Does Mitral Valve Commissural Calcification Predicts Restenosis at Long-Term Follow-up After Percutaneous Balloon Mitral Valvuloplasty?
Article Information
Samir Rafla1*, Tarek Bishay2
1Alexandria University, Faculty of Medicine, Cardiology Department, Alexandria, Egypt
2National Heart Institute, Cardiology Department, Cairo, Egypt
*Corresponding author: Samir Rafla, Alexandria University, Faculty of Medicine, Cardiology Department, Alexandria, Egypt
Received: 23 December 2019; Accepted: 30 December 2019; Published: 06 January 2020
Citation: Samir Rafla, Tarek Bishay. Does Mitral Valve Commissural Calcification Predicts Restenosis at Long-Term Follow-up After Percutaneous Balloon Mitral Valvuloplasty?. Cardiology and Cardiovascular Medicine 4 (2020): 028-038.
Share at FacebookAbstract
Percutaneous balloon mitral valvuloplasty (PBMV) is an effective form of treatment for patients with mitral valve stenosis (MS). The commissural (com.) appearance is a factor that is not assessed by the mitral valve (MV) scores (as the Wilkins score). The aim of this study was to determine whether the presence of calcium in the MV coms. as demonstrated echocardiographically, could predict restenosis at 3 years follow-up after PBMV. 220 consecutive patients with rheumatic MS who underwent successful PBMV by using the Inoue balloon catheter were studied prospectively. Com. calcification (calc.) was present in 70 patients (32%). Com. splitting occurred immediately after PBMV in all the 220 patients studied. Bilateral com. splitting was present more significantly in patients without com. calc. than in patients with com. calc. (P < 0.001). 140 patients presented at 3 years follow-up. Com. calc. was present in 35 patients (25%) while the other 105 patients (75%) had no com. calc. Bilateral com. splitting was present more significantly in patients without com. calc. than in patients with com. calc. (P < 0.001). Severe MR was present in 20 patients (14.3%). It was present more significantly in patients with com. calc. than in patients without com. calc. (P < 0.001). Restenosis occurred in 30 patients (21.4%). Conclusion, patients with com. calc. have a lower incidence of bilateral com. splitting; have a higher incidence of severe MR at one year and at 3 years follow-up after PBMV. Old age, large LAD, high total echo score of the MV, MV score ? 8, lower MVA before PBMV, low incidence of bilateral com. splitting, low MVA after PBMV and the presence of com. calc. are significant predictors of restenosis at 3 years follow-up. Com. calc. is a strong predictor of restenosis at 3 years follow-up after PBMV.
Keywords
Percutaneous balloon mitral valvuloplasty; Restenosis; Rheumatic Mitral Stenosis; Commissural calcification
Percutaneous balloon mitral valvuloplasty articles, Restenosis articles, Rheumatic Mitral Stenosis articles, Commissural calcification articles
Article Details
Abbreviations:
PBMV = Percutaneous balloon mitral valvuloplasty); COM-CALC = commissural calcification; MVA= mitral valve area; LAD= left atrial diameter.; F.C.= Functional Class.
Introduction
PBMV is an effective form of treatment for MS. It is important to identify patients who would benefit from this procedure. In the selection of patients for PBMV, MV morphology is conventionally assessed by echocardiographic scores (as Wilkins score) [1] based on a semiquantitative assessment of leaflet mobility, thickening, calcification and subvalvular thickening, however, these scores do not include com. assessment. As com. splitting is the dominant mechanism by which MS is relieved by PBMV [2-11], assessment of the com. morphology should logically be an important part of the evaluation of patients with MS considered for PBMV.
Aim of the work
To determine whether the presence of calcium in the mitral valve coms., as demonstrated echocardiographically, could predict restenosis at 3 years follow-up after PBMV.
Patients and Methods
235 consecutive patients with rheumatic MS who were scheduled for PBMV were studied prospectively at the NHI during the period between August 2008 and March 2012.
Exclusion criteria:
- Patients with intracardiac masses or thrombi.
