to its impact on morbidity and mortality, especially among children under 1 year of age. Over this, the significance of breast milk as the preferred meal during the first six months of life is widely acknowledged by organizations devoted to the health of infants, and it is regarded as a vital public health policy. The World Health Organization (WHO) recommends starting breastfeeding as soon as possible after delivery and continuing it exclusively throughout the first six months of the baby's life [21]. In order to improve the nutrition of pregnant women, infants, and young children, the WHO has established the 2025 Global Nutrition Targets. In the fifth of these, "raise the percentage of exclusive breastfeeding in the first 6 months up to at least 50%," breastfeeding has been given priority.
Age, marital status, and economic level are the major sociodemographic characteristics that affect the length of breastfeeding. Therefore, younger women with poor educational levels, single women, and women with lower incomes had a decreased likelihood of successfully continuing nursing for a long time [12]. High effect elements including smoking, birth method, parity, mother-child separation, maternal education, and maternal education on breastfeeding were recently identified in one study [13]. For instance, breastfeeding rates at 6 months were much higher for women who had graduated from high school or other higher education institutions, had received breastfeeding instruction, started nursing within an hour of giving birth, and did not work outside. The breastfeeding rate during the first six months was, however, considerably lower for women who smoked and lived at home with their parents [14]. The length of breastfeeding is closely correlated with maternal age, and adolescents breastfeed less often and for a shorter period of time [15]. Adolescent women claim that the choice to breastfeed is made before to giving birth and that their partner's and family members feelings about the procedure may influence when it begins. Nursing is affected by a variety of factors, including its effects on social and personal relationships, the availability of social support, the physical difficulties of breastfeeding, understanding of breastfeeding techniques and their advantages, and the mother's comfort level with breastfeeding [16]. For moms in this age range, there is a much greater likelihood that they will continue nursing 4 weeks after giving birth if they have a better prenatal attitude to start breastfeeding and higher confidence in pre and postnatal care [17]. The behavior of nursing is complex in this manner. Each woman's choice and capacity to effectively commence breastfeeding is influenced by a variety of social, psychological, and cultural elements in addition to sociodemographic, clinical, and habitual aspects; these influences operate at several levels, from the individual to society.
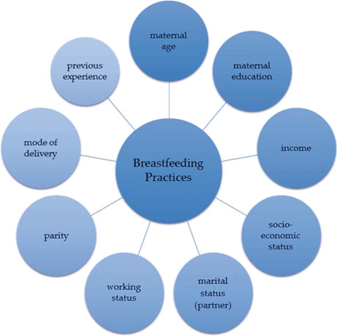
Figure 1: Breastfeeding Practices
All the variables that affect nursing practice's growth and the many levels that interact must be taken into account when creating a conceptual model of it. It is feasible to understand how several levels interact and affect a person's choice to breastfeed or not.
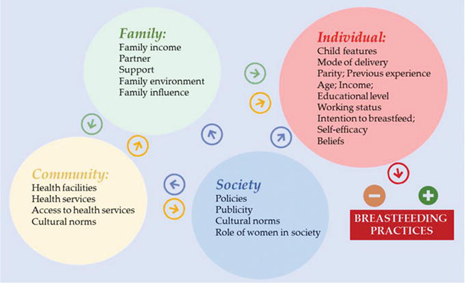
Figure 2: Breastfeeding Practices
Complementary feeding
Optimal growth and development must be maintained for the sake of babies and children's futures as well as the growth of the society in which they inhabit [14]. Children often suffer from malnutrition as a result of improper feeding practices, such as the cessation of exclusive breastfeeding and the early introduction of weaning foods. Major causes include inadequate nutritional quantity and quality later in infancy [15]. The risk of stunting and underweight in preschoolers, as well as negative effects on development and learning capacity, have all been linked in studies to household food poverty [15,16]. The higher development of children has also been connected to household food security [14]. Since development problems, micronutrient deficiencies, and infectious illnesses are most prevalent in children between the ages of 6 and 24 months, these children are often the focus of complementary/supplementary feeding therapy [7]. The preschool years (ages 1-5) are a time of rapid and profound postnatal brain growth (also known as neural plasticity), as well as the development of core cognitive skills (i.e., working memory, attention, and inhibitory control). Programs that focus on individual nutritional deficiencies may not be as long-lasting or as successful as a food-based, comprehensive approach. There are many variables that affect supplemental feeding, and moms must make difficult decisions about when and how to begin it. Prior to developing an intervention approach to avoid childhood malnutrition, it is crucial to understand the decision-making process, societal beliefs, knowledge, attitude, and complementary feeding practices. The primary proximal causes of malnutrition during the first two years of life include poor eating habits, including breastfeeding and supplemental feeding, along with high rates of infectious illnesses.
