Differences in Sagittal Balance in Patients with and without Degenerative Spondylolisthesis Who are Surgically Treated for Spinal Stenosis. A Comparative Study
Article Information
Bougiouklis Dimitrios1*, Patsiaouras Thomas2
1Department of Orthopaedics and Traumatology, General Hospital of Pyrgos, Greece
2Department of Orthopaedics, General Hospital Asklepieion Voulas, Athens, Greece
*Corresponding Author: Bougiouklis Dimitrios, Department of Orthopaedics and Traumatology, General Hospital of Pyrgos, 27100, Greece
Received: 30 December 2019; Accepted: 10 January 2020; Published: 23 January 2020
Citation:
Bougiouklis Dimitrios, Patsiaouras Thomas. Differences in Sagittal Balance in Patients with and without Degenerative Spondylolisthesis Who are Surgically Treated for Spinal Stenosis. A Comparative Study. Journal of Spine Research and Surgery 2 (2020): 007-016.
Share at FacebookAbstract
Introduction: In pathogenesis of degenerative spondylolisthesis (DS) and its development, several predisposing factors have been advocated. However, the role of lumbar sagittal alignment has not been well studied yet. The purpose of this retrospective study was to analyze the sagittal spinopelvic alignment and to compare these parameters between patients with and without degenerative spondylolisthesis who were surgically treated for lumbar spinal stenosis.
Materials and Methods: Between 2008-2018, we studied 68 patients who underwent surgery for lumbar spinal canal stenosis. 34 of these patients, suffered by DS (group 1), and the other 34, age- and gender-matched patients, not presented DS (group 2). Surgical treatment was realized after six months of unsuccessful conservative treatment. Spinopelvic parameters including pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), L4 slope, L5 slope, thoracic kyphosis (TK), lumbar lordosis (LL), segmental lumbar lordosis (SLL) and sagittal balance were compared between the two groups. In the group 1, the slippage grade (% slip) was also evaluated.
Results: PI, SS, L4 slope, L5 slope, TK and LL in the group 1 were significantly greater than those in the group 2, and PI had positive correlation with % slip (p<0.05). The SLL of patients with DS was significantly lower than those without DS. In the group 1, there was a strong correlation between the PI and the SS (p<0.001), rather than with the PT (p<0.01). Between the two groups there was no significant difference in PT.
Conclusions: In patients with degenerative spondylolisthesis, PI was significantly greater than that in patients without DS and PI had positive correlation with the percentage of slippage. Greater PI turns to be a predisposing factor to the development and the progression of vertebral sliding. On the other hand, patients who suffer
Keywords
Degenerative, Spondylolisthesis, Spine Stenosis, Spinal Alignment, Pelvic Incidence, Lumbar Lordosis, Pelvis Shape
Degenerative articles Degenerative Research articles Degenerative review articles Degenerative PubMed articles Degenerative PubMed Central articles Degenerative 2023 articles Degenerative 2024 articles Degenerative Scopus articles Degenerative impact factor journals Degenerative Scopus journals Degenerative PubMed journals Degenerative medical journals Degenerative free journals Degenerative best journals Degenerative top journals Degenerative free medical journals Degenerative famous journals Degenerative Google Scholar indexed journals Spondylolisthesis articles Spondylolisthesis Research articles Spondylolisthesis review articles Spondylolisthesis PubMed articles Spondylolisthesis PubMed Central articles Spondylolisthesis 2023 articles Spondylolisthesis 2024 articles Spondylolisthesis Scopus articles Spondylolisthesis impact factor journals Spondylolisthesis Scopus journals Spondylolisthesis PubMed journals Spondylolisthesis medical journals Spondylolisthesis free journals Spondylolisthesis best journals Spondylolisthesis top journals Spondylolisthesis free medical journals Spondylolisthesis famous journals Spondylolisthesis Google Scholar indexed journals Spine Stenosis articles Spine Stenosis Research articles Spine Stenosis review articles Spine Stenosis PubMed articles Spine Stenosis PubMed Central articles Spine