Effect of mHealth on modifying behavioural risk-factors of hypertensive Disorders in Pregnancy in Mezam Division.
Article Information
Nkem Ernest NJUKANG.1,5,6* Thomas Obinchemti EGBE.2 Nicolas TENDONGFOR.8 Tah Aldof YOAH.1,10,11 Kah Emmanuel NJI.1,9 Martyn SAMA.1 Fidelis Atabon AKO.7 Joseph KAMGNO.3,4
1Department of Public Health and Hygiene.
2Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Buea, Cameroon.
3Faculty of Medicine and Biomedical Sciences/University of YaoundeI.
4Centre for Research on Filariasis and other Tropical Diseases (CRFilMT), Yaounde, Cameroon.
5Quality Assurance/Quality Management System Mentor, Global Health System Solutions (GHSS), Yaounde,Cameroon.
6Country Project Coordinator, Africa Field Epidemiology Network, Far North Region, Cameroon.
7Service Head, Blood Transfusion Centre, Regional Hospital Bamenda.
8Head of Department Public Health and Hygiene, University of Buea.
9African Capacity Building Foundation Harare, Zimbabwe.
10Department of School Health Promotion, Regional Delegation of Secondary education.
11Department of Public Health and Epidemiology, Biaka University Institute of Buea.
*Corresponding Author: Nkem Ernest Njukang, Faculty of Health Sciences, University of Buea, Cameroon.
Received: 13 November 2022; Accepted: 19 November 2022; Published: 2 December 2022.
Citation: Nkem Ernest NJUKANG., Thomas Obinchemti EGBE., Nicolas TENDONGFOR., Tah Aldof YOAH., Kah Emmanuel NJI., Martyn SAMA., Fidelis Atabon AKO., Joseph KAMGNO. Effect of mHealth on modifying behavioural riskfactors of hypertensive Disorders in Pregnancy in Mezam Division. Journal of Environmental Science and Public Health. 6 (2022): 314-321.
Share at FacebookAbstract
Background: The increasing trend of non-communicable diseases (NCDs) has placed heavy burden” in low and middle-income (LAMI) countries. Hypertensive disorders in pregnancy (HDP) been one of the NCD remain a major public health problem worldwide, and its prevalence varies from country to country and from institution to institutions. HDP remain a major cause of maternal and neonatal morbidity and mortality. Mobile phone technology is increasingly viewed as a promising communication channel that can be utilized for primary prevention of NCDs by promoting behaviour change and risk factor modification. The aim of this study was to evaluate the effect of mHealth intervention in bringing about changes in behavioural risk factors of HDP in Mezam division.
Methods: It is a “Before and After” Intervention study conducted on over 342 subjects, over a period of seven months ( April - October, 2018) in Mezam division, NWR Cameroon. An mHealth intervention package consisting of weekly text messages and monthly telephone calls addressing lifestyle modification for risk factors of HDP was given to the intervention group , compared to no intervention package in control group . Consecutive sampling was used to recruit participants into the study. Eligibility to partake in the study was the possession of a cellphone.
Results: At baseline, the two groups were similar in terms of socio -demographic characteristics and modifiable behavioural risk factors . At the end of the Intervention Phase , significant improvement was seen in modifiable behavioural risk factors in the intervention group compared to control group. Mean alcohol consumption score decreased from 20.7 to 1.4; P<0.001. Stress decreased from an average of 54.4 to 19.3; P=0.002. High salt intake decreased from an average of 16.4 to 4.3; P=<0.001. Physical activity (MET/min/week) increased from 183.00 to 417.27; P=<0.001. Fru
Keywords
Behavioural risk factors, mobile communication, health promotion, HDP.
Behavioural risk factors articles; mobile communication articles; health promotion articles; HDP articles.
Article Details
1. Introduction
Hypertensive disorders in pregnancy (HDP) remain a major public health problem worldwide, and its prevalence varies from country to country and from institution to institutions. HDP remain a major cause of maternal and neonatal morbidity and mortality(1, 2) . The prevalence of HDP is roughly 8–10% of all pregnancies worldwide (3-5). It complicates up to 1 in 10 gestations and affects an estimated 240,000 women in the United States each year (6). In Asia and Africa, nearly one tenth of all maternal deaths are linked to HDP, likewise in Latin America where a quarter of all maternal deaths have been linked to these complications (7).
