Effects of a chiropractic three-dimensional surface on vagal nerve activity and distress: An experimental study
Article Information
Hadas Tavil1*, Ariel D. Levine2, Ronen Tuchfeld3, Barak Sekeles3, Ronen Mendi4, Yori Gidron5
1The Adelson School of Medicine, Ariel University
2Orthopedic surgery department, Bnai-Zion medical center
3Daily Backup LTD
4R.L. Mendi Center Ltd
5Faculty of health sciences, University of Haifa
*Corresponding Author: Eng. Hadas Tavil, Med student, Engineer, The Adelson School of Medicine, Ariel University, Ramat Hagolan st. 56, Ariel, 4070000, Israel.
Received: 24 July 2023; Accepted: 31 July 2023; Published: 17 August 2023
Citation: Hadas Tavil, Ariel D. Levine, Ronen Tuchfeld, Barak Sekeles, Ronen Mendi, Yori Gidron. Effects of a chiropractic three-dimensional surface on vagal nerve activity and distress: An experimental study. Journal of Spine Research and Surgery. 5 (2023): 76-81.
Share at FacebookAbstract
Background:
Research in the past 30 years has shown the importance of the vagal nerve in predicting reduced risk and possible therapeutic effects on fatal diseases (e.g., heart disease, cancer) and chronic pain. Vagal nerve activity is indexed by heart-rate variability (HRV).
Objective:
This study compared the effects of a unique chiropractic 3D surface on HRV, distress, and discomfort with two control conditions.
Methods:
Thirty-six participants were recruited (mean age 51.6 years; 52.8% women), who were randomly assigned to rest for 10 minutes either in supine position on a standard mattress (control 1), rest in prone position on a standard mattress (control 2), or to rest in prone position on a chiropractic surface (experimental group). We measured HRV, blood pressure, heart rate (HR), distress, and discomfort, before, immediately after the 10min rest, and 5min later.
Results:
For participants in control 1, SDNN and PNN50 increased significantly from 1st to 3rd measures only. For participants in control 2, HRV did not change significantly. In the experimental condition, SDNN, RMSSD, and PNN50 increased significantly from 1st to 2nd measure, and SDNN increased significantly from 1st to 3rd measure. Increases in PNN50 were more prominent in the experimental group than in both controls combined.
Conclusions:
This study showed that a chiropractic surface significantly increased multiple HRV parameters, more than two control conditions. Suppose the results are reproducible in clinical situations involving the vagal nerve (e.g., diabetes); such a chiropractic surface may be a novel treatment for chronic health conditions associated with reduced HRV.
Keywords
vagal nerve; heart rate variability; chiropractic mattress; experiment; health promotion
vagal nerve articles vagal nerve Research articles vagal nerve review articles vagal nerve PubMed articles vagal nerve PubMed Central articles vagal nerve 2023 articles vagal nerve 2024 articles vagal nerve Scopus articles vagal nerve impact factor journals vagal nerve Scopus journals vagal nerve PubMed journals vagal nerve medical journals vagal nerve free journals vagal nerve best journals vagal nerve top journals vagal nerve free medical journals vagal nerve famous journals vagal nerve Google Scholar indexed journals heart rate variability articles heart rate variability Research articles heart rate variability review articles heart rate variability PubMed articles heart rate variability PubMed Central articles heart rate variability 2023 articles heart rate variability 2024 articles heart rate variability Scopus articles heart rate variability impact factor journals heart rate variability Scopus journals heart rate variability PubMed journals heart rate variability medical journals heart rate variability free journals heart rate variability best journals heart rate variability top journals heart rate variability free medical journals heart rate variability famous journals heart rate variability Google Scholar indexed journals chiropractic mattress articles chiropractic mattress Research articles chiropractic mattress review articles chiropractic mattress PubMed articles chiropractic mattress PubMed Central articles chiropractic mattress 2023 articles chiropractic mattress 2024 articles chiropractic mattress Scopus articles chiropractic mattress impact factor journals chiropractic mattress Scopus journals chiropractic mattress PubMed journals chiropractic mattress medical journals chiropractic mattress free journals chiropractic mattress best journals chiropractic mattress top journals chiropractic mattress free medical journals chiropractic mattress famous journals chiropractic mattress Google Scholar indexed journals experiment articles experiment