Diarrhoeal Disease in Relation to Childhood Malnutrition and Its Impact on Socio-economic Condition in Emerging Countries Like Bangladesh
Article Information
Reema Afroza Alia1*, Nayeema Sadia2, Nazma Parvin Shammy2, Ferdous Ara Tithy3, Rumana Shelim4, Rukhsana Parvin5
1Associate Professor, Department of Pediatrics, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
2Assistant Professor, Department of Pediatrics, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
3Registrar, Department of Pediatrics, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
4Associate Professor, Department of Pediatrics, East-West Medical College & Hospital, Dhaka, Bangladesh
5Assistant Professor, Department of Pediatrics, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh
*Corresponding Author: Dr. Reema Afroza Alia, Associate Professor, Department of Pediatrics, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
Received: 30 June 2022; Accepted: 14 July 2022; Published: 08 September 2022
Citation: Reema Afroza Alia, Nayeema Sadia, Nazma Parvin Shammy, Ferdous Ara Tithy, Rumana Shelim, Rukhsana Parvin. Diarrhoeal Disease in Relation to Childhood Malnutrition and Its Impact on Socioeconomic Condition in Emerging Countries Like Bangladesh. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 370-379.
Share at FacebookAbstract
Despite a drop in the previous three decades, diarrhoeal illness remains a significant worldwide cause of young fatalities. Childhood rotavirus, diarrhoea, climatic variables, and malnutrition all have a significant link. Conversely, in the recent decade, a major nutritional transition (reduced undernutrition) was reported in under 5 children, particularly in developing countries such as Bangladesh, with a concurrent increasing trend of rotavirus infection. Given the pathophysiology of rotavirus, there might be a connection between this dietary change, climate, and other man-made variables in metropolitan places like Dhaka, Bangladesh, in increasing rotavirus infection. Despite great socioeconomic development and a decade of measures targeted at alleviating it, malnutrition among children under the age of five remains a serious issue in Bangladesh. Despite the fact that various studies have been undertaken to determine the key risk factors for malnutrition, none of them have examined the significance of low birth weight (LBW) 36%. In recent decades, Bangladesh has seen a significant decrease in the number of children dying from diarrhoea. Despite being a resource-constrained, highly populated nation, Bangladesh has been able to accomplish a considerable decrease in pediatric diarrhoea mortality over the last few decades. Improving hand hygiene habits, increasing zinc coverage for diarrhoea therapy, and sustaining nutritional improvement are some of the challenges that remain to further reduce the burden of disease and death caused by diarrhoea. Continuous engagement with NGOs and the commercial sector, as well as the adoption of pluralistic health system platforms for preventive and curative service delivery, are essential to extend intervention coverage and speed the end of children's diarrhoeal deaths in Bangladesh.
Keywords
Bangladesh, Diarrhoea, Malnutrition, Policies and Programs, Health Medicine
Article Details
1. Introduction
The diarrhoeal disease remains a leading global cause of childhood deaths despite a decline in the last three decades [1]. Since the 1980s, global estimates of diarrhea-related mortality have shown a continuous drop. Despite all breakthroughs in health technology, better treatment, and greater use of oral rehydration therapy in recent decades, diarrhoeal illnesses remain a major source of morbidity and death globally. In contrast to mortality trends, diarrhea-related morbidity has not decreased, and worldwide estimates remain between two and three bouts of diarrhoea per under five-year-old kid each year [2, 3]. There are a number of factors contributing to the poor diminishing trend of diarrhoeal illnesses, particularly in developing nations, with environmental sanitation difficulties playing a prominent role. According to a recent study, some interventional measures for environmental sanitation in India should be prioritized [4]. This is due to the shifting pattern of exposure to risk factors for water-borne illnesses at different levels, such as urbanization and industry. As a result of the aforesaid results, it is critical to examine the diarrhoeal disease morbidity pattern and variables associated with it, as well as preventative and control techniques, as well as current advances, in order to implement suitable control measures at different levels in the community. The worldwide burden of diarrhoea mortality is borne mostly by developing nations, with the majority of fatalities occurring in Sub-Saharan Africa and South Asia [5, 6].