A number of modifiable/behavioural risk factors are linked with increased risk to this condition. These are tobacco use, physical inactivity, unhealthy diet, excessive salt intake, stress and harmful use of alcohol. These risk factors are now common not only in developed countries but in less developed countries as well. Primary prevention of HDP is directed towards modifying these risk factors.
Smoking, alcohol intake, poor physical activity and insufficient fruit and vegetable intake are well-known modifiable/behavioral risk factors of HDP (8, 9). Addressing this risk factors is important not just for reducing adverse pregnancy outcomes such as low birth weight, fetal and infant mortalities, and potential congenital defects, but for decrease of HDP among mothers as well (8, 9). In Nepal, a 2013 non-communicable disease risk factor survey (STEPS) revealed national prevalence of tobacco use to be 30.8%, alcohol intake of 17.4%, insufficient fruit and vegetable intake of 98.9%, and poor physical activity of 3.5% (10). In addition, a higher percentage (15%) of pregnant women reported to consume alcohol during pregnancy (11).
Behaviour change communication (BCC) is an important strategy for modification of behavioural or lifestyle associated risk factors of HTN. Text messages using mobile phones is viewed as a promising communication channel that offers the potential to improve healthcare delivery and promote behaviour change among vulnerable populations. The most important advantage of text messages (mobile health intervention) is the fact that it can be delivered to several individuals in a cost-effective way and in a fairly shorter time.
There are limited studies demonstrating the effect of mHealth in lifestyle modifications for HDP, especially in less developed countries and evidence for effectiveness of these interventions comes from reviews which have not included such countries (12, 13). Nevertheless, a systematic review conducted to investigate the effectiveness of mHealth interventions to promote physical activity and healthy diets reviewed 15 studies conducted in low and medium income (LAMI) countries across the world, resolved that the majority of the studies established that mHealth interventions were effective in promoting physical activity and healthy diets (14). The current study was conducted with the objective of evaluating the effect of mHealth intervention in bringing about changes in behavioural risk factors of HDP in a Mezam division.
Behaviour change communication (BCC) is an important strategy for modification of behavioural or lifestyle associated risk factors of NCDs. Mobile phone technology is viewed as a promising communication channel that offers the potential to improve healthcare delivery and promote behaviour change among vulnerable populations. A major advantage of mHealth interventions is the fact that they can be delivered to many individuals in a cost-effective manner and in a relatively shorter time.
There are limited studies demonstrating the effect of mHealth in lifestyle modifications for NCDs, especially in less developed countries and evidence for effectiveness of these interventions comes from reviews which have not included such countries (12, 15). Nevertheless, a systematic review conducted to investigate the effectiveness of mHealth interventions to promote physical activity and healthy diets reviewed 15 studies conducted in low and medium income (LAMI) countries across the world, resolved that the majority of the studies established that mHealth interventions were effective in promoting physical activity and healthy diets (16). The current study was conducted with the objective of evaluating the effect of mHealth intervention in bringing about changes in behavioural risk factors of HDP in Mezam division.
2. Methods
2.1 Study design and area: We conducted a hospital-based, “before and after” intervention study with control over a period of seven months from April to October, 2018. The study was conducted in the Santa and Tubah health district (HD) within Mezam Division. Four facilities, two from each district were selected for the study. For Santa HD; Santa District Hospital and Akum Integrated Health Centre (IHC). For Tubah HD; Tubah District Hospital and Bambui IHC. Both districts have almost equal level of development (Rural Areas). The population though cosmopolitan has a greater majority of local ethnic groups, practice subsistence farming and can boast of a rich variety of food crops. The town is endowed with touristic potentials owing to its landscape characterized by waterfalls, craters and traditional palaces. Subsistent farming and petit trading characterise women of this sub-divisions, keeping some of the women very active. However, the current crisis in the region has limited these women from their activities and equally contributed to little/no ANC follow-up, as a result putting pregnant women at risk of developing HDP.