- Patients with previous PBMV or surgical mitral commissurotomy.
- Patients who developed suboptimal outcome after the procedure.
- Patients who developed severe MR after the procedure.
Every patient was subjected to:
- Complete history taking.
- Clinical examination. Evaluation of the NYHA, F.C. was done.
- Chest X-Ray.
- PBMV procedure: was done by using the Inoue balloon catheter technique [2].
- Transthoracic echocardiography (TTE): was done before the procedure, at one-year follow-up and at 3 years follow up.
* MVA was measured by planimetry of the mitral orifice in the parasternal short-axis view. The MV was scored using the criteria described by Wilkins et al. [1]. MV score ³ 8 was considered high [12].
* Optimal (successful) outcome was considered if the MVA post PBMV was ³ 1.5cm2 and an increase in MVA of at least 25% from the initial MVA was achieved [9].
* Com. Morphology was assessed in the parasternal short axis view. Both anterolateral and posteromedial coms. were individually examined. Com. calc. was either unilateral or bilateral. Unilateral com. calc. was either anterolateral or posteromedial.
* Com. splitting was identified as a new area of echo dropout along the long axis of the MV orifice which was contiguous with the orifice [12]. Com. splitting was either unilateral or bilateral. Unilateral com. splitting was either anterolateral or posteromedial.
Transesophageal Echocardiography (TEE): was done before PBMV to all the patients.
One-year follow-up:
* TTE was done to the patients who presented at one-year follow-up.
* TEE was done to the patients who developed severe MR.
* Restenosis: echo restenosis was defined at follow-up as a loss of 50% of the initial gain and a MVA < 1.5 cm2. [3]
3 Years follow-up:
* TTE was done to the patients who presented at 3 year follow-up.
* TEE was done to the patients who developed severe MR.
* Informed consent was obtained from the patients.
Statistical Analysis
* Quantitative data were expressed as mean ± standard deviation.
* Student’s t test was used to compare quantitative data between 2 groups.
* Discrete variables were compared with Chi squared test.
* A value of p < 0.05 was considered statistically significant. P < 0.01 was considered highly significant.
Results
* 235 consecutive patients with MS who were scheduled for PBMV were studied prospectively. In 3 patients, the procedure was not completed due to inability to cross the interatrial septum. Cardiac tamponade occurred in 3 patients as a complication of transseptal puncture. Suboptimal outcome occurred in 2 patients. So, these 8 patients were excluded from the study. 7 patients developed severe MR. All of them had a high total MV score (³ 8/16). Also, all of them had com. calc. (unilateral). TEE was done to all of them. The mechanism of severe MR in these 7 patients were tears of the mitral leaflets. Leaflet tears were related to the calcified com. if splitting occurred in that com. (2 patients) and to the contralateral com. if the calcified com. did not split (5 patients). These 7 patients were also excluded from the study. So, the study population consisted of 220 patients. All of them were in NYHA, F.C. > II.
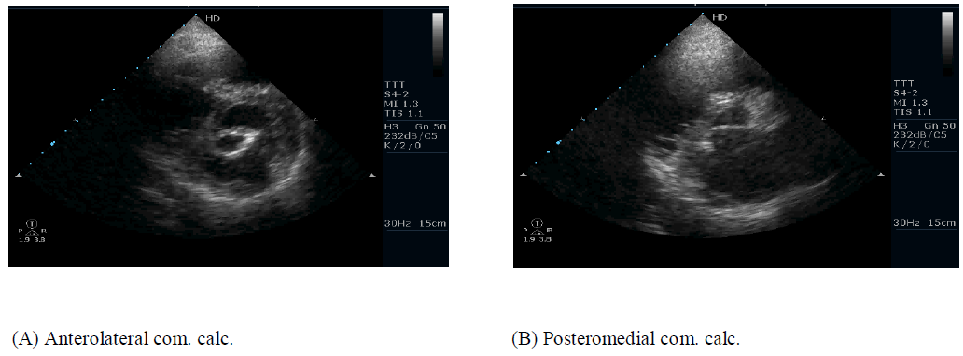
* Com. calc. was present in 70 patients (32%). It was unilateral com. calc. {43 patients (61.4%) had anterolateral com. calc. and 27 patients (38.6%) had posteromedial com. calc. (Figure 1)}. The other 150 patients (68%) had no com. calc.