The ideal IYCF for a kid guard against both under- and over-nutrition as well as the long-term effects of both. According to a review of many studies [22,23] breastfeeding is an affordable obesity therapy. When compared to artificially-fed babies, breastfed infants had a reduced chance of developing asthma, diabetes [14] heart disease [15] high cholesterol [26] and other cardiac risk factors, as well as malignancies such childhood leukemia [19], and breast cancer later in life [20]. Given the strong correlation between food quality and obesity, effective complementary feeding with a variety of nutrient-dense meals may help avoid overweight and obesity. To ensure that investments are made in children under the age of two to reduce the risk of stunting and obesity, optimal IYCF and early intervention are even more crucial for countries that are in the midst of a nutrition transition1 and are dealing with a double burden of malnutrition (both under and over-nutrition). For newborns who have previously had poor development, a rapid catch-up in weight gain during the first two years is essential to preventing long-term under-nutrition and reducing morbidity and mortality. If a child is unable to catch up before the age of two, rapid weight gain in later childhood is not optimal since it significantly increases the risk of chronic disease. A low birth weight child who is stunted and underweight throughout childhood and adulthood before becoming overweight is the worst-case scenario for chronic diseases including cardiovascular and metabolic problems.
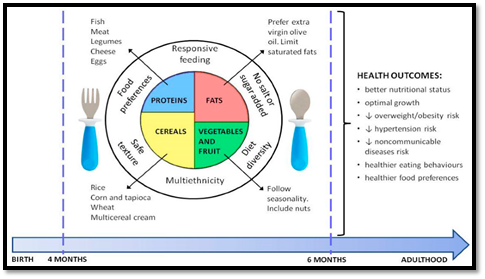
Figure 3: Health Outcomes
Beliefs regarding Complementary feeding
According to earlier studies [24], only half of the moms were aware of the ideal window of time to introduce complementary foods, which is when a baby has reached the age of 6 months. On the other hand, mothers stated that one-fourth of them believed that complementary food should be introduced before the age of six months. In Ethiopia, where it was found that 19.7% of mothers started complementary feeding before the age of six months [4]. According to the results of prior studies, more than three-quarters of the mother in the present research were aware of different supplemental meal kinds [25]. In Finland [24,26] which found that all mothers agree that complementary meals are helpful for children. The salient beliefs that mothers have regarding the benefits and drawbacks of introducing complementary feeding, as well as the importance of what others have to say, are the factors that most strongly influence mothers' decisions regarding complementary feeding. The other research was found that mothers' decisions were also strongly influenced by their neighbors, relatives, and health professionals, as well as by their perception of the benefits of complementary feeding [26]. The majority of mothers believe that complementary foods are good for their kids in a variety of ways, such as helping to develop the baby's brain and providing them with extra nourishment for healthy growth and development and improved intellect. This conclusion conflicts with one from an Australian research that revealed some mothers did not see the introduction of supplemental feeding as favorable [25]. The current research discovered that moms supplement their children's diets to cut down on the frequency of nursing and feel free to work without worrying about their child's hunger. However, almost all moms said that their infants don't like eating anything. Consistent with the research [25,26], that showed that the majority of children only drank breast milk for nutrition. Only a small percentage of women attempt to play-feed their infants, whereas over half force-feed their children. The moms may not have had a high level of education and may not have known how to feed themselves or the risks of forcing eating. A research showed that mothers' perceptions of complementary feeding are incorrect; for example, many believe that complementary foods are to blame for their kids' illnesses and avoid giving to them [12]. Nearly majority of the women consulted their families as sources of knowledge on supplemental feeding. This result is in line with the research of which discovered that dads are related to newborn and early child feeding patterns [24]. Other research, however, indicated that mothers obtained information independently from friends, family, the local community, radio, television, health institutions. The moms of the children may have all lived in slum areas and been housewives, which may be the cause. So it was challenging to walk outdoors and ask the medical professionals for information.