Approval of the study was obtained from the Faculty of Health Science Institutional Review Board, University of Buea and the Regional Delegates of Public Health, NWR and Directors of all facilities involved in the study.
2.2 Participants
We recruited the participants using a consecutive sampling method (pregnant women ≤13 weeks and meeting the inclusion criteria were included in the study). We included pregnant women of reproductive ages, who had been residing in Mezam division for at least 6 months, had access to mobile phones and could read the messages. Individuals with impaired sight, hearing, inability to talk and those with severe mental retardation were excluded from the study. We equally excluded pregnant women who could not be contacted after 3 successive calls. Participants were enrolled in the study after obtaining written and informed consent.
2.3 Sample size, allocation and blinding
With the assumption of a 18.1% prevalence of alcohol consumption in Ngoundere (Adamawa Region, Cameroon) at 95% confidence with 80% power, 142 participants per group were needed for a 10%, reduction in risk factors to be detected (17). Assuming an attrition rate (loss to follow-up) of 20%, 171 participants were needed for each group. The participants were allocated to intervention and control groups in the ratio of 1:1. The two sub-divisions are further from one another and the health facilities widely spaced out within each district. This was done to avoid interaction and communication between participants in the two groups. Though it was not possible to blind the investigator, the participants were blinded as they do not know which group they were allocated to (single blind study).
2.4 Procedure
The study went on in three phases i.e. the Pre-Intervention, Intervention and Post-Intervention Phases. In the Pre-Intervention Phase, baseline data was collected from both groups using a pre-tested, structured questionnaire based on the WHO STEPS approach for NCD risk factor surveillance. We collected personal and socio-demographic data and detailed information about behavioural risk factors of hypertension in pregnancy (physical inactivity, tobacco, poor diet, high salt intake, stress and alcohol use). Hight, weight and blood pressure were measured. Participants knowledge of HTN was equally evaluated. In the Intervention phase, the intervention package for the intervention group included weekly text messages delivered through SMS. The messages included short and catchy slogans on the importance of modification of behavioural risk factors. Each message had an average of 20–30 words. The schedule of the messages was prepared to address each behavioural risk factor and messages were sent every week in rotation. At a time, two risk factors were addressed. The subjects in the intervention group were equally contacted via telephone calls once a month. Each telephone call lasted for about 20 minutes during which we reiterated the importance of modifying behavioural risk factors of HDP, addressed queries and provided positive reinforcement. No such mHealth intervention package was given to the control group. In the Post-Intervention Phase, participants were visited at their last ANC (last ANC dates were recorded and participants contacted on phone before this dates) and data regarding their personal, socio-demographic, behavioural risk factors, weight and BP were recollected as scheduled.
2.5 Outcome and other measures
We expressed physical activity in terms of Metabolic Equivalent-minutes (MET-min) and weekly activity level of 600 or more MET-min was considered to be adequate, in accordance with WHO recommendations (18). Diet was assessed in terms of number of servings of fruits or vegetables in a day. Standard definition of ‘serving’ was used as per WHO STEPS approach and a daily consumption of 5 or more servings of fruits or vegetables was considered to be adequate (18). Our primary outcome was the percentage/mean change in behavioural risk factors at the end of the study in the intervention group as compared to control group i.e. change in the proportion of subjects engaged in low physical activity (less than 600 MET-min per week) and proportion consuming inadequate diet (less than 5 servings of fruits/vegetables per day). Our secondary outcomes were changes in physiological risk factors (BMI, Blood Pressure-systolic and diastolic). These variables were expressed quantitatively and difference in means was assessed.
2.6 Statistical Analysis
Data was entered and cleaned in Excel and analyzed using SPSS version 21. Continuous/quantitative data was analysed using mean and standard deviation while categorical/ qualitative data data using proportions and percentages. Independent sample t-test (quantitative data) and Chi-square test (qualitative data) were used to compare baseline characteristic between intervention and control group respectively. Paired t-test was used to compare post-intervention data to pre-intervention data for continuous variables while Mcnemar test was used to compare post-intervention data to pre-intervention for categorical variables. A P value of less than 0.05 was taken to be statistically significant.