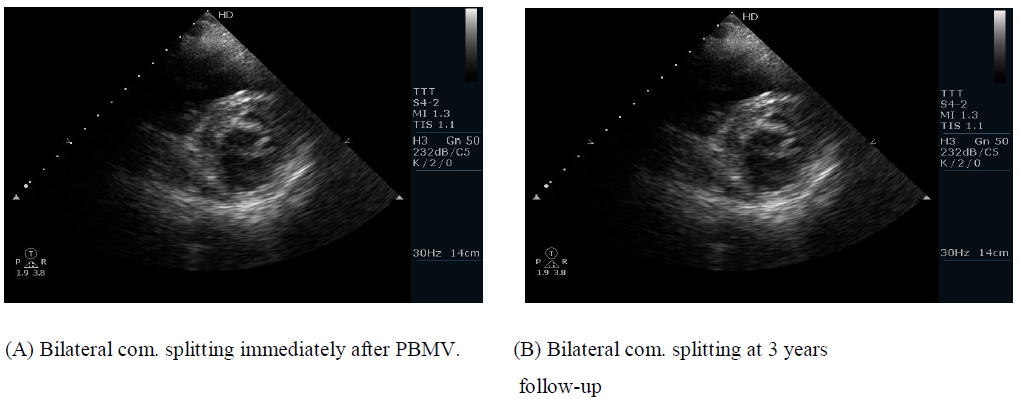
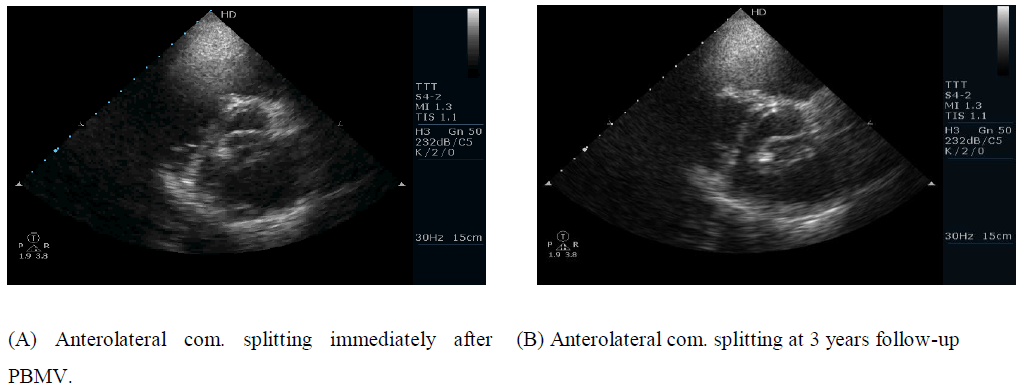
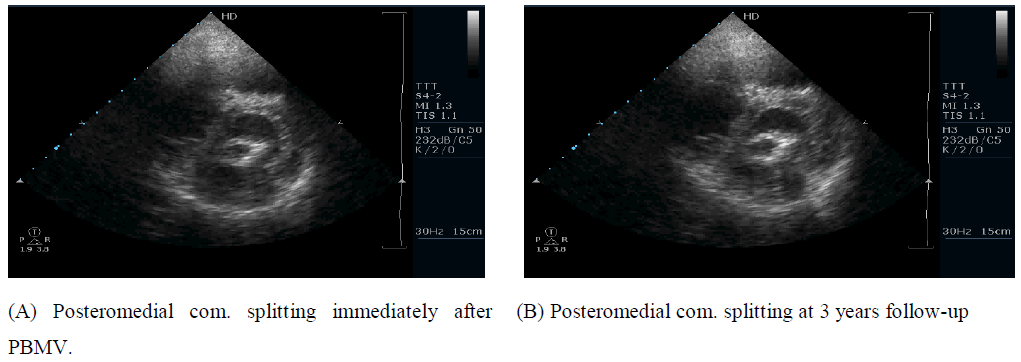
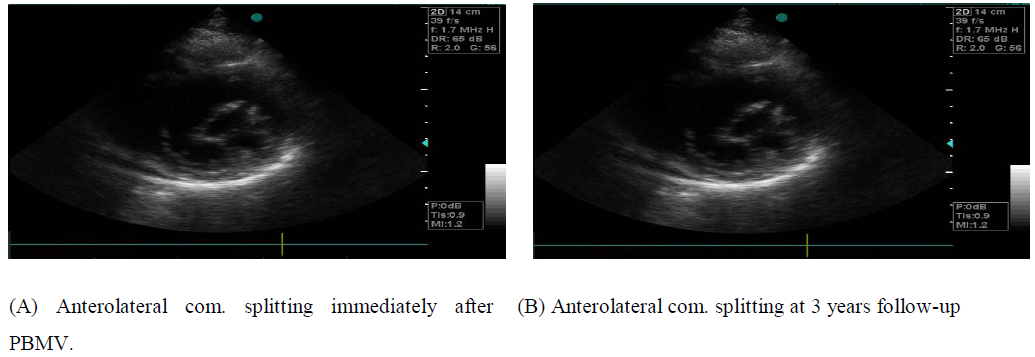
* Com. splitting occurred immediately after PBMV in all the 220 patients studied. Of the 70 patients with com. calc., 10 patients (14.3%) had bilateral com. splitting (Figure 2) while 60 patients (85.7%) had unilateral com. splitting {40 patients (66.7%) had anterolateral com. splitting (Figure 3) and 20 patients (33.3%) had posteromedial com. splitting (Figure 4). Of the 150 patients without com. calc., 120 patients (80%) had bilateral com. splitting while 30 patients (20%) had unilateral com. splitting {19 patients (63.3%) had anterolateral com. splitting (Figure 5) and 11 patients (36.7%) had posteromedial com. splitting}. Bilateral com. splitting was present more significantly in patients without com. calc. than in patients with com. calc. (P < 0.001).
One-year follow-up results:
* 190 patients presented at one year after PBMV. Com. calc. was present in 56 patients (29.5%). 34 patients (60.7%) had anterolateral com. calc. and 22 patients (39.3%) had posteromedial com. calc. The other 134 patients (70.5%) had no com. calc.