Period of complementary feeding
Breastmilk is the only source of nourishment for a kid up to the age of 6 months; supplemental feeding must start as soon as that milestone is reached. Additionally, the jaw starts to move in a biting motion at five months. Solid meals start to be swallowed at around 6-7 months. Between 8 and 12 months, the tongue begins to move side to side. Around six months is the optimal time, or "sensitive phase," to introduce supplemental feeding. Delaying the introduction of supplemental feeding may cause the kid to reach a "critical phase," after which the youngster may always have trouble chewing and may struggle to consume solids in the future.
The following are some additional benefits of supplementary eating at 6 months of age:
- Child improves hand-to-mouth coordination and neck/head control.
- Child begins to love biting and mouthing.
- The intestines are developed and prepared to process grains and pulses.
- Due to gum hardening and tooth emergence, the baby enjoys chewing and gumming semisolids.
- Solids are less likely to be forced out of the mouth.
|
Appropriate |
Avoidable |
|
Combination of cereals and pulses (Khichdi, Dal-rice, etc.), locally available staple foods such as idli, dosa, dhokla, ragi, chapati, roti, paratha with oil/ ghee, and some amount of sugar. |
Biscuits, breads, pastry, chocolates, cheese, softy, ice cream, doughnuts, cakes, etc. Tinned foods, packaged or stored foods, artificially cooked foods with preservatives or chemicals |
|
Mashed banana, other pulpy fruits |
Fruit juices and fruit drink |
|
Milk-based cereals preparations |
Commercial breakfast cereals |
|
Sprouts, pulses, legumes, groundnuts, almonds, cashewnuts, raisins (Note: Any nut should be well grinded and mixed with food as solid pieces maycause choking in young children) |
Repeatedly fried foods containing trans-fatty- acids (which predispose to obesity, diabetes, atherosclerosis, cardiac, and neurological problems in future) |
Table 1: Categorizes the appropriateness of complementary foods for infants
Complementary feeding practices in Bangladesh
Bangladesh confronts several difficulties in providing growing children with nutrient-appropriate nourishment. In order to prevent under-nutrition throughout the early stages of development, Bangladesh must overcome several obstacles to provide growing children with nutrition that is age-appropriate. For the first six months, a child must only be fed breast-milk in order to provide adequate nutrition and the development of a robust immune system. After this time, parents must start adding certain meals to their diets and continue nursing their children until they are two years old. The transition from only nursing to family foods is made by this approach, which is referred to as complementary feeding. It is essential for providing a kid with the extra nourishment they need and spans the key 6-24-month period for their physical and mental development Worldwide, there are greater incidences of under-nutrition among children mal five during this time due to nutrient deficits and infections. Many parents lack basic knowledge on the best times to start, how often, and the minimal requirements for dietary variety when it comes to supplementing their children's diets with food. A quarter of the population experiences food insecurity in the home. Proteins like fish and beef are sometimes out of reach for families with low budgets. Age-appropriate supplemental feeding rates throughout the country are very low, and in certain places, including urban slums, they are shockingly low. Mothers in Bangladesh often choose formula and may have a hard time persuading their husbands to buy meat and fish. There are folklores in certain societies about feeding children fish and meat. Even though these things are readily accessible at home, young children are sometimes not provided them. To ensure that babies obtain colostrum, sometimes known as "first milk," which is rich in nutrients essential for defending newborns against common diseases like pneumonia and diarrhea, breastfeeding must begin within an hour of delivery. Due to variations in geographic location and economic status, few families practice this early beginning and nursing for up to two years. As an instance, the early initiation rate in Khulna Division is 47.3% as compared to 73.5% in Sylhet. Mothers from the lowest and wealthiest quintiles breastfeed their infants less often, with 48.1 vs 62.5 percent, respectively. The World Health Assembly's goal for Bangladesh regarding exclusive breastfeeding has been met, however there has been a worrying reduction in the practice.