3. Results
3.1 Flowchart of participants in the study
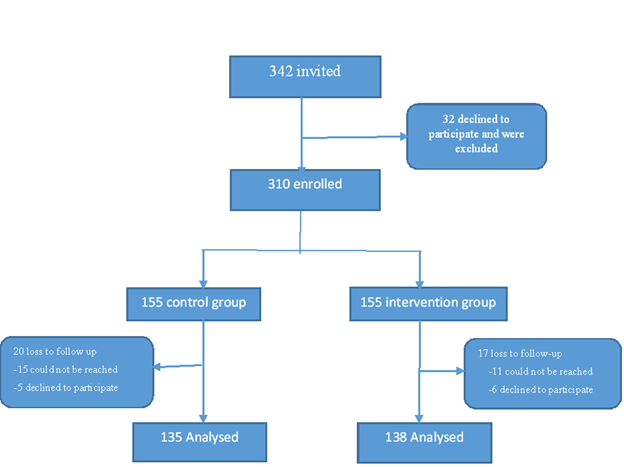
Figure 1 depicts the flow of participants in the study. We approached 342 individuals fulfilling the inclusion criteria and asked to enroll for the study. Of these, 9.4% (n=32) declined to participate. The remaining 310 subjects were allocated to control group (n=155) and intervention group (n=155) in a random manner (randomization in SPSS). Among the control group, 5.8% (n=20) were lost to follow-up. Among the intervention group, 4.9% (n=17) were lost to follow up. Hence, of the 310 enrolled participants, 273 completed the study, thus the completion rate was 88.1% (Figure 1).
3.2 Socio-demographic characteristics of participants in the intervention and control groups.
Table 1 shows the socio-demographic characteristics of the participants in control and intervention groups. The two groups were similar in terms of socio-demographic characteristics such as age, marital status, education, occupation and religion at baseline.
Table 1: Socio-demographic characteristics of the participants in the intervention and control group (chi-square)
|
Characteristic |
Intervention group |
Control group |
P value |
|
(n=140), n (%) |
(n=135), n (%) |
||
|
Age (years) |
0.783 |
||
|
18 – 24 |
52 (37.1) |
48 (36.5) |
|
|
25 – 29 |
47 (33.6) |
40 (30.4) |
|
|
30 – 34 |
31 (22.1) |
31 (23.0) |
|
|
≥ 35 |
10 (7.1) |
14 (10.4) |
|
|
Marital status |
0.822 |
||
|
Married |
91 (65.0) |
85 (63.7) |
|
|
Single/Widow/Divorced |
49 (35.0) |
48 (36.3) |
|
|
Occupation |
0.1 |
||
|
Housewife |
32 (22.9) |
20 (14,8) |
|
|
Peasant/Student |
50 (35.7) |
32 (23.7) |
|
|
Petit trading |
37 (26.4) |
56 (41.5) |
|
|
Employed |
21 (15.1) |
25 (20.0) |
|
|
Religion |
0.223 |
||
|
Catholic/Protestant |
100 (71.4) |
95 (70.4) |
|
|
Pentecostal |
28 (20.0) |
31 (23.0) |
|
|
None/Muslim |
12 (8.6) |
9 (6.7) |
|
|
Education |
0.734 |
||
|
None/Primary |
20 (14.3) |
22 (16.3) |
|
|
Secondary |
44 (31.4) |
47 (24.4) |
|
|
High School |
33 (23.6) |
33 (24.4) |
|
|
Tertiary |
43 (30.1) |
33 (24.4) |
3.3 Baseline data between intervention and control group
Table 2 and 3 shows the baseline data regarding smoking status, stress, alcohol consumption (categorical data) and physical activity, fruits/vegetable intake/day, knowledge of hypertension, overweight/obese, SBP and DBP in the control and intervention groups. No significant difference was found among all the variables at baseline.