Research articles experiment review articles experiment PubMed articles experiment PubMed Central articles experiment 2023 articles experiment 2024 articles experiment Scopus articles experiment impact factor journals experiment Scopus journals experiment PubMed journals experiment medical journals experiment free journals experiment best journals experiment top journals experiment free medical journals experiment famous journals experiment Google Scholar indexed journals health promotion articles health promotion Research articles health promotion review articles health promotion PubMed articles health promotion PubMed Central articles health promotion 2023 articles health promotion 2024 articles health promotion Scopus articles health promotion impact factor journals health promotion Scopus journals health promotion PubMed journals health promotion medical journals health promotion free journals health promotion best journals health promotion top journals health promotion free medical journals health promotion famous journals health promotion Google Scholar indexed journals Spine Pain articles Spine Pain Research articles Spine Pain review articles Spine Pain PubMed articles Spine Pain PubMed Central articles Spine Pain 2023 articles Spine Pain 2024 articles Spine Pain Scopus articles Spine Pain impact factor journals Spine Pain Scopus journals Spine Pain PubMed journals Spine Pain medical journals Spine Pain free journals Spine Pain best journals Spine Pain top journals Spine Pain free medical journals Spine Pain famous journals Spine Pain Google Scholar indexed journals Spine Research articles Spine Research Research articles Spine Research review articles Spine Research PubMed articles Spine Research PubMed Central articles Spine Research 2023 articles Spine Research 2024 articles Spine Research Scopus articles Spine Research impact factor journals Spine Research Scopus journals Spine Research PubMed journals Spine Research medical journals Spine Research free journals Spine Research best journals Spine Research top journals Spine Research free medical journals Spine Research famous journals Spine Research Google Scholar indexed journals Disc Degeneration articles Disc Degeneration Research articles Disc Degeneration review articles Disc Degeneration PubMed articles Disc Degeneration PubMed Central articles Disc Degeneration 2023 articles Disc Degeneration 2024 articles Disc Degeneration Scopus articles Disc Degeneration impact factor journals Disc Degeneration Scopus journals Disc Degeneration PubMed journals Disc Degeneration medical journals Disc Degeneration free journals Disc Degeneration best journals Disc Degeneration top journals Disc Degeneration free medical journals Disc Degeneration famous journals Disc Degeneration Google Scholar indexed journals Spine tumor articles Spine tumor Research articles Spine tumor review articles Spine tumor PubMed articles Spine tumor PubMed Central articles Spine tumor 2023 articles Spine tumor 2024 articles Spine tumor Scopus articles Spine tumor impact factor journals Spine tumor Scopus journals Spine tumor PubMed journals Spine tumor medical journals Spine tumor free journals Spine tumor best journals Spine tumor top journals Spine tumor free medical journals Spine tumor famous journals Spine tumor Google Scholar indexed journals Spinal cord articles Spinal cord Research articles Spinal cord review articles Spinal cord PubMed articles Spinal cord PubMed Central articles Spinal cord 2023 articles Spinal cord 2024 articles Spinal cord Scopus articles Spinal cord impact factor journals Spinal cord Scopus journals Spinal cord PubMed journals Spinal cord medical journals Spinal cord free journals Spinal cord best journals Spinal cord top journals Spinal cord free medical journals Spinal cord famous journals Spinal cord Google Scholar indexed journals
Article Details
Introduction
Among the leading non-communicable diseases which form the global burden of diseases (GBD) are ischemic heart disease (IHD), stroke, cancer, and chronic obstructive pulmonary disease (COPD) [1]. Moreover, mental illnesses and chronic pain are burdens that contribute to disability-associated life years (DALY) [2]. Inflammation and an excessive sympathetic response are either etiologic or prognostic factors for GBDs [3]. For example, in cancer, the inflammatory response interferes with cellular anti-cancer processes (e.g., p53) and contributes to escape from apoptosis, angiogenesis, and metastasis [4]. The sympathetic response determines the destination of metastasis and increases the metastatic potential [5]. Inflammation and the sympathetic response may also contribute to developing mental diseases [6].