* Com. splitting was present in all the 190 patients. No patient who had com. splitting immediately after PBMV developed com. fusion of any com. at one-year follow-up. Of the 56 patients with com. calc., 7 patients (12.5%) had bilateral com. splitting while 49 patients (87.5%) had unilateral com. splitting {32 patients (65.3%) had anterolateral com. splitting and 17 patients (34.7%) had posteromedial com. splitting}. Of the 134 patients without com. calc., 106 patients (79.1 %) had bilateral com. splitting while 28 patients (20.9 %) had unilateral com. splitting {18 patients (64.3 %) had anterolateral com. splitting and 10 patients (35.7 %) had posteromedial com. splitting}. Bilateral com. splitting was present more significantly in patients without com. calc. than in patients with com. calc. (P < 0.001).
* Severe MR was present in 17 patients (8.9%). None of them had tears of the mitral leaflets. Of the 56 patients with com. calc., 14 patients (25%) had severe MR. Of the 134 patients without com. calc., 3 patients (2.3%) had severe MR. Severe MR was present more significantly in patients with com. calc. than in patients without com. calc. (P < 0.001).
* Restenosis occurred in 10 patients (5.3%).
* All the 17 patients with severe MR and the 10 patients with restenosis were not followed up.
3 years follow-up results:
* 140 patients presented at 3 years after PBMV.
* Com. calc. was present in 35 patients (25%). 21 patients (60%) had anterolateral com. calc. and 14 patients (40%) had posteromedial com. calc. The other 105 patients (75%) had no. com. calc.