Table 2: Comparing Baseline Categorical variables between Intervention and control group (Chi-square test)
|
Characteristic |
Intervention group |
Control group |
P value |
|
(n=140), n (%) |
(n=135), n (%) |
||
|
Smoking status |
0.666 |
||
|
Smoke |
3 (2.1) |
4 (2.9) |
|
|
Alcohol consumption |
0.551 |
||
|
Take alcohol |
29 (20.7) |
32 (23.7) |
|
|
Stressed up |
0.516 |
||
|
Yes |
64 (45.7) |
67 (49.6) |
|
|
Salt Consumption |
0.648 |
||
|
High salt consumers |
23 (16.4) |
25 (18.5) |
Table 3: Comparing Baseline Continuous Variables between Intervention and control group (Independent sample t-test)
|
Characteristic |
Intervention group |
Control group |
P value |
|
(n=140), Mean (SD) |
(n=135), Mean (SD) |
||
|
Physical activity (PA) |
0.219 |
||
|
MET/Min/week score (/600) |
183.00 (140.0) |
162.67 (133.13) |
|
|
Fruits/Vegetable |
0.901 |
||
|
Consumption/day (/5) |
3.26 (1.11) |
3.27 (1.14) |
|
|
Knowledge of hypertension |
0.476 |
||
|
Knowledge score (/7) |
3.30 (0.13) |
3.21 (0.41) |
|
|
Physiological Parameters |
|||
|
Overweight/obsessed |
0.637 |
||
|
BMI (kg/m2) |
27.68(4.58) |
27.92 (4.67) |
|
|
Systolic BP |
0.14 |
||
|
Mean SBP |
108.77 (12.22) |
110.87 (11.70) |
|
|
Diastolic BP |
0.903 |
||
|
Mean DBP |
67.27 (8.22) |
67.16 (10.42) |
|
3.4 Percentage/Mean change in lifestyle/physiological factors at Post intervention in both the intervention and control group
Table 4 & 5 shows the percentage/mean change in behaviour, knowledge and physiological factor scores after mHealth intervention (text messages) in the intervention group and no intervention in the control group.
For the categorical/nominal variables, percentage difference/scores of alcohol consumption, stress and high salt intake decreased significantly in intervention group but not in the control group. Alcohol consumption score decreased from 20.7 at baseline to 1.4 at post intervention (percentage difference=19.3, P<0.001). Stress decreased from 54.4 at baseline to 19.3 at post intervention (percentage difference=35.0, P=0.002). High salt intake decreased from 16.4 at baseline to 4.3 at post intervention (percentage difference=12.1, P=<0.001). Though all smokers in the intervention group quit smoking, this change wasn’t statistically significant between baseline and post intervention.
Similarly, for the continuous variables, physical activity (MET/min/week) was found to increase from an average of 183.00 at baseline to 417.27 at post intervention (Mean difference=234.5, P=<0.001). Fruits/vegetable consumption was found to increase from an average of 3.26 at baseline to 4.91 at post intervention (Mean difference=1.65, P=<0.001). Knowledge of hypertension was found to increase from an average of 3.30 at baseline to 6.16 at post intervention (Mean difference=12.1, P=<0.001). No statistically significant change in the above variables were found in the control group.
For the physiological parameters, no statistically significant change was found in the intervention group. However, in the control group, there was statistically significant increase in body weight, systolic and diastolic blood pressure. In the control group, BMI was found to increase from an average of 4.67 at baseline to 4.94 at post intervention (Mean difference=0.48, P=0.002). SBP was found to increase from an average of 11.70 at baseline to 12.56 at post intervention (Mean difference=3.08, P= <0.001). In the control group, BMI was found to increase from an average of 8.65 at baseline to 9.52 at post intervention (Mean difference=1.63, P= <0.001).
Table 4: Percentage change in lifestyle/physiological factors at Post intervention in both the intervention and control group (Mcnemar Test).