Both inflammation and sympathetic activity are related to low vagal activity. Insufficient vagal activity can predict the diseases mentioned above [3]. Research has shown the importance of the vagal nerve in predicting reduced risk and possibly having therapeutic effects on GBDs and mental conditions [3,7,8]. We index the vagal nerve’s activity by heart-rate variability (HRV) [9], the fluctuations in the intervals between normal heartbeats. High HRV predicts a lower risk of and better prognosis following heart attacks [10] and better survival rates in cancer [7]. These relations may exist because the vagal nerve inhibits inflammation, oxidative stress, and sympathetic activity, contributing to GBDs [3,11]. HRV is also negatively related to mental conditions [12] and to known risk factors such as obesity, diabetes, and hypertension [13].
These findings call for activating the vagal nerve in people at risk for GBDs, mental diseases, and their risk factors. One inexpensive manner to activate the vagal nerve is by deep and paced slow breathing, which increases HRV [8]. However, not all people can perform such deep breathing, especially those with pulmonary problems. Additionally, this requires long-term adherence to 15-20 min of daily practice. Another option includes vagomimetic medications (e.g., pyridostigmine). However, such drugs may have side effects.
Additionally, electrically stimulating the vagal nerve stimulation is possible via an implantable device or non-invasive device placed on the ear or neck [14]. These methods also have side effects, such as pain. Thus, the development of other passive solutions for vagal activation is needed. Can resting on unique surfaces improve HRV?
One study found that resting on firm mattresses led to more significant increases in HRV [15]. Based on chiropractic principles, a new 3D surface for self-care was developed (CogniSpine). It aims to achieve a sensory-motor integration of signals from the limbs and spine with cortical activity [16]. We accomplished this by using natural spinal decompression and adjustments without external force. This surface also aims to increase diaphragmatic breathing, which may elevate HRV. Studies have shown that chiropractic spinal adjustment of C1-2 increases HRV [17]. Yet, the effects of this 3D surface on HRV have not been investigated. This study aimed to examine the impact of the 3D surface on HRV and perceived stress levels using an experimental randomized-controlled trial (RCT) design. Since the 3D surface requires laying in the prone position and resting in the horizontal position increases HRV [18], this position may partly account for the effects of the 3D surface protocol. Thus, we compared three groups:
Resting in a supine position on a standard mattress (control 1)
Resting in the prone position on a standard mattress (control 2)
Resting in the prone position on the CogniSpine 3D surface (experimental condition)
Methods
Sample:
After obtaining ethics approval from the ethics committee of the faculty of health sciences at Haifa University, we recruited 36 generally healthy participants from the north of Israel who volunteered to participate in this study. For health reasons during the Covid-19 pandemic, only asymptomatic people or those vaccinated against Covid-19 were allowed to participate. Nevertheless, two participants didn’t have proof of vaccination but were otherwise healthy.
Measures:
Background information:
This included participants’ age, gender, weight, height, hours of physical activity/week, smoking, co-morbidities (hypertension, diabetes, chronic pain), and when they received vaccination for the 2nd or 3rd time against Covid-19.
Vagal nerve activity and blood pressure:
HRV parameters were obtained using the “IFeelWell” HRV monitor device, which provides HRV time domain parameters of the standard deviation of intervals between normal beats (SDNN), root mean square of successive differences (RMSSD), and the percent of normal intervals > 50 ms (pNN50). HRV was measured before, during, and 5 min after resting on the CogniSpine 3D surface or on a standard mattress, each time segment lasting 5 minutes. This device uses a photoplethysmograph placed on the left index finger during the measurements. A recent study found that HRV measured by the “IFeelWell” device predicted IBD exacerbations in children [19]. Blood pressure was measured using a digital blood pressure monitor (“Matrix 100”).
Discomfort and stress:
Discomfort was assessed by asking participants to indicate their level of discomfort on a 1-100 scale (1 = no discomfort, 100 = worse discomfort). Similarly, we asked participants to indicate their current stress level on a 1-100 scale (1 = no stress, 100 = highest stress). Both parameters were assessed at baseline (T1), after resting in one of the positions (T2), and 5 min later (T3).