* Com. splitting was present in all the 140 patients. No patient who had com. splitting at one-year follow-up after PBMV developed com. fusion of any com. at 3 years follow-up.
* Of the 35 patients with com. calc., 4 patients (11.4%) had bilateral com. splitting (Figure 2) while 31 patients (88.6%) had unilateral com. splitting {20 patients (64.5%) had anterolateral com. splitting (Figure 3) and 11 patients (35.5%) had posteromedial com. splitting (Figure 4)}. Of the 105 patients without com. calc., 79 patients (75.2 %) had bilateral com. splitting while 26 patients (24.8 %) had unilateral com. splitting {17 patients (65.4 %) had anterolateral com. splitting (Fig. 5) and 9 patients (34.6 %) had posteromedial com. splitting}.
* Bilateral com. splitting was present more significantly in patients without com. calc. than in patients with com. calc. (P < 0.001).
* Severe MR was present in 20 patients (14.3%). None of them had tears of the mitral leaflets. Of the 35 patients with com. calc., 15 patients (42.9%) had severe MR. Of the 105 patients without com. calc., 5 patients (4.8%) had severe MR. Severe MR was present more significantly in patients with com. calc. than in patients without com. calc. (P < 0.001).
* Restenosis occurred in 30 patients (21.4%) (Figure 3).
* MV score ³ 8 was present in 59 patients (42.1%). Of the 35 patients with com. calc., 30 patients (85.7%) had MV score ³ 8. Of the 105 patients without com. calc., 29 patients (27.6%) had MV score ³ 8. MV score ³ 8 was present more significantly in patients with com. calc. than in patients without com. calc. (P < 0.001).
* The patients were classified into 2 groups:
Group I: (Restenosis group):
* Included 30 patients (21.4%) with restenosis.
* Their age ranged from 24 to 47 years old with a mean of 35.03 ± 6.64 years. 20 patients (66.7%) were females (F) and 10 patients (33.3%) were males. 20 patients (66.7%) were in sinus rhythm (SR) and 10 patients (33.3%) were in atrial fibrillation (AF). LAD ranged from 4.5 to 5.8 cm with a mean of 5.12 ± 0.38 cm. Total echo score of the MV ranged from 6.0 to 10.0 with a mean of 8.03 ± 1.61. MV score ³ 8 was present in 20 patients (66.7%). MVA before PBMV ranged from 0.6 to 1.0 cm2 with a mean of 0.80 ± 0.15 cm2. Mild MR before PBMV was present in 11 patients (36.7%). Com. calc. was present in 30 patients (100%). Bilateral com. splitting was present in two patients (6.7%). MVA immediately after PBMV ranged from 1.6 to 2.1 cm2 with a mean of 1.82 ± 0.18 cm2.
Group II: (No restenosis group):
* Included 110 patients (78.6%) without restenosis.
* Their age ranged from 15 to 39 years old with a mean of 25.54 ± 4.89 years. 70 patients (63.6%) were females and 40 patients (36.4%) were males. 76 patients (69%) were in SR and 34 patients (31%) were in AF. LAD ranged from 4.2 to 5.7 cm with a mean of 4.91 ± 0.51 cm. Total echo score of the MV ranged from 6.0 to 9.0 with a mean of 6.90 ± 1.10. MV score ³ 8 was present in 39 patients (35.4%). MVA before PBMV ranged from 0.7 to 1.2 cm2 with a mean of 0.90 ± 0.19 cm2. Mild MR before PBMV was present in 38 patients (34.5%). Com. calc. was present in 5 patients (4.5%). Bilateral com. splitting was present in 81 patients (73.6%). MVA immediately after PBMV ranged from 1.8 to 2.4 cm2 with a mean of 2.10 ± 0.24 cm2.
(3) Predictors of restenosis at 3 years follow-up: (Table 1)
* Several factors were compared in both groups. The factors analyzed were: age, gender, rhythm, LAD, total echo score of the MV, MV score ³ 8, MVA before PBMV, Mild MR before PBMV, bilateral com. splitting, MVA immediately after PBMV and com. calc.