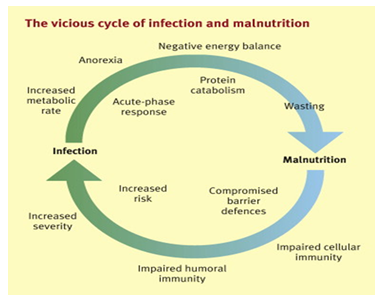
Among impoverished Bangladesh, diarrhoea in children is still a severe problem. There is a significant link between diarrhoea in children and a variety of environmental variables. For example, both high and low rainfall has been linked to an increase in diarrhoea cases caused by Vibrio cholera, whereas rising temperatures and both high and low rainfall have been linked to an increase in non-cholera cases [7]. These might be linked to rising river levels, resulting in floods that affect the most vulnerable individuals in low-income communities with sub-optimal water-satiation practices. In the Dhaka megacity, flooding is also linked to fast land covering (land loss, habitat destruction, and loss of natural plant cover). Furthermore, overpopulation, inadequate sewage systems, and waste disposal, along with water stagnation, rising surface temperatures, and pollution, allow other illnesses such as typhoid and dengue fever in Dhaka and simultaneously encourage other diseases like as typhoid and dengue fever [8, 9]. Childhood malnutrition has been linked to an increased incidence of infectious diarrhoea, according to epidemiological research [10]. Rotavirus is one of the most common causes of infantile diarrhea, and cellular attachment to healthy cells in the brush border of the intestine is critical in the pathophysiology of rotavirus infection.
As a consequence, well-nourished children are disproportionately affected by rotavirus infection as compared to undernourished children. Climate change has an impact on ecosystems and may forecast the onset and re-emergence of certain illnesses. Data from the Dhaka Hospital's long-running diarrhoeal disease surveillance system (DDSS) at the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) found a link between rotavirus diarrhoea and high temperatures, low humidity, and high river levels, as well as seasonal variability. Despite considerable improvements in water and sanitation policies in the capital city and its surrounding catchment regions, the facility has suffered a prolonged growing trend of rotavirus infection over the previous two decades. Bangladesh's childhood malnutrition profile has evolved over time, similar to that of other nations, with a recent decline in undernutrition and a rise in overnutrition [11, 12]. The review article attempted to demonstrate the value of identifying the critical inputs necessary to resuscitate worldwide efforts to prevent and manage childhood diarrhoea. This study is particularly notable since Bangladesh is suffering from the repercussions of its success, with a high degree of complacency about diarrhoea and the idea that the problem has been resolved.
2. Causes of Diarrhoeal Disease
Diarrhea is the second biggest cause of mortality among children under the age of five. Every year, almost 500,000 children under the age of five die from diarrhoea. Every year, almost 1.7 billion people throughout the world suffer from diarrhoea. Diarrhoea kills more children per day than AIDS, malaria, and measles combined. In 2013, diarrheal illnesses killed an estimated 1.3 million people, including 45,000 babies. About 40% of diarrhoea hospitalizations in children under the age of five are caused by the rotavirus. Every year, around 215,000 children under the age of five die as a result of rotavirus. Campylobacter, E. coli, non-typhoidal Salmonella, and Shigella are some of the most frequent bacteria that cause diarrhoea. Cryptosporidium, Entamoebahistolytica, and Giardia lamblia are all common parasite causes of diarrhoeal illness. In children under the age of five, malnutrition is one of the leading causes of illness and death [1, 2]. It harms children's growth and development in both the short and long term [11, 12]. Malnourished children, for example, are less productive physically, emotionally, and cognitively than healthy children, and they are more likely to develop chronic diseases and impairments [13-15]. Diarrhoeal illness, after pneumonia, was the second largest cause of mortality among children under the age of five in low-income countries in 2004, killing 1.5 million children per year. Children under the age of three in underdeveloped nations had three bouts of diarrhoea each year on average. According to an analysis of 33 research in affluent nations, the incidence and prevalence of acute gastrointestinal sickness ranged from 0.1 to 3.5 episodes per person-year. According to research in Bangladesh, Vibrio cholerae O1 (23%) was the most common pathogen identified, followed by ETEC (14%) (11%). Infants accounted for around 8% of cholera infections, with the youngest children being one month old, whereas ETEC infections accounted for 11%. The enterotoxin type was almost evenly distributed among the isolated ETEC strains: ST accounted for 31%, LT/ST for 38%, and LT accounted for 31%. G. lamblia prevalence varied significantly between studies in South Asia, Southeast Asia, and the Far East, with higher levels in urban than rural areas, more in poor communities, slightly higher in males than females with children aged 2 to 5, and among university students, elderly people, HIV-positive patients, and gastric carcinoma patients. 30 In rural southern India, rates of Giardia infection in diarrhoea patients vary from 0.4% to 70%, with asymptomatic cyst passing reaching 50%. Between 1980 and 2015, Bangladesh's under-five mortality rate decreased significantly, from 198.9 per 1000 live births to 37.6 per 1000 live births. Diarrhea mortality rates among children under the age of five decreased from 15.1 to 6.0 per 1000 live births over the same time period [16]. The burden of diarrhoeal illnesses was also reduced in a similar way. According to the BDHS, the reported prevalence of diarrhoea in the previous two weeks among under-five children decreased from 12.6 percent to 5.7 percent (a 56 percent reduction) between 1993 and 2014, and the prevalence of diarrhoea with blood decreased from 2.8% to 1% (a 64% reduction) [13]. Persistent diarrhoea was reduced from 8% in 1991 to 1% in 2010 [17] according to hospital-based research. The absence of nationally representative surveillance data makes a reliable assessment of diarrhoea incidence in Bangladesh difficult, while we do have estimates from smaller specialized research groups at various time intervals.