UNICEF collaborates with the government to educate healthcare professionals in counseling techniques and to improve their ability to communicate effectively. These community-based professionals exhibit specialized strategies for ensuring nutrition for kids, families, and caregivers. Additionally, the government educates health professionals on how to breastfeed successfully, how to conserve breastmilk, how to treat breast diseases, and how to deal with apparent milk shortages. Health professionals are also taught to evaluate and analyze the practices being used in households and utilize the results to create change-oriented initiatives. Additionally, UNICEF assists medical institutions in compiling monthly data on all district-level nutrition benchmarks. UNICEF assists the government in establishing standards for the quantity, variety, age-based frequency, texture, and cleanliness of supplemental foods for children. Boiled vegetables, animal protein, mashed cereals, and ripe fruits like papaya and mango are a few examples. As part of prenatal care, UNICEF is actively striving to increase the percentage of moms who get nutrition counseling. Along with expanding the reach of vitamin A initiative for kids between the ages of 6 months a 5 years, we are concentrating on increasing the proportion of caregivers who receive nutrition counseling overall. UNICEF promotes the rights of women and children in the workplace as part of our efforts to meet the rising needs of women and children in urban areas. As part of the Mothers Work initiative, UNICEF encourages factories to have family-friendly policies for their employees by establishing the 7 minimum standards, which include breastfeeding spaces and feeding breaks, child care availability, leave for expectant parents, financial and medical benefits, and employment protection. Breastfeeding is highly valued in Bangladesh. Over 80% of infants who are still breastfeeding at 20-23 months of age are almost all (98%) breastfed at some point in their lives. However, there are many areas of feeding infants and young children that might be far better. Less than half of newborns (43%) are breastfed within an hour of delivery, which is a common delay in breastfeeding beginning (BDHS, 2007). Due to the premature introduction of supplementary meals and other liquids, about 64% of babies less than six months are nursed exclusively (BDHS, 2011). Additionally, supplemental feeding might start too late; according to recommendations, only approximately 21% of newborns got it. The National Nutrition Services (NNS) of the Health, Population, Nutrition Sector Program (HPNSP), an initiative of the Ministry of Health and Family Welfare, aimed to educate field-level personnel in the health and family planning sectors in order to enhance IYCF practices. A three-day training course has been created.
Guideline for complementary food practices
Dietary diversity refers to providing a youngster with a variety of meals in order to sufficiently meet his or her nutritional needs. Consuming four or more of the seven food categories is known as minimum dietary diversity (MDD), which is necessary to satisfy daily nutritional and energy needs. This assures that in addition to a basic meal, the youngster has a high possibility of ingesting at least one food from an animal source and one fruit or vegetable that day (grain, root, or tuber)
|
Recommended food group |
Examples/Variety of foods in different groups |
|
Grains, roots, and tubers |
Rice, wheat, maize, jowar, ragi, potato, sweet-potato |
|
Legumes and nuts |
Pulses, nuts, oil-seeds, dry fruits |
|
Vitamin-A rich fruits and vegetables |
Orange/yellow/green vegetables or fruits such as mango, carrot, papaya, and tomato |
|
Other fruits and vegetables |
Locally available, fresh fruits and vegetables, preferably seasonal and inexpensive |
|
Dairy products |
Milk, curd, yogurt, butter, and paneer |
|
Eggs |
Eggs |
|
Flesh Foods |
Meat, fish, poultry, and organ meats |
Table 2: The various food groups for complementary food practices
For feeding newborns, a wide variety of commercial meals are offered on the market. They are pricey and often make lofty and false health promises. While readily accessible, ready-to-use food, fake food, and packaged food are often not the healthiest or most ideal options for feeding children. As much as possible, meals for children should be made at home using items that are easily accessible. Organizations dedicated to children's health adviser against promoting commercial meals for feeding newborns and young children (under 2 years old).