|
Characteristic |
Intervention group (n=140) |
Control group (n=135) |
||||
|
Baseline |
Post-intervention |
Difference % |
Baseline |
Post-intervention |
Mean difference |
|
|
Proportion (%) |
Proportion (%) |
(p-value) |
Proportion (%) |
Proportion (%) |
(p-value) |
|
|
Smoking |
3 (2.1) |
0 (0.0) |
-2.1 (0.250) |
4 (2.9) |
3 (2.2) |
-0.7 (1.00) |
|
Alcohol |
29 (20.7) |
2 (1.4) |
-19.3 (0.001) |
32 (23.7) |
29 (21.5) |
-2.2 (0.250) |
|
Stress |
76 (54.3) |
27 (19.3) |
-35 (0.002) |
67 (49.6) |
63 (46.7) |
- 2.9 (0.125) |
|
High salt consumers |
23 (16.4) |
6 (4.3) |
-12.1(0.001) |
25 (18.5) |
21 (15.6) |
-2.9 (0.344) |
Table 5: Mean change in lifestyle/physiological factors at Post intervention in both the intervention and control group (Paired t-test).
|
Characteristic |
Intervention group (n=140) |
Control group (n=135) |
||||
|
Baseline |
Post-intervention |
Mean difference (p-value) |
Baseline |
Post-intervention |
Mean difference |
|
|
Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
(p-value) |
||
|
PA (MET/min/week (/600)) |
183.00 (140.03) |
417.50 (140.23) |
234.5 (<0.001) |
8.55 (1.04) |
8.57 (1.05) |
0.02(0.51) |
|
Fruit/vegetable (/5) |
3.26 (1.11) |
4.91 (1.84) |
1.65 (<0.001) |
4.25 (0.76) |
4.28 (0.85) |
0.03 (0.74) |
|
Knowledge of HTN (/7) |
3.30 (1.10) |
6.16 (0.85) |
2.86 (<0.001) |
1.74 (0.33) |
1.71 (0.25) |
- 0.03 (0.54) |
|
Physiological Parameters |
||||||
|
BMI (kg/m2) |
27.68 (4.58) |
27.49 (4.19) |
0.19(0.537) |
27.95 (4.67) |
28.43 (4.94) |
0.48 (0.002) |
|
SBP (mmHg) |
108.74 (12.22) |
110.22 (10.43) |
1.48 (0.210) |
110.87 (11.70) |
113.96 (12.56) |
3.08 (<0.001) |
|
DBP (mmHg) |
67.29 (8.22) |
68.28 (7.18) |
0.99 (0.212) |
67.64 (8.65) |
69.27 (9.52) |
1.63(<0.001) |
SD= Standard Deviation
4. Discussion
This study reveals that using mHealth interventions such as text messages (SMS) and phone calls for BCC could be effective in improving inadequate fruits/vegetable intake, physical inactivity smoking cessation, stress reduction, decrease alcohol intake, decrease overweight/obese, maintain SBP and DBP and improve knowledge of hypertension which are all lifestyle factors of HDP. A number of studies in developed countries, have demonstrated the usefulness of mHealth interventions (test messages) to improve behavioural risk factors of hypertension. For example, an mHealth intervention promoting healthy diet, physical activity and gestational weight gain among pregnant women in Australia and results showed a significantly lower gestational weight gain (GWG) in the intervention group (7.8 kg ± 4.7 versus 9.7 kg ± 3.9; P =0.041) compared with the control group at intervention completion. Furthermore, Intervention group women reported significantly smaller reductions in total, light- and moderate-intensity physical activity from baseline to completion of the intervention (P = 0.001) compared with the control group, but no differences in consumption frequencies of key food groups (19).
In an Indian study by Sharma et al., (20), using mobile text messages and phone calls, the percentage of participants consuming inadequate diet reduced from 100% to 94.7% in the intervention group. Insufficient physical activity reduced from 41.6% to 35.3% in the intervention group while no change was observed in terms of percentage in the control group. Mean number of daily servings of fruits and vegetables increased from 1.2 to 2.8 (Z=-11.961, P=0.000) while in control group, it increased from 1.2 to 2.2 (Z=-12.041, P=0.000). In the same study, significant reductions were equally seen in the physiological risk factors in the intervention group as compared to control group. Mean BMI in intervention group reduced from 23.8 to 23.7 at the end of the intervention period (Z=-2.834, P=0.005). Mean systolic blood pressure reduced from 129.9 to 128.6 mmHg in the intervention group which was significant (Z=-3.824, P=0.000), though no change was recorded in the DBP. There was a marginal increase in mean systolic blood pressure in the control group (20). Similar results were reported by the current study.