Stenosis 2023 articles Spine Stenosis 2024 articles Spine Stenosis Scopus articles Spine Stenosis impact factor journals Spine Stenosis Scopus journals Spine Stenosis PubMed journals Spine Stenosis medical journals Spine Stenosis free journals Spine Stenosis best journals Spine Stenosis top journals Spine Stenosis free medical journals Spine Stenosis famous journals Spine Stenosis Google Scholar indexed journals Spinal Alignment articles Spinal Alignment Research articles Spinal Alignment review articles Spinal Alignment PubMed articles Spinal Alignment PubMed Central articles Spinal Alignment 2023 articles Spinal Alignment 2024 articles Spinal Alignment Scopus articles Spinal Alignment impact factor journals Spinal Alignment Scopus journals Spinal Alignment PubMed journals Spinal Alignment medical journals Spinal Alignment free journals Spinal Alignment best journals Spinal Alignment top journals Spinal Alignment free medical journals Spinal Alignment famous journals Spinal Alignment Google Scholar indexed journals Pelvic Incidence articles Pelvic Incidence Research articles Pelvic Incidence review articles Pelvic Incidence PubMed articles Pelvic Incidence PubMed Central articles Pelvic Incidence 2023 articles Pelvic Incidence 2024 articles Pelvic Incidence Scopus articles Pelvic Incidence impact factor journals Pelvic Incidence Scopus journals Pelvic Incidence PubMed journals Pelvic Incidence medical journals Pelvic Incidence free journals Pelvic Incidence best journals Pelvic Incidence top journals Pelvic Incidence free medical journals Pelvic Incidence famous journals Pelvic Incidence Google Scholar indexed journals Lumbar Lordosis articles Lumbar Lordosis Research articles Lumbar Lordosis review articles Lumbar Lordosis PubMed articles Lumbar Lordosis PubMed Central articles Lumbar Lordosis 2023 articles Lumbar Lordosis 2024 articles Lumbar Lordosis Scopus articles Lumbar Lordosis impact factor journals Lumbar Lordosis Scopus journals Lumbar Lordosis PubMed journals Lumbar Lordosis medical journals Lumbar Lordosis free journals Lumbar Lordosis best journals Lumbar Lordosis top journals Lumbar Lordosis free medical journals Lumbar Lordosis famous journals Lumbar Lordosis Google Scholar indexed journals Pelvis Shape articles Pelvis Shape Research articles Pelvis Shape review articles Pelvis Shape PubMed articles Pelvis Shape PubMed Central articles Pelvis Shape 2023 articles Pelvis Shape 2024 articles Pelvis Shape Scopus articles Pelvis Shape impact factor journals Pelvis Shape Scopus journals Pelvis Shape PubMed journals Pelvis Shape medical journals Pelvis Shape free journals Pelvis Shape best journals Pelvis Shape top journals Pelvis Shape free medical journals Pelvis Shape famous journals Pelvis Shape Google Scholar indexed journals degenerative spinal stenosis articles degenerative spinal stenosis Research articles degenerative spinal stenosis review articles degenerative spinal stenosis PubMed articles degenerative spinal stenosis PubMed Central articles degenerative spinal stenosis 2023 articles degenerative spinal stenosis 2024 articles degenerative spinal stenosis Scopus articles degenerative spinal stenosis impact factor journals degenerative spinal stenosis Scopus journals degenerative spinal stenosis PubMed journals degenerative spinal stenosis medical journals degenerative spinal stenosis free journals degenerative spinal stenosis best journals degenerative spinal stenosis top journals degenerative spinal stenosis free medical journals degenerative spinal stenosis famous journals degenerative spinal stenosis Google Scholar indexed journals degenerative spondylolisthesis articles degenerative spondylolisthesis Research articles degenerative spondylolisthesis review articles degenerative spondylolisthesis PubMed articles degenerative spondylolisthesis PubMed Central articles degenerative spondylolisthesis 2023 articles degenerative spondylolisthesis 2024 articles degenerative spondylolisthesis Scopus articles degenerative spondylolisthesis impact factor journals degenerative spondylolisthesis Scopus journals degenerative spondylolisthesis PubMed journals degenerative spondylolisthesis medical journals degenerative spondylolisthesis free journals degenerative spondylolisthesis best journals degenerative spondylolisthesis top journals degenerative spondylolisthesis free medical journals degenerative spondylolisthesis famous journals degenerative spondylolisthesis Google Scholar indexed journals