Group IRestenosis (30) |
Group II No restenosis (110) |
P Value |
|
|
Age |
35.03 ± 6.64 |
25.54 ± 4.89 |
P < 0.001 |
|
Gender (F) |
20 (66.7%) |
70 (63.6%) |
NS |
|
Rhythm (AF) |
10 (33.3%) |
34 (31%) |
NS |
|
LAD |
5.12 ± 0.38 |
4.91 ± 0.51 |
P < 0.05 |
|
MV score |
8.03 ± 1.61 |
6.90 ± 1.10 |
P < 0.001 |
|
MV score ³ 8 |
20 (66.7%) |
39 (35.4%) |
P < 0.01 |
|
MVA before |
0.80 ± 0.15 |
0.90 ± 0.19 |
P < 0.01 |
|
Mild MR before |
11 (36.7%) |
38 (34.5%) |
NS |
|
Bilateral com. splitting |
2 (6.7%) |
81 (73.6%) |
P < 0.001 |
|
MVA after |
1.82 ± 0.18 |
2.10 ± 0.24 |
P < 0.001 |
|
Com. calc. |
30 (100%) |
5 (4.5%) |
P < 0.001 |
Table 1: Predictors of restenosis at 3 years follow-up.
* Patients with restenosis (group I) at 3 years follow-up had:
- An older age (P < 0.001).
- A larger LAD (P < 0.05).
- A higher total echo score of the MV (P < 0.001).
- A higher incidence of MV score ³ 8 (P < 0.01).
- A lower MVA before PBMV (P < 0.01).
- A lower incidence of bilateral com. splitting (P < 0.001).
- A lower MVA after PBMV (P < 0.001).
- The presence of com. calc. (P < 0.001).
* So, old age, large LAD, high total echo score of the MV, MV score ³ 8, low MVA before PBMV, low incidence of bilateral com. splitting, low MVA after PBMV and the presence of com. calc. were significant predictors of restenosis at 3 years follow-up.
* NYHA, F.C. > II was present in 26 patients (86.7%) of the patients with restenosis while it was present in 22 patients (20%) of the patients without restenosis. NYHA, F.C. > II was present more significantly in patients with restenosis than in patients without restenosis (P < 0.001) (Table 2). So patients with restenosis developed a worse F.C. in the majority of them.
* Severe MR occurred in 15 patients (42.9%) of the patients with restenosis, while it occurred in 5 patients (4.8%) of the patients without restenosis. Severe MR occurred more significantly in patients with restenosis than in patients without restenosis (P < 0.001) (Table 2).
Group IRestenosis (30) |
Group II No restenosis (110) |
P Value |
|
|
NYHA, F.C. > II |
26 (86.7%) |
22 (20%) |
P < 0.001 |
|
Severe MR |
15 (42.9%) |
5 (4.8%) |
P < 0.001 |
Table 2: Comparison between the 2 groups as regards NYHA, F.C. and Severe MR at 3 years follow-up.
Discussion
The immediate success rate and long-term outcome of PBMV are dependent on the underlying MV morphology. However, the com. appearance is a factor that is not assessed by the MV scores (as the Wilkins score).
The present study was designed to determine whether the presence of calcium in the MV Coms., as demonstrated echocardiographically, could predict restenosis at 3 years follow-up after PBMV.
In the present study, 220 consecutive patients with MS who underwent successful PBMV were studied prospectively. Com. calc. was present in 70 patients (32%). It was unilateral com. calc. It is to be noticed here in the present study that no patient studied had bilateral com. calc., the reason for this is that all the patients with MS and bilateral com. calc. had a very high total echo score (Wilkins Score) and from the beginning, none of them was scheduled for PBMV. Sutaria et al. [11] reported the same finding in their patients studied.
It has been documented in the literature that the mechanism of MVA increase after PBMV is splitting of one or both of the fused coms. Also it has been documented that patients with bilateral com. splitting have a higher increase in MVA than patients with unilateral com. splitting [2-11].