Design:
This study employed an experimental design. Using random numbers generated by an online program, participants were randomly assigned to either:
- The experimental CogniSpine 3D surface and resting in the prone position
- Resting in a supine position on a standard mattress (control 1)
- Resting in the prone position on a standard mattress (control 2)
Their levels of HRV, discomfort, and stress were assessed 5 min before (T1=Baseline), during the 10 min resting on their allocated surface (T2=Post-treatment), and after an additional 5 min (T3=Recovery). The measures during T1 and T3 were obtained while participants were sitting.
Interventions:
The experimental CogniSpine 3D surface is a specially designed and patented geometric shape and a combination of visco-elastic materials of different firmness levels. The surface dimensions were: 95cm X 20cm X 50cm. There are no reported long-term adverse effects from using the CogniSpine 3D surface among patients who used it.
The first control group rested on a standard mattress in the prone position. The mattress dimensions were 190cm X 140cm X 20cm. The second control group used the same standard mattress but rested supine. Participants of all three groups were instructed to rest on the mattress for 10min.
Precautions taken for the Covid-19 pandemic:
To ensure participants’ hygiene during the Covid-19 pandemic, we used the “CleanBit” device between participants. According to the FDA and the Israeli authorities, this produces an anti-septic spray that destroys 99.99% of pathogens and is safe and acceptable.
Statistical analysis:
After randomization, we first tested the equality of groups on baseline data, using an analysis of variance (ANOVA) for continuous data and chi-square tests for categorical data. Then, all outcomes were examined using a mixed-design ANOVA, focusing on the Time x Group interaction, with Time (T1, T2, T3) serving as the within-subjects factor and group (experimental, control 1 and control 2 merged) serving as the between-subjects factor. Changes from T1 to T2 and T1 to T3 were also tested within each group separately using paired t-tests. All the data is presented in its original values. Yet, since many HRV parameters were not normally distributed, we log-transformed them. We thus performed the primary analyses on the log-transformed values.
Results
Demographic variables
In control group 1, percentages of males and females were similar, while in control group 2, 2/3 were men, and in the experimental group, 2/3 were women. Across the groups, 18-50% of all participants smoked, and 9-29% had chronic pain. The mean age of all participants ranged from 48-54 years in the three groups. Tables 1 and 2 show the demographic data in each group.
|
Group Variable |
Control 1 |
Control 2 |
Experimental |
|||
|
Gender |
M |
F |
M |
F |
M |
F |
|
45.5 |
54.5 |
63.6 |
36.4 |
35.7 |
64.3 |
|
|
Smoking |
27.3 |
18.2 |
50 |
|||
|
Hypertension |
0 |
0 |
14.3 |
|||
|
Diabetes |
0 |
0 |
0 |
|||
|
Chronic Pain |
9.1 |
9.1 |
28.6 |
|||
Table I: Percentages of cases per group on demographic and health variables
|
Group Variable |
Control 1 |
Control 2 |
Experimental |
|||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Age [y] |
51.64 |
12.05 |
48 |
14.41 |
54.36 |
11.51 |
|
BMI [kg/m2] |
23.55 |
3.58 |
25.38 |
3.76 |
24.9 |
2.34 |
|
Sports [h/w] |
3.91 |
3.42 |
4.54 |
5.37 |
6.32 |
4.32 |
Table II: Means and standard deviations per group of continuous demographic and health variables
Changes in study outcomes over time per group
The three groups showed no significant differences in all the demographic variables, indicating that the randomization procedure was adequate.