3. Childhood Malnutrition
Malnutrition among children is a major worldwide health issue that continues to pose a serious danger to poverty reduction and long-term development. Malnutrition kills almost 3.1 million children yearly, accounting for 45 percent of fatalities among children under the age of five [1, 2]. Early infancy cognitive development is negatively impacted by malnutrition [3, 4]. It also causes school absenteeism and obstructs adult productivity and wages [18, 19]. Malnourished moms give birth to babies who struggle to grow and thrive, and the repercussions of malnutrition may be passed down the generations. Malnutrition is most common in South Asian nations, especially India, Pakistan, and Bangladesh, according to regional estimates from 2014 [1]. Although Bangladesh has achieved substantial progress in attaining most of the Millennium Development Goals during the previous decade [20]. improvements in child nutrition have been quite gradual [21]. Despite more than a decade of measures targeted at lowering Bangladesh's malnutrition rate, it remains unacceptably high when compared to the developed world [21]. According to the results of a recent national health survey [16, 17]. The prevalence of stunting (low height for age) decreased from 51% in 2004 to 41% in 2011, while the prevalence of underweight (low weight for age) decreased from 43% in 2004 to 36% in 2011. During the same time span, the prevalence of wasting (low weight for height) remained stable at roughly 16 percent, much above the WHO emergency threshold of 15%. These findings indicate that additional measures are needed to enhance the nutritional health of Bangladesh's children under the age of five. Malnutrition among children under the age of five is now one of the government's and many foreign organizations' top priorities in Bangladesh. As a result, identifying the causes linked to malnutrition in children under the age of five is critical so that stakeholders may develop evidence-based policies to promote nutrition. One of the key issues for public health experts has been identifying these determinants and offering practical suggestions for improving nutrition [3]. Maternal illiteracy, low household economic status, food insecurity, lack of exclusive breastfeeding, administration of pre-lacteals, and colostrum deprivation have all been identified as potential factors linked to child malnutrition in studies conducted around the world in the last two decades [22-26]. Low maternal education, poor socioeconomic position, and short prior birth intervals have all been recognized as substantial risk factors in research undertaken in developing countries such as Bangladesh [22-25]. Over the past decade, Bangladesh has made significant progress on each of these fronts [16] but progress toward lowering the incidence of child malnutrition has been disappointingly modest [21].