In the present study, com. splitting occurred in all the patients studied. The reason for this is that all the 220 patients studied had undergone a successful procedure and patients with suboptimal outcome were excluded from the study. In the present study, bilateral com. splitting occurred more significantly in patients without com. calc. than in patients with com. calc. immediately after PBMV, at one-year follow-up and at 3 years follow-up. Since com. splitting is the dominant mechanism by which MS is relieved by PBMV, so, direct assessment of the MV com. morphology should be an important part of the evaluation of patients with MS considered for PBMV and not to depend only on other scores of the MV as they do not include com. assessment.
In the present study, 7 patients were excluded because they developed severe MR immediately after PBMV. All of them had. com. calc. At one-year follow-up and at 3 years follow-up, severe MR was present more significantly in patients with com. calc. than in patients without com. calc. In agreement with this result, Cannan et al., [10] reported the same result at a mean follow-up period of 1.8 years.
In the present study, restenosis occurred in 30 patients (21.4%) at 3 years follow-up. Thomas et al., [9] reported restenosis in 21% of their patients at one-year follow-up. Desideri et al., [13] reported restenosis in 20% of their patients followed for a mean period of 19 months. Zeitoun et al., [14] reported restenosis in 15% of their patients followed for a mean period of 16 months. These reports have a different and variable durations of follow-up compared to the present study.
In the present study, the patients who presented at 3 years follow-up were classified into 2 groups. Group I included 30 patients (21.4%) with restenosis and group II included 110 patients (78.6%) without restenosis.
To determine the factors predicting restenosis at 3 years follow-up, several factors were compared in both groups. Old age, large LAD, high total echo score of the MV, MV score ³ 8, low MVA before PBMV, low MVA after PBMV were significant predictors of restenosis at 3 years follow-up in the present study. This result is in agreement with the results of Thomas et al., [9], Desideri et al., [13] and Zeitoun et al., [14] but with a variable durations of follow-up periods.
Low incidence of bilateral com. splitting was a significant predictor of restenosis at 3 years follow-up in the present study. Cannan et al., [10] and Fatkin et al., [12] reported that bilateral com. splitting was a significant predictor of a good outcome after PBMV. Com. calc. was a significant predictor of restenosis at 3 years follow-up in the present study. We did not find in the literature any report evaluating the role of com. calc. for predicting restenosis at 3 years after PBMV to compare the result of the present study with it.
In the present study, patients with restenosis developed a worse F.C. in the majority of them. Similar result was reported by Thomas et al., [9] Desideri et al., [13] and Zeitoun et al., [14] but with a variable period of follow-up. Babu et al. [15] validated the importance of assessing the morphology of mitral valve commissures.
Conclusions and Recommendations
- Patients with com. calc. have a lower incidence of bilateral com. splitting than patients without com. calc. after PBMV, at one year and at 3 years follow-up.
- Patients with com. calc. have a higher incidence of severe MR at one year and at 3 years follow-up after PBMV.
- Restenosis occurs in 21.4% of the patients at 3 years follow-up after PBMV.
- Old age, large LAD, high total echo score of the MV, MV score ³ 8, low MVA before PBMV, low incidence of bilateral com. splitting, low MVA after PBMV and the presence of com. calc. are significant predictors of restenosis at 3 years follow-up after PBMV.
- calc. is present in all the patients who develop restenosis at 3 years follow-up after PBMV. So, com. calc. is a strong predictor of restenosis at 3 years follow-up after PBMV.
- Patients with restenosis at 3 years follow-up after PBMV have a worse NYHA F.C. than patients without restenosis.
- Patients with restenosis at 3 years after PBMV have a higher incidence of severe MR than patients without restenosis.
It is recommended that every effort should be done by the echo operators to evaluate the MV coms. searching for calc. and not to depend only on the scores of the MV for evaluating the patients before doing PBMV.