Quality, frequency and amount of complementary food practicing
For a kid to experience optimum growth and development, nutrition is key, particularly during the first 1,000 critical days. The emotional development of the kid depends on feeding habits that are fulfilling and comfortable for both mother and child. Regarding good feeding techniques, the mother and family should be inspired, encouraged, informed, and supported. Feeding your kid in a sensitive manner can make sure they appreciate the experience. Every society has a staple food-the item that makes up the majority of daily consumption, like wheat or rice. Parents are required to name the standard homemade cuisine. In rural areas, families might encourage growing their own food in a kitchen garden, collecting it, preparing it, and storing it whichever suits them best. Depending on their preferences and capacity to pay, urban residents may obtain the basic foods. An excellent source of protein and calories, staple foods may be prepared and served. The foods should be safe and hygienic through following steps:
- Maintain a clean atmosphere to protect food.
- It is required to provide food that seems to be fresh and smells excellent.
- Refrigerator storage is required for prepared meals and perishable items including meat, milk, and eggs.
- In the absence of a refrigerator, adequately cover the meal and give it to the kid within two hours.
- Reheat the meal before eating it to destroy any harmful bacteria if it has been kept for a longer period of time. Rats, mice, cockroaches, flies, and dust should be kept at bay while the meal is being prepared.
|
Age |
Texture |
Frequency |
Average amount of each meal |
|
6-8 months |
Begin with mashed foods or thick porridges |
Daily 2-3 meals along with frequent breastfeeding |
In the beginning, 2-3 tablespoon-full |
|
9-11 months |
Mashed foods, finely chopped, and foods that can be picked up by baby |
Daily 3 meals with continued breastfeeding plus offer 1-2 additional snacks |
1/2 cup/bowl (125 mL) |
|
1-2 years |
Staple family foods, mashed or chopped (if required |
Daily 3-4 meals with continued breastfeeding plus 1-2 additional snacks |
3/4 to one cup/bowl (250 mL) |
Table 3: The following complementary food schedule can be followed
Discussion
Children between the ages of six months and two years benefit from increased calorie intake, feeding frequency, and nutritional variety with the support and awareness provided from the health care professionals. Such a major result may be imagined along the following pathway: Nutrition education may broaden or update the understanding of food scientists and nutrition among health professionals. Indeed, two RCTs carried out in Brazil [19] and India [26] discovered that nutrition training of health professionals enhanced their nutritional understanding. Health professionals' nutrition knowledge may be updated via nutrition training, which can also inform them of new information that is relevant to their work surroundings [16,23,28,29]. They will be better able to communicate, provide counseling, and treat undernutrition as a result of being able to address the factors that contribute to undernutrition in their local communities [12,19,28,29]. Knowledgeable health professionals may impart dietary information when they provide advice to caregivers who visit medical facilities [20]. Comparable to this, skilled health professionals may contact caregivers via outreach and home visits even in remote locations, and they could achieve a similar result this way [17,24]. The caregivers who got advice from health professionals who had undergone nutrition training demonstrated increased nutrition knowledge and information retention [16,29]. The caregivers who received counseling may also act as change-makers. Parents who get regular counseling and are equipped with the most recent nutrition information are better able to feed their children [16,20]. Such habits might include eating often, combining high-quality meals well, consuming more energy, and changing one's diet. By reducing their risk of undernutrition, children's growth may be enhanced [24]. Additionally, food-borne illnesses may be decreased and food preparation cleanliness can be improved [22]. These are additional factors that contribute to undernutrition. Even in places where food is scarce, nutrition advice from qualified health professionals has been shown to be useful [21,24]. For instance, in the Bangladeshi RCT, nearly a third of the families were impoverished and had food insecurity. Despite these challenges, the nutrition information provided by skilled health professionals inspired and altered their eating habits. They may then give their kids the proper balance of meals [30]. There are some important tips for parents that they need to if they want to practice nursing complementary feeding:
- Start supplemental feedings after the 180 days have passed.