Article Details
Abbreviations
DSS: degenerative spinal stenosis
DS: degenerative spondylolisthesis
PI: pelvic incidence
SS: sacral slope
PT: pelvic tilt
LL: lumbar lordosis
SLL: segmental lumbar lordosis
TK: thoracic kyphosis
HAC7P: plumbline of C7
1. Introduction
Degenerative spondylolisthesis (DSL) and degenerative spinal stenosis (DSS) represent two different clinical entities with similar symptoms and clinical signs, but with peculiar demographic characteristics and radiographic findings [1]. The degenerative process which leads to lumbar stenosis is initiated by disc dehydration and bulging causing the narrow of the space and this one leads to an increased transfer of stress to the facet joints. This fact accelerates facet joint cartilage degeneration and osteophyte formation. The combination of degenerative changes in the disc and facet joints can lead to central canal or lateral recess stenosis [2]. Degenerative spondylolisthesis occurs mostly at L4/L5 in adults older than 40 years and it is defined as slipping of a lumbar vertebra with an intact neural arch (3). In pathogenesis and its development, several predisposing factors have been advocated. Some of them are sagittal orientation and osteoarthritis of the facet joints, hormone factors, ligament hyperlaxity, insufficiency of paravertebral muscles, increased body mass index and female sexual hormones [4-6]. On assessing pathological mechanism and treating degenerative disease of the spine, the spinal sagittal alignment is an important tool. Many studies have, primarily in the normal population, investigated sagittal balance, and it is well established that the shape and the spatial orientation of the pelvis determine the organization of the thoracolumbar spine. Pelvic shape is determined by a fundamental parameter, the pelvic incidence (PI) whereas pelvis spatial orientation is defined by two positional parameters, the sacral slope (SS) and he pelvic tilt (PT). However, few studies are referred to the impact of the spinopelvic sagittal alignment, especially the influence of the pelvic shape, as a factor that would be related to degenerative spondylolisthesis [7]. In 2005, Rousouly et al. classified four types of spinopelvic sagittal alignment [8]. In this classification type IV is characterized by a high pelvic incidence and sacral slope, associated with an important lumbar lordosis. In this type, S1 endplate orientation is relatively vertical, which could represent a predisposing factor for slippage of lumbar vertebrae. The purpose of this retrospective study was to analyze the sagittal spinopelvic alignment and to compare these parameters between patients with and without degenerative spondylolisthesis who were surgically treated for lumbar spinal stenosis.
2. Materials and Methods
A total of 68 patients with lumbar spinal canal stenosis, 34 patients with degenerative spondylolisthesis (group 1) and 34 patients without degenerative spondylolisthesis (group 2), were surgically treated for spinal stenosis between 200 and 2018. Group 1 consisted of 10 men and 24 women, and group 2 Consisted of 11 men and 23 women. The mean age was 64.5 years (range, 42-79) in group 1 and 67.3 (range, 43-82 years) in group 2, respectively. In every patient of group 1 the involved level was the L4/L5. According to Meyerding’s classification the slippage grade was evaluated [9] and was determined to be 67.6% grade I and 32.3% grade II. In group 2, the involved level was L3/L4 in 3 patients, L4/L5 in 14 patients, L5/S1 in 7 patients, L3/L4/L5 in 6 patients and L4/L5/S1 in 4 patients. All patients of both groups have sustained a surgical treatment after failure of conservative management for at least six months (Figure 1). From the study, the exclusion criteria were: previous spinal surgery, spinal disease (trauma or tumor), idiopatic or degenerative scoliosis, developmental spondylolishesis and coxofemoral pathology. Both group were comparable in terms of gender and age.