Compliance with Ethical Standards:
Conflicts of interest:
None
Research involving human participants:
Any transesophageal echo done to the patients was for their benefit, no money taken, no injuries happened.
All procedures performed in our study that involved human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent:
Informed consent was obtained from all individual participants included in the study.
Funding:
No funds were received from any agent.
References
- Wilkins GT, Weyman A.E, Abascal VM, Block P and Palacios IF. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 60 (1988): 299.
- Inoue K, Owaki T, Nakamura T, Kitamura F, Miyamoto N. Clinical application of transvenous mitral commissurotomy by a new balloon catheter. J Thorac Cardiovasc Surg 87 (1987): 394-402.
- Al-Zaibag M, Ribeiro PA and Al-Fagih MR. Percutaneous double balloon mitral valvotomy for rheumatic mitral valve stenosis. Lancet 1 (1986): 757.
- Block PC, Palacios IF, Jacobo MI and Fallon JT. Mechanism of percutaneous mitral valvotomy. Am J Cardiol 59 (1987): 178.
- Kaplan JD, Isner JM, Karas RH, Halaburka KR, Ronstam MA, Hongen TJ, Cleveland RJ. and Salem DN. In vitro analysis of mechanism of balloon valvuloplasty of stenotic mitral valves. Am J Cardiol 59 (1987): 318.
- Reid CL, Mekay CR, Chandraratna PA, Kawanishi DT and Rahimtoola SH. Mechanism of increase in mitral valve area and influence of anatomic features in double balloon catheter, catheter balloon valvuloplasty in adults with rheumatic mitral stenosis. A Doppler and two-dimensional echocardiography. Circulation 3 (1987): 76.
- Applebaum R.M, Kasliwal R.R, Kanojia A, Seth A, Bhandari S, Trehan N, Winer H.E, Tunick P.A, and Kronzon I: Utility of three-Dimensional echocardiography during balloon mitral valvuloplasty. J Am Coll Cardiol 32 (1988): 1504.
- Wilkins GT, Weyman AE, Abascal VM, Block PC and Palacios IF. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 60 (1988): 299.
- Thomas MR, Monaghan MJ, Michalis LK and Jewitt DE. Echocardiographic restenosis after successful balloon dilatation of the mitral valve with the Inoue balloon: Experience of a United Kingdom Centre: Br Heart J 69(1993): 418.
- Cannan CR, Nishimura RA, Reeder GS, Ilstrup DR, Larson DR, Holmes DR and Tajik AJ. Echocardiographic assessment of commissural calcium: A simple predictor of outcome after percutaneous mitral balloon valvotomy. J Am Coll Cardiol 29 (1997): 175.
- Sutaria N, Shaw TRD, Prendergast B and Northridge D. Transesophageal echocardiographic assessment of mitral valve commissural morphology predicts outcome after balloon mitral valvotomy. Heart 92 (2006): 52.
- Fatkin D, Roy P, Morgan JJ. and Feneley MP. Percutaneous balloon mitral valvotomy with the Inoue single-balloon catheter: Commissural morphology as a determinant of outcome. J Am Coll Cardiol 21 (1993): 390.
- Desideri A, Vanderperren O, Serra A, Barraud P, Petitclerc R, Lesperance J, Dyrda I, Crepeau J and Bonan R.: Long-term (9 to 33 months) Echocardiographic follow-up after successful percutaneous mitral commissurotomy. Am. J. Cardiol 69 (1992): 1602.
- Zeitoun DM, Brochet E, Holmin C, Rosenbaum D, Cormier B, Serfaty J, Iung B and Vahanian A. Three-dimensional evaluation of the mitral valve area and commissural opening before and after percutaneous mitral commissurotomy in patients with mitral stenosis. Eur Heart J 28 (2007): 72.
- D Sarath Babu,KP Ranganayakulu,D Rajasekhar,V. Vanajakshamma,andT. Pramod Kumar. Assessment of mitral valve commissural morphology by transoesophageal echocardiography predicts outcome after balloon mitral valvotomy. Indian Heart J 65 (2013): 269–275.