|
Group Variable |
Control 1 |
Control 2 |
Experimental |
|||
|
Stress |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
14.09 |
17.72 |
26.64a*b* |
30.01 |
13.57 |
18.55 |
|
2 |
12.73 |
17.8 |
20.27 |
28.62 |
11.93 |
14.95 |
|
3 |
10 |
17.18 |
17.27 |
26.02 |
12.64 |
17.35 |
|
Discomfort |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
8.36 |
15.28 |
11.82 |
14.71 |
16.43 |
20.14 |
|
2 |
9.45 |
14.23 |
11.36 |
10.27 |
18.57 |
25.9 |
|
3 |
7.64 |
10.8 |
7.27 |
7.54 |
11.79 |
15.39 |
|
RMSSD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
29.57 |
17.96 |
32.41 |
10.01 |
27.48b* |
13.29 |
|
2 |
27.46 |
16.14 |
31.7 |
20.25 |
31.19 |
14.7 |
|
3 |
31.72 |
17.97 |
34.05 |
15.18 |
35.46 |
20.49 |
|
SDNN |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
33.99b* |
11.09 |
45.52 |
15.48 |
37.34a*b* |
16.55 |
|
2 |
41.9 |
20.85 |
44.93 |
25 |
41.99 |
17 |
|
3 |
40.13 |
11.84 |
50.13 |
22.24 |
43.42 |
17.66 |
|
PNN50 |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
8.57b* |
17.43 |
11.56 |
11.56 |
7.98a** |
10.4 |
|
2 |
6.96 |
11.97 |
8.03 |
9.63 |
12.18 |
13.09 |
|
3 |
11.21 |
17.26 |
10.93 |
11.66 |
8.15 |
8.35 |
|
SBP [mmhg] |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
115.55 |
13.65 |
119.95 |
17.27 |
112.93 |
13.49 |
|
3 |
120.05 |
16.72 |
118.09 |
17.90 |
112.75 |
12.47 |
|
DBP [mmhg] |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
67.86b* |
10.64 |
70.32 |
10.38 |
64.32 |
8.28 |
|
3 |
71.45 |
11.45 |
68.27 |
10.89 |
66.86 |
7.55 |
|
HR [bpm] |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
1 |
69.14b*** |
6.61 |
71.18 |
12.50 |
69.64 |
9.29 |
|
3 |
64.68 |
6.05 |
71.00 |
12.84 |
68.68 |
9.93 |
Note: Control 1= Standard mattress with supine rest; Control 2= Standard mattress with prone rest; Experimental= CogniSpine 3D surface; a= Difference between baseline and post-treatment; b= Difference between baseline and recovery period; *=p≤0.05; **=p≤0.01; ***p≤0.001; 1=Baseline; 2=Post-treatment; 3=Recovery
Table III. Means and standard deviations of main study outcomes per group
Table 3 shows the results of the main study variables in each group. For control group 1, SDNN significantly increased from T1 to T3 (t(10)=2.58, p<0.05). Similarly, PNN50 significantly increased from T1 to T3 (t(8)=3.04, p<0.05). Mean DBP significantly increased from T1 to T3 (t(10)=2.70, p<0.05) and Mean HR significantly decreased from T1 to T3 (t(10)=4.56, p=0.001).
For control group 2, stress levels significantly decreased from T1 to T2 (t(10)=2.71, p<0.05) and from T1 to T3 (t(10)=2.57, p<0.05). No other cardiovascular parameter changed over time.
For the experimental group, RMSSD significantly increased from T1 to T3 (t(13)=2.89, p<0.05). SDNN significantly increased from T1 to T2 (t(13)=2.15, p=0.05) and from T1 to T3 (t(13)=2.17, p<0.05). Finally, PNN50 significantly increased from T1 to T2 (t(11)=3.32, p<0.01). All other contrasts were not statistically significant. Figure 1 shows the changes in RMSSD over time per group. Finally, we found no correlations between the baseline subjective parameters of distress and discomfort and any HRV parameter (all p’s> 0.05).