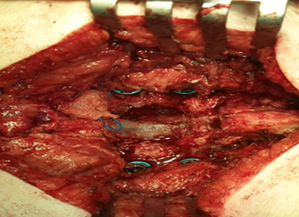
Figure 1: A intraoperative foto a patient with degenerative lumbar spondylolisthesis who underwent to wide decompression plus fusion.
2.1 Spinopelvic parameters
Spinopelvic parameters were measured on preoperative lateral lumbar x-rays using a standardized procedure. Each patient in the same standing position with the hands placed on supports and the hips and knees held in extension. With this protocol the thoracic and the lumbar spine, the sacrum and both femoral heads were visible for evaluation. The following radiographic parameters were measured by a single author: pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), thoracic kyphosis (TK) between the superior endplate of T1 to the inferior endplate of T12, lumbar lordosis (LL) between the inferior endplate of T12 and the superior endplate of S1 using the Cobb’s method, segmental lordosis from L1/L2 to L4/L5 between the superior endplate of the upper vertebrae and the inferior endplate of the lower vertebrae, segmental lordosis of L5/S1 between the superior endplate of L5 and S1, L4 slope and L5 slope. The spinopelvic parameters were measured as reported by Duval et al [10]. To evaluate global balance, the horizontal distance between hip axis (HA) and the C7 plumbline (HAC7PL) was also measured (Figure 2). The PI was defined as the angle between the perpendicular to the sacral plate and the line connecting the midpoint of the sacral plate to the bicoxofemoral axis (Figure 3). The PI is a constant morphological parameter, independent of the spatial orientation of the pelvis. Its value depends on the position of the sacroiliac joints in relation with the shape of the sacrum and the coxofemoral joints. The SS corresponds to the angle between the sacral plate and the horizontal plane (Figure 3). It is a positional parameter that varies according to the position of the pelvis. The PT corresponds to the angle between the vertical plane and the line connecting the midpoint of the sacral plate to the bicoxofemoral axis (Figure 3). Such as SS, the PT is a positional parameter. When the PT is increased the pelvis rotates backward around the coxofemoral joints. The PI represents the algebraic sum of the SS and the PT: PI = SS + PT.

Figure 2: A preoperative lateral lumbar x-ray of a female patient with degenerative spondylolisthesis. The patient is standing with the hand placed on clavicles and the hips and knees held in extension. With this protocol the thoracic and the lumbar spine, the sacrum and both femoral heads were visible for evaluation.

Figure 3: The spinopelvic parameters can by measured on pre-operative lateral view of lumbar spine as reported by Duval et al.
2.2 Statistical analysis
All data were expressed as the mean ± standard deviation. Overall differences of sagittal spinopelvic parameters between the two groups were statistically analyzed. Student’s t-test was used to compare each parameter between the group 1 and group 2. Furthermore, Pearson correlation coefficient was used to determine correlations among the spinopelvic parameters and between PI and % slip. To minimize individual variations, spinopelvic parameters/PI ratios were assessed and compared between the two groups. Statistical p-values less than 0.05 were considered statistically significant.