- Continue nursing for an additional two years while providing the right supplemental nutrition.
- Dispense semisolid food (Avoid watery food such as soups, fruit juices, and animal milk)
- Prefer cooking your own meal (clean, fresh, cheap, and easily available)
Prefer balanced meals (cereal, pulses, and vegetables) that are prepared using locally available products.
Add one meal at a time; as soon as the youngster begins to accept it, introduce a different preparation.
Adding ghee, oil, oil-seed powder, and fats to food increases its energy content and flavor, with the exception of children who are overweight or obese.
The child's preferences and choices must be honored. Never force feed. As much as the youngster eats, give. Observe the child's weight.
Conclusion
Health professionals who have received nutrition training may change how young infants are fed. Feeding frequency, calorie intake, and dietary variety are a few examples of these behaviors. Training materials should be created based on the local environment and should provide instructions on how to recognize meals that are readily accessible, reasonably priced, and deserving, which is crucial in places where food supply is scarce. Additionally, educated health professionals provide the possibility of a local community information source that is easily accessible and trustworthy. In this sense, educating health professionals on nutrition may be a crucial starting point for a long-term plan to raise young children's nutritional status. MNP delivery through routine health services, community-based outreach, market-based models, and other platforms has the potential to increase awareness of crucial IYCF practices in a broad sense and increase frequency of contact between caregivers and providers of IYCF counselling and support. This is because it builds on a supportive policy environment and is complemented by strategic and integrated BCC efforts. MNP treatments have the ability to provide current IYCF programs a fresh focus and new resources with frequent follow-up at the home level and the use of hands-on approaches for training caregivers on how to prepare meals and serve them to their young children. But only when MNP intervention design, implementation, monitoring, and evaluation activities are completely included into IYCF programming can this be accomplished. Initiatives focused on food that aim to achieve sustainable development have had trouble taking off. Community- and health-focused organizations have ignored these strategies in favor of programs that have yielded quick and noticeable results. Numerous underdeveloped countries, international institutions, and non-governmental organizations (NGOs) have shown that food-based approaches provide a practical, affordable, and locally enduring solution to micronutrient shortages.
References
- Black RE, Allen LH, Bhutta ZA, et al Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008, 371 (9608): 243-260.
- UNICEF: State of the World's children. New York, USA: United Nations Children's Fund (2008).
- Oldewage-Theron WH, Dicks EG, Napier CE. Poverty, household food insecurity and nutrition: coping strategies in an informal settlement in the Vaal Triangle, South Africa. Public Health 120 (2006): 795-804.
- Zezza A, Tasciotti L. Urban agriculture, poverty, and food security: empirical evidence from sample of developing countries.Rome, Italy: Food and Agriculture Organization (2010).
- Lo YT, Chang YH, Lee MS, et al. Dietary diversity and food expenditure as indicators of food security in older Taiwanese. Appetite 58 (2012): 180-187.
- Blumberg S, Bialostosky K, Hamilton W, et al. The effectiveness of a short form of the household food security scale. Am J Public Health 89 (1999): 1231-1234.
- Guldan GS, Fan HC, Ma X, et al. Culturally appropriate nutrition education improves infant feeding and growth in rural Sichuan, China. J Nutr 130 (2000): 1204-1211.