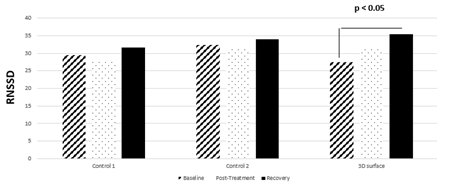
Figure 1: Changes in root mean square of successive differences (RMSSD) overtime per group
Further analyses showed no significant differences in any measure of HRV at all three-time points (T1, T2, T3) between control 1 and control 2 (all p’s> 0.05). We thus merged both control groups and compared them to the experimental group. For RMSSD, the time X group interaction tended to be significant (F(2,68)=2.52, p<0.09). Subsequently, RMSSD changed significantly in the experimental group (F(2,68)=3.35, p=0.05), but not in the merged control groups (F(2,42)=2.25, p=0.11). Specifically, RMSSD didn’t change between T1 to T2 (p>0.05) or between T1 to T3 (p>0.05) in the merged control groups. In contrast, RMSSD tended to increase significantly between T1 to T2 (p=0.09) and significantly increased between T1 to T3 (p<0.05) only in the experimental group. For pNN50, the time X group interaction was significant (F(2,58)=6.73, p<0.005). Following this, we found that pNN50 didn’t change over time in the merged control groups (p>0.05) but did increase from T1 to T2 in the experimental group (p=0.007). Yet, the time X group interaction was insignificant for SDNN (F(2,68)=0.31, NS).
Discussion
Some chronic non-communicable diseases and mental illnesses are associated with low vagal activity, indexed by low HRV [3,7,12]. Finding new ways to stimulate the vagal nerve can help reduce the individual, social, medical, and economic burden of such diseases. In the present study, we examined the effects of an innovative chiropractic 3D surface on vagal nerve activity and distress. Participants were randomly allocated to rest in the supine position on a standard mattress (control 1), to rest in the prone position on a standard mattress (control 2), or to rest on a 3D surface in the prone position (experimental).
For control group 1, two HRV time domain parameters (SDNN, pNN50) significantly increased from baseline to recovery. Mean DBP significantly increased from baseline to recovery, while mean HR decreased simultaneously. For control group 2, only stress levels decreased from baseline to post-treatment and from baseline to recovery. All three HRV time domain parameters (RMSSD, SDNN, pNN50) increased for the experimental group. Specifically, increases from baseline to post-treatment were seen in both SDNN and pNN50. Finally, both RMSSD and SDNN increased from baseline to recovery.
A similar pattern emerged when comparing the merged control groups to the experimental group. RMSSD and pNN50 increased in the experimental group and didn’t change in the integrated control groups. Combining the two control groups provided greater statistical power. The last results strengthen the pattern observed when analyzing all three groups separately.
These results show that control group 1 had inconsistent effects on cardiovascular outcomes, which were not seen in the post-treatment period, but did show during recovery. Control group 2 participants only seemed to improve in subjective distress. In contrast, resting on the chiropractic 3D surface led to more significant increases in HRV in both periods and more consistently than resting on a standard mattress in either position. These results echo those of Kou et al. 2013 who found that resting on a firm mattress led to increased HRV compared to a soft mattress [15]. Our results replicated and extended their results by showing increases in time domain HRV parameters using an innovative firm mattress designed to mimic chiropractic manipulations. This innovative 3D surface (CogniSpine) is thought to simultaneously activate body organs and systems, based on chiropractic principles, to improve the integration of signals from the limbs and spine with cortical activity [16]. These mechanisms await further investigation.
We found no correlations between the baseline subjective indexes of stress and discomfort with HRV. However, this contrasts with a meta-analysis that found that HRV decreases after an acute stressor [20]. We did not induce stressors in the present study, which could explain the lack of correlations.
This study included several limitations. First, regarding the study’s design, we didn’t have another control group that rested supine on the 3D surface since it is technically impossible due to its planned structure for such use. Nevertheless, we compared resting on the 3D surface in a prone position to two planned control conditions where participants rested in supine or prone positions on a standard mattress. Second, the sample size was relatively small, which could have masked certain effects. Third, we did not measure any frequency domain HRV parameter. Future studies should address these limitations by increasing the sample size and measuring the time and frequency domains of HRV.
If replicated, the results of this study may have clinical implications related to the ability to increase HRV by resting on the CogniSpine 3D surface. Prospective randomized controlled studies on populations with chronic physical diseases or mental illnesses associated with low HRV using this 3D surface, need to be performed. These could include a more extended period of using the 3D surface and long-term measures, which may reveal enduring effects on HRV and clinical outcomes.
Acknowledgements
The authors wish to thank the participants of the study.
Grant support or other sources of funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval and consent to participate
The study was approved by the ethics committee of the faculty of social welfare and health sciences, University of Haifa, and participants provided written informed consent. Trial registration number: 2786.