3. Results
There were significant differences in PI, SS, SLL between the two groups. The PI of group 1 (patients with degenerative spondylolisthesis) (56.9 ± 10.5°) was significantly greater than that of group 2 (patients without degenerative spondylolisthesis (49.1 ± 9.3°). The SS of group 1 (33.8 ± 9.5°) were also significantly greater than the one of group 2 (27.8 ± 6.3°). There was no significant difference in PT (23.1 ± 5° vs. 21.9 ± 4.2°) and HAC7PL (15.1 ± 31 mm vs. 15.1 ± 29.5°) (Figure 4). There were significant differences in segmental lordosis L4/S1 between the two groups. The segmental lordosis of group 1 (19.5°) was significantly slower than the one of group 2 (24.8°) However, the segmental lordosis was significantly higher in patients with spondylolisthesis at the levels L1/L2 (4.5o vs 3o) and L2/L3 (10o vs 6.9o) (Table 2). The L4/S1 segment is a hypermobile segment, the most common segmental instability, especially degenerative spondylolisthesis and/or stenosis lesion in DS and degenerative spinal stenosis pathology, and comprises most of the lumbar lordosis in the lumbar spine. In analysis of parameter/PI ratios, the SLL/PI ratio of group 1 (0.43 ± 0.5) was significantly lower than that of group 2 (0.61 ± 0.5). The spinopelvic parameters stratified according to gender were also compared between the two groups. In group 1, L4 slope, L5 slope, TK and LL were also significantly greater than those in group 2, both in males and females (fig 5). The mean L4 slope was 8.3o and the mean L5 slope was 17.5o, in patients with spondylolisthesis. The mean L4 slope was 3.3o and the mean L5 slope was 9.9o in the patients without spondylolisthesis. L5 slope was significantly larger than L4 slope in both groups. Degrees of correlations among the spinopelvic parameters differed between the two groups. In the group with degenerative spondylolisthesis, PI was more strongly correlated with SS (p<0.001) and LL ( p<0.001) than with PT (p<0.01). In contrast, in the group without degenerative spondylolisthesis, PI was more strongly correlated with PT (p<0.001) than with SS (p<0.01).

Figure 4: In contrast with PI (56.9 ± 10.5° vs. 49.1 ± 9.3°)) and SS (33.8 ± 9.5° vs. 27.8 ± 6.3°) which were significantly increased in group of patients with DS, PT was almost the same in both groups (23.1 ± 5° vs. 21.9 ± 4.2°).
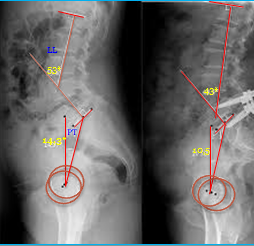
Figure 5: Pre- and post-operative radiographs of a patient with degenerative spondylolisthesis who underwent on posterior interbody fusion at level L4-L5. Postoperatively lumbar lordosis present a similar value to normal individuals.
4. Discussion
There are several factors that may be responsible in the development of degenerative spondylolisthesis, such as gender, ligamentous hyperlaxity, hormones, pregnancy, orientation of the lumber facet joints and configuration of the lamina [11-13]. The spine sagittal balance represents an important tool in the management of lumbar degenerative disorders [14]. However, relationship between the above factors and the sagittal imbalance had not yet been established. Roussouly et al. described four typical subtypes of sagittal orientation of the lumbar spine and pelvis. Type IV of this classification is characterized by a high pelvic incidence and sacral slope, associated with a relatively vertical S1 endplate in the sagittal plane and an important lumbar lordosis. Individuals with this type of sagittal orientation may be prone to an anterior displacement of above lumbar vertebrae. Legaye et al. [15] reported that a large PI indicated a steep SS and large sagittal curves. As reported by Barrey et al., patients with DS demonstrate a significantly greater PI (60o) than the normal population (52o) and they also suggested that the shape of the pelvis was, for degenerative spondylolisthesis, the major predisposing factor. Schuller et al. [16] also reported a significant increase in PI (66.o vs. 54.2o) and SS (42.3o vs. 33.4o) in the DS group than in the control group (individuals with low back pain due to moderate degenerative disc disease). According to these authors, the anatomic orientation of the pelvis with a high PI and SS represent a predisposing factor for DS. In the present study, we demonstrated that PI (56.9 ± 10.5° vs. 49.1 ± 9.3°) and SS (33.8 ± 9.5° vs. 27.8 ± 6.3°) in patients with degenerative spondylolisthesis were significantly larger than without degenerative spondylolisthesis. Our analysis of the spinopelvic sagittal alignment, stratified according to gender in the present