A study in the UK (randomized control trial (RCT)) found that mobile intervention via SMS significantly improved the physical activity level of the intervention group as compared to control group. The study concluded that text messages aid the recall of, and could enhance interventions that target, plans and goals related to increased physical activity (21). A Swedish study evaluated the effectiveness of a weight loss program sent through SMS. It addressed diet regulation as well as physical activity and 12 months later, the experimental group had lost significantly more weight than the control group (22). A systematic review published in 2016 reviewed 15 studies evaluating mHealth and eHealth interventions for promotion of healthy diets and physical activity in LAMI countries. The results suggested that eHealth & mHealth interventions might be effective in improving physical activity and diet quality in LAMI countries. Overall, the review showed that 50% of the eHealth & mHealth interventions were effective in increasing physical activity, and 70% of the identified interventions were effective in improving diet quality (Müller et al., 2016).
A study was carried out in Holland on reducing alcohol use during pregnancy via health counselling by midwives and internet-based computer-tailored feedback (a cluster randomized trial). Multilevel multiple logistic regression analyses showed that computer-tailoring respondents stopped using alcohol more often compared to usual care respondents 6 months after baseline (53/68, 78% vs 51/93, 55%;P=.04) (23).
Do et al., (24), carried out a study to determine which eHealth interventions help people to stop smoking and results showed that smoking cessation interventions using web-based and mobile health (mHealth) platform resulted in significantly greater smoking abstinence, RR 2.03 (95% CI 1.7–2.03), and RR 1.71 (95% CI 1.35–2.16), respectively. Similarly, smoking cessation trials using tailored text messages (RR 1.80, 95% CI 1.54–2.10) and web-based information (RR 1.29, 95% CI 1.17–1.43) also increased cessation. In contrast, little or no benefit for smoking abstinence was found for computer-assisted interventions (RR 1.31, 95% CI 1.11–1.53) (24).
It is not possible to assess whether the phone calls or the text messages contributed more towards the change observed in this study. However, the feature of phone call in the mHealth package provided a gateway for two-way communication. The text messages provided continuous input of health messages and the phone calls served to reiterate those messages, follow-up on progress and provide motivation and positive reinforcement to the subjects. The strength of our study is that we evaluated behavioural and physiological risk factors for HDP. Considering that behavioural risk factors are self-reported and based on recall, they are prone to bias. However, Blood pressure and anthropometric measurements were taken by trained health personnel which greatly reduces bias. Though it was a hospital-based study, randomisation could have reduced the likelihood of participant interaction and pass on the health promotion messages to each other. Equally participants in the intervention and control group are likely not to have the same ANC schedule, which equally reduces the likeliness of interaction. Furthermore, the HDs and HFs were further apart, thus limiting the chances of interactions. These parameters help enhances the external validity of our study. The study nonetheless had some limitations. Firstly, the blinding of investigator wans’t possible which could be a source of bias in the study. Secondly, behavioural risk factors were self-reported and hence likely to recall and self-desirability bias. Lastly, because the sample size of the study was calculated based on the primary outcome (change in behavioural risk factors), it might be underpowered to detect the changes in the physiological risk factors which have lesser prevalence in the community.
5. Conclusion
This study has demonstrated the usefulness of mHealth for health promotion and lifestyle modification at community level in a less developed country. However, there is a necessity for more such studies, especially large-scale RCTs to be carried out to generate good quality evidence. This study was conducted to evaluate the effectiveness of mHealth via text messages in improving lifestyle factors of hypertension in pregnancy. Though inter-personal communication is the most effective means for BCC, it is somehow expensive to realise in terms of time, money and man-power. The most advantageous feature of mHealth that makes it a better choice is its cost effectiveness. With the growing burden of HDP among women, such cost effective and innovative measures will be needed that can easily reach the masses.
6. Acknowledgements
The authors would like to thank the Regional Delegate of the North West Region, the Directors of the respective facilities sampled into this study for their Administrative approval and all the regnant women who participated in the study for their sacrifice to ensure this piece of work was successful.