Declarations of conflicting interests
Ronen Tuchfeld, Barak Sekeles and Dr. Ronen Mendi declare conflicting interests. R. Tuchfeld owns the company of the experimental 3D surface. B. Sekeles and Dr. R. Mendi are consultants in the company. However, the experiment was conducted independently by Hadas Tavil and the statistical analyses were performed independently by Yori Gidron and Hadas Tavil.
References
- Vos T, Lim SS, Abbafati C, et al. GBD 2019 Diseases and Injuries Collaborators: Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 (2020): 1204-1222.
- Hay SI, Abajobir AA, Abate KH, et al. GBD 2016 DALYs and HALE Collaborators: Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390 (2017): 1260-1344.
- Gidron Y, Deschepper R, De Couck M, et al. The Vagus Nerve Can Predict and Possibly Modulate Non-Communicable Chronic Diseases: Introducing a Neuroimmunological Paradigm to Public Health. J Clin Med 7 (2018): 371.
- Greten FR and Grivennikov SI. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 51 (2019): 27-41.
- Stavropoulos I, Sarantopoulos A and Liverezas A. Does sympathetic nervous system modulate tumor progression? A narrative review of the literature. J Drug Assess 9 (2020): 106-116.
- Martone G. The inflammation hypothesis and mental illness. J Clin Psychiatr Neurosci 2 (2019): 3-12.
- Zhou X, Ma Z, Zhang L, et al. Heart rate variability in the prediction of survival in patients with cancer: A systematic review and meta-analysis. J Psychosom 89 (2016): 20-25.
- Gitler A, Vanacker L, De Couck M, et al. Neuromodulation Applied to Diseases: The Case of HRV Biofeedback. J Clin Med 11 (2022): 5927.
- Kuo TB, Lai CJ, Huang YT et al. Regression analysis between heart rate variability and baroreflex-related vagus nerve activity in rats. J Cardiovasc Electrophysiol 16 (2005): 864-869.
- Buccelletti E, Gilardi E, Scaini E, et al. Heart rate variability and myocardial infarction: Systematic literature review and metanalysis. Eur Rev Med Pharmacol Sci 13 (2009): 299-307.
- Rosas-Ballina M, Olofsson PS, Ochani M, et al. Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science 334 (2011): 98-101.
- Koch C, Wilhelm M, Salzmann S, Rief W and Euteneuer F. A meta-analysis of heart rate variability in major depression. Psychol Med 49 (2019): 1948-1957.
- Benichou T, Pereira B, Mermillod M, et al. Heart rate variability in type 2 diabetes mellitus: A systematic review and meta-analysis. PLoS One 13 (2018): e0195166.
- Li L, Wang D, Pan H, et al. Non-invasive Vagus Nerve Stimulation in Cerebral Stroke: Current Status and Future Perspectives. Front Neurosci 16 (2022): 820665.
- Kuo TBJ, Li J-Y, Lai C-T, et al. The Effect of Bedding System Selected by Manual Muscle Testing on Sleep-Related Cardiovascular Functions. BioMed Res Int (2013): 937986.
- Haavik-Taylor H and Murphy B. Cervical spine manipulation alters sensorimotor integration: A somatosensory evoked potential study. Clin Neurophysiol 118 (2007): 391-402.
- Win NN, Jorgensen AM, Chen YS et al. Effects of Upper and Lower Cervical Spinal Manipulative Therapy on Blood Pressure and Heart Rate Variability in Volunteers and Patients with Neck Pain: A Randomized Controlled, Cross-Over, Preliminary Study. J Chiropr Med 14 (2015): 1-9.
- Watanabe N, Reece J and Polus BI. Effects of body position on autonomic regulation of cardiovascular function in young, healthy adults. Chiropr Osteopat 15 (2007): 19.
- Yerushalmy-Feler A, Cohen S, Lubetzky R, et al. Heart rate variability as a predictor of disease exacerbation in pediatric inflammatory bowel disease. J Psychosom Res 158 (2022): 110911.
- Kim H-G, Cheon E-J, Bai D-S, et al. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig 15 (2018): 235-245.