sex-matched study, demonstrated that PI in patients with DS were significantly greater than those without DS. Therefore, large PI in association with abrupt SS might be in both genders a common predisposing factor for DS. In the series of Funao et al., the global sagittal balance was well-maintained such in patients with DS as in those without DS, and there was no significant difference in PT (23° vs. 22°) between them. In the present study, global sagittal balance was maintained in both groups and between them there was no significant difference in PT. However, in patients with degenerative spondylolisthesis, the average value of pelvic tilt was resulted superior of normal range. In the general population, the correlation between PI and LL was defined by Vaz et al. [17]. A high PI is usually related to a high lumbar lordosis and viceversa. Furthermore, lumbar lordosis is linearly increased with sacral slope. In this study, the initial comparison of parameters between the two groups demonstrated that the LL of patients with DS was larger than the one of patients without DS (42.5ο vs 38.8o), but when we took in consideration the LL/PI ratio, we saw that in the DS group it was smaller than the one of the non-DS group (0.746 vs 0.790). That means that the lumbar lordosis in patients with degenerative spondylolysthesis is larger than the one in patients with degenerative spinal stenosis, because of the fact that in the first group of patients the PI is larger. However, lumbar lordosis of the DS group considering the PI value is actually smaller than the one of the non-DS group. A great lumbar lordosis in patients with DS, represents a well-known factor of excessive mechanical stresses on posterior articular joints, thus accelerating arthrosis changes. In addition, the segmental lordosis of L4/S1 of group 1 (19.5°) was significantly smaller than the one of group 2 (24.8°). In patients with spondylolisthesis, the loss of segmental lordosis of L4/S1 is larger than the one in patients without spondylolisthesis, and it is caused such by the anterior slippage as the degenerative disc space narrowing. On the other hand, when analyzing the segmental lordosis of the cranial levels, it became evident that the segmental lordosis of L1/L2 and L2/L3 was significantly increased in patients with spondylolisthesis compared to patients without spondylolisthesis (respectively, 10o vs 6.9o and 4.5o vs 3o). This is due to the hyperextention of the levels above the spondylolisthesis. Furthemore, as suggested by Beckers and Bekaert, the hyperlordosis of cranial lumbar segments increases posterior stress on L4/L5 facet joints [18]. Our results demonstrate that the segmental hyperlordosis above L4/L5 may be resulted as a possible compensation mechanism of lower lordosis decrease and of posterior tilt of the pelvis. As a result, it seems that sagittal imbalance in patients with degenerative spondylolisthesis is caused such by the loss of lumbar lordosis, as by the loss of segmental lordosis of caudal levels and finally by the pelvic retroversion which acts as a compensatory mechanism. Actually, the slippage and the loss of lordosis lead to a sagittal anterior imbalance as demonstrated by anterior translation of the C7 plumbline [19]. In the DS patients, it is suggested that the limit of anterior displacement of the axis of gravity is succeeded by the pelvis retroversion which corresponds to rotation of the pelvis around the coxofemoral joints. This mechanism is secondary to the action of hip extensor muscles [20]. Our results are in concordance with these affirmations. We actually noticed that the degree of correlations among the spinopelvic parameters differed between the DS and non-DS groups: in patients with DS, there was a strong correlation between the pelvic incidence and the sacral slope rather than with the pelvic tilt. Consequently, we may conclude that the sacral slope’s increase is the main compensating factor to the presence of a greater pelvic incidence. In contrast we noticed that, in patients without DS, there was a strong correlation between the pelvic incidence and the pelvic tilt rather than with the sacral slope. Consequently, we may deduce that the retroversion of the pelvis turns to be the main compensating factor for a greater pelvic incidence. Actually, the sagittal imbalance of patients with degenerative lumbar stenosis but without slippage is caused by overall loss of lumbar lordosis and significant pelvic retroversion operated as a compensation mechanism [21].