7. References
- Ye C, Ruan Y, Zou L, Li G, Li C, et al. The 2011 Survey on Hypertensive Disorders of Pregnancy (HDP) in China: Prevalence, Risk Factors, Complications, Pregnancy and Perinatal Outcomes 9(6) (2014).
- Duley L. The global impact of pre-eclampsia and eclampsia Semin Perinatol. 33(3) (2009):130-7.
- Ghulmiyyah L, Sibai B. Maternal mortality from preeclampsia/Eclampsia. Semin Perinatol 36(4)( 2012):56-9.
- WHO U, UNFPA and the World Bank. Trends in maternal mortality 1990-2008: Estimates developed by WHO, UNICEF, UNFPA and the World Bank. 2010. World Health Organization 10(2012).
- Organization WH. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. World Health Organization 10(2011).
- Roccella EJ. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. American Journal of Obstetrics & Gynecology 183(1)(2000):1-22.
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet 367(9516) (2006):1066–74.
- WH. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization 396(2009).
- Paudel R, Kwan L, Jitendra KS, Seok-Ju Y, Dilaram A, et al. Prevalence of behavioral risk factors of cardiovascular diseases and associated socio-economic factors among pregnant women in a rural area in Southern Nepal. BMC Pregnancy and Childbirth 18(484) (2018):1-9.
- Aryal K NS, Mehata S, Vaidya A, Singh S, Paulin F, et al. Non communicable diseases risk factors: STEPS Survey Nepal 2013. Kathmandu: Nepal Health Research Council 5(2014).
- Niraul S, Jha N, Shyangwa P. Alcohol consumption among women in a district of Eastern Nepal. Health Renaiss 11(3) (2014):205-12.
- Vandelanotte C, Müller AM, Short CE, Hingle M, et al. Past, present and future or e- & mHealth research to improve physical activity and dietary behaviors. Journal of Nutrition, Education and Behaviour 48(3) (2016):219-28.
- Burke LE, Ma J, Azar KM, Bennett GG, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 132(12) (2015):1157-213.
- Müller AM, Alley S, Schoeppe S, CV. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: A systematic review. International journal of Behavioural and Nutritional Activity 13(109) (2015).
- Burke LE, Ma J, Azar KM, Bennett GG, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart 132(12) (2015).
- Circulation. 132(12) (2015):1157-213.
- Müller AM, Alley S, Schoeppe S, Vandelanotte C. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: A systematic review. International Journal of Behavioral Nutrition and Physical Activity 13(109) (2016):1-14.
- Garg A, Anand T, Sharma U, Kishore J, et al. Prevalence of risk factors for chronic non-communicable diseases using WHO steps approach in an adult population in Delhi. Journal of Family Medicine and Primary Care 3(2) (2014):112-8.
- Ruth B, Catherine LG-C. The WHO STEP-wise approach to surveillance of non-communicable diseases (STEPS). Geneva: World Health Organisation (WHO) 106 (2003):1-50.
- Willcox JC, Wilkinson SA, Lappas M, Ball K, et al. A mobile health intervention promoting healthy gestational weight gain for women entering pregnancy at a high body mass index: the txt4two pilot randomised controlled trial. International Journal of Obstetricians and Gynaecologists 124 (2017):1718–28.
- Sharma M, Banerjee B, Ingle GK, Garg S. Effect of mHealth on modifying behavioural risk-factors of noncommunicable diseases in an adult, rural population in Delhi, India: mHealth All rights reserved 3(42) (2017):1-9.
- Prestwich A, Perugini M, Hurling R. Can implementation intentions and text messages promote brisk walking? A randomized trial: Health Psychology 29 (2010):40-9.
- Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study: Public Health Nutrition 12(12) (2009):2382-91.
- Nickie Y, van der Wulp NY, Hoving C, Eijmael K, et al. Reducing Alcohol Use During Pregnancy Via Health Counseling by Midwives and Internet-Based Computer-Tailored Feedback: A Cluster Randomized Trial. Journal of Medical Internet Research 16(12) (2014):1-9.
- Do HP, Tran BX, Pham QL, Nguyen LH, et al. Which eHealth interventions are most effective for smoking cessation? A systematic review: Patient Preference and Adherence 12 (2018):2065-84.