- Saloojee H, De Maayer T, Garenne M, et al. What's new? Investigating risk factors for severe childhood malnutrition in a high HIV prevalence South African setting. Scand J Public Health Suppl 69 (2007): 96-106.
- Shi L, Zhang J. Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. J Trop Pediatr 57 (2011): 91-98.
- Bhandari N, Mazumder S, Bahl R, et al. Use of multiple opportunities for improving feeding practices in under-twos within child health programmes. Health Policy Plan 20 (2005): 328-336.
- Stang J, Rehorst J, Golicic M. Parental feeding practices and risk of childhood overweight in girls: implications for dietetics practice. J Am Diet Assoc 104 (2004): 1076-1079.
- Dussault G, Franceschini MC. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health 4 (2006): 12-24.
- Meijers JM, Halfens RJ, Van der Bokhorst-de Schueren MA, et al. Malnutrition in Dutch health care: prevalence, prevention, treatment, and quality indicators. Nutrition 25 (2009): 512-519.
- Valle NJ, Santos I, Gigante DP, et al. Household trials with very small samples predict responses to nutrition counseling intervention. Food Nutr Bull. 24 (2003): 343-349.
- Aboud FE, Moore AC, Akhter S. Effectiveness of a community-based responsive feeding programme in rural Bangladesh: a cluster randomized field trial. Matern Child Nutr 4 (2008): 275-286.
- Palwala M, Sharma S, Udipi SA, et al. Nutritional quality of diets fed to young children in urban slums can be improved by intensive nutrition education. Food Nutr Bull 30 (2009): 317-326.
- Roy SK, Fuchs GJ, Mahmud Z, et al. Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately-malnourished children in Bangladesh. J Health Popul Nutr 23 (2005): 320-330.
- Vitolo MR, Rauber F, Campagnolo PD, et al. Maternal dietary counseling in the first year of life is associated with a higher healthy eating index in childhood. J Nutr 140 (2010): 2002-2007.
- Sunguya B, Koola J, Atkinson S. Infections associated with severe malnutrition among hospitalised children in East Africa. Tanzan Health Res Bull 8 (2006): 189-192.
- WHO: Building a future for women and children. The 2012 report. 2012, Geneva, Switzerland: World Health Organization (2012).
- Ahmed F. Micronutrient deficiencies among children and women in Bangladesh: progress and challenges. Journal of Nutritional Science 5 (2016): 1-12.
- Maternal multiple micronutrient supplementation has limited impact on micronutrient status of Bangladeshi infants compared with standard iron folic acid supplementation. Journal of Nutrition 140 (2010): 618.
- Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr 4 (2008): 24-85.
- Akl EA, Kennedy C, Konda K, et al. Using GRADE methodology for the development of public health guidelines for the prevention and treatment of HIV and other STIs among men who have sex with men and transgender people. BMC Publ Health 12 (2012): 386
- Assessment of study quality. Cochrane handbook for systematic reviews of interventions 426 [updated september 2006]. Edited by Higgins J, Green S. Chichester, UK: John Wiley & Sons LTD (2009): 79-87.
- Santos I, Victora CG, Martines J, et al. Nutrition counseling increases weight gain among Brazilian children. J Nutr 131 (2001): 2866-2873.
- Merrill RD. High prevalence of anemia with lack of iron deficiency among women in rural Bangladesh: a role for thalassemia and iron in groundwater. Asia Pac J Clin Nutr 21 (2012): 416-422.
- Penland JG, Sandstead HH, Alcock NW et al. A preliminary report: effects of zinc and micronutrient repletion on growth and neuropsychological function of urban Chinese children. J Am Coll Nutr 16 (1997): 268-272.
- Bangladesh National Nutrition Survey 1995-96. Institute of Nutrition and Food Science, University of Dhaka (1998).
- Bhutta ZA. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost. Lancet 382 (2013): 452-477.