5. Conclusions
Patients with degenerative spondylolisthesis have a greater pelvic incidence, lower segmental lumbar lordosis/PI ratio and relatively high propensity for sagittal imbalance compared with degenerative spinal stenosis patients. That means that a high PI may be a predisposing factor to the development of DS. Furthermore, there is a positive correlation between the pelvic incidence and the percentage of the slippage. Patients with degenerative spondylolisthesis have a significant loss of segmental lordosis of the caudal lumbar spine, which is partially compensated by hyperextension in the upper lumbar spine and pelvis back tilt. The degree of the correlation among the spinopelvic parameters differ between patients with DS and patients without DS. In the first ones, there is a strong correlation between the PI and the SS, rather than with the PT.
Acknowledgements
None declared
Conflict of Interest
Authors declare no conflict of interest or any funding source received for this study.
References
- Arnoldi CC, Brodsky AE, Cauchoix J, et al. Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clin Orthop Relat Res 115 (1976): 4-5,
- Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 20 (1995): 1307-1314.
- Pedram M, Dupuy R, Vital JM. Spondylolisthesis lombaire degeneratif. Encyclopedie Medico-Chirurgicale. Elsevier, Paris, Chapter 15-835-B-10 (2003).
- Fujiwara A, Tamai K, An HS, et al. Orientation and osteoarthritis of the lumbar facet joint. Clin Orthop Relat Res 385 (2001): 88-94.
- Grobler LJ, Robertson PA, Novotny JE, et al. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine 18 (1993): 80-91.
- Jacobsen S, Sonne-Holm S, Rovsing H, et al. Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine 32 (2007): 120-125.
- Morel E, Vialle R, Rillardon L, et al. Analysis of Sagittal Balance in Degenerative Spondylolisthesis. Paris, Sauramps Medical Eds (2004): 107-118.
- Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30 (2005): 346-353.
- Mac-Thiong J-M, Wang Z, Guise JA, et al. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine 33 (2008): 2316-2325.
- Funao H, Tsuji T, Hosogane N, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J 21 (2012): 2181-2187.
- Matsunaga S, Sakou T, Morizono Y, et al. Natural history of degenerative spondylolisthesis: pathogenesis and natural course of the slippage. Spine 15 (1990): 1204-1210.
- Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Intern Orthop (SICOT) 25 (2001): 40-42.
- Sato K, Wakamatsu E, Yoshizumi A, et al. The configuration of the laminas and facet joints in degenerative spondylolisthesis. Spine 14 (1989): 1265-1271.
- Barrey C, Jund J, Noseda O, et al. Sagittal balance of the pelvis–spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16 (2007): 1469-1470.
- Legaye J, Duval-Beaupe`re G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7 (1998): 99-103.
- Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J 20 (2011): 713-719.
- Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11 (2002): 80-87.
- Beckers L, Bekaert J. The role of lordosis. Acta Orthop Belg 57 (1991): 198-202.
- Roussouly P, Gollogly S, Noseda O, et al. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: Aradiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31 (2006): E320-E325.
- Vital JM, Gille O, Gangnet N. Sagittal balance and implication on clinical practice [in French]. Rev Rhum 71 (2004): 120-128
- Jae Kwan Lim, Sung Min Kim. Comparison of Sagittal Spinopelvic Alignment between Lumbar Degenerative Spondylolisthesis and Degenerative Spinal Stenosis. J Korean Neurosurg Soc 55 (2014): 331-336.