4. Impact on Socio-economic Condition Due to Childhood Malnutrition
Child malnutrition in Bangladesh and socioeconomic disparities and if they vary by subnational area. Stunting and underweight were found to be more common among Bangladeshi children born to lower-income families and mothers with less education. A recent study discovered large income and education-related disparities in child malnutrition in the north-eastern (e.g., Sylhet) and southern and eastern (e.g., Barisal and Chittagong). In addition, the protective impact of a mother's education and family affluence differed throughout Bangladesh's regions. A study showed that stunting and being underweight were found to be more prevalent in the southern and eastern areas, such as Barisal, Chittagong, and Sylhet. Similar geographical trends in the frequency of stunting and underweight were also discovered in previous investigations in Bangladesh. Prior research has shown that Bangladesh's eastern and south-eastern areas had the greatest rates of severe child wasting and stunting, with wasting levels above the WHO critical threshold level. The most robust drivers of child malnutrition outcomes seemed to be parental education and family wealth. According to the research, children born to parents with greater levels of education and money had the best nutritional outcomes. Despite the fact that parental SES measures are protective variables for child health in Bangladesh and other poor countries [8, 17], have a significant variation in the impact of these protective factors across Bangladesh's regions. For example, the adjusted models' prediction probabilities showed that family wealth and a mother's education are both inversely linked with outcomes throughout the areas. Poverty is a key predictor of child underweight, as is socioeconomic level. Children from low-income households are more likely to be underweight than children from higher-income families [4]. Despite the fact that Bangladesh has had great economic development and substantial advances in educational accomplishment over the previous 20 years, a considerable section of the population, roughly 43.3%, continues to live below the poverty line of $1.25 per day [27]. The job of lowering the country's incidence of underweight children is particularly challenging since such a big percentage of the population lives in poverty, unable to purchase healthy food or access better health care facilities. Indeed, a number of studies in Bangladesh found that household socioeconomic position was a key driver of children underweight, with children from better socioeconomic backgrounds having a decreased risk of being underweight [27]. Children from the greatest wealth index had 44% lower risks of being underweight than children from the worst wealth index, according to research conducted in Bangladesh by Alom et al. [27]. Most research done in Bangladesh indicated that mothers' literacy level, latrine choice, and low family income are linked risk factors for underweight in children under the age of five [28-30]. Improper feeding practices, maternal antenatal and postnatal care, diarrhea in children within the previous two weeks [31] living in a rural area [30]. Mothers with fewer media exposure, children of mothers working outside the home [32], unimproved toilet facilities, and living in the Sylhet division [7] are among the other risk factors estimated to be significantly associated with the risk of child underweight. Several studies in Bangladesh found that the likelihood of being underweight among children under the age of five increases as the child's age increases. The reasons of underweight are complex and interconnected, and they vary by region, emphasizing the need for local research investigations. There is considerable evidence that the incidence of childhood sickness is related to the age of the child, especially in the majority of poor countries [8]. Children in higher wealth index homes had a reduced risk of being underweight, which was backed up by another study that stated that children in lower wealth index households had a higher risk of being underweight [16, 17, 26]. It's possible that children in higher wealth index homes were more likely to come from food-secure families, have dads and moms who were more educated, and live in better neighborhoods with better health facilities. It is widely known that maternal knowledge of child health has a profound impact on child well nourishment, and a study performed in Bangladesh documented those mothers with better child health knowledge had mostly come from the richest household.
5. Public Sector Health Initiatives to Combat Diarrhea
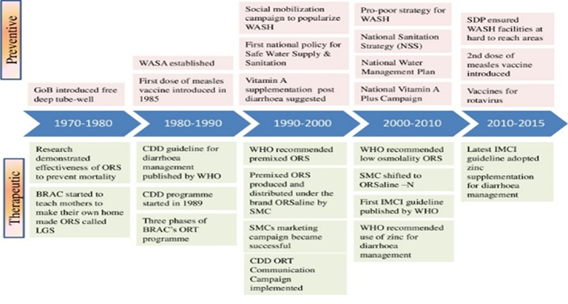
Bangladesh was one of the first countries to implement programs focused on reducing diarrhea-related fatalities among children. It all started in 1970, when Bangladesh was still a part of Pakistan, with the introduction of a Communicable Disease Control program to track diarrhoea outbreaks throughout the nation. Prevention and management of diarrhoeal illnesses became a main primary health care objective in the health sector with the Alma-Ata declaration in 1978 [32]. WHO launched the Control of Diarrhoeal Disease (CDD) Programme [7] in response to the worldwide burden of diarrhoeal illnesses, which was subsequently accepted by Bangladesh in. 1989 [33]. The Integrated Care of Pediatric Diseases (IMCI) approach was created by WHO and UNICEF in the late 1990s to combine the management of common childhood illnesses such as diarrhoea, pneumonia, malaria, measles, and malnutrition. The Government of Bangladesh made a significant step in reducing under-five mortality when it adopted IMCI as an integrated approach under the "Health and Population Sector Programme (1997-2002) (HPSP)" - the first Sector Wide Approach (SWAp) All of the vertical programs dealing with common childhood ailments were combined into a single management guideline. Large governmental and private sector expenditures on community health workers, particularly following the Alma Ata Declaration in 1978, aided the quick adoption of community-based interventions such as ORS for diarrhoea, family planning, and immunization [34].
6. Recent Developments in Combating Diarreheoa
In 62 nations, the rotavirus vaccine has been approved for use, with 11 countries including it in their national vaccination schedule. Infant rotavirus vaccine should be included in all national immunization regimens, according to the Strategic Advisory Group of Experts (SAGE). Following reconstitution as a 1ml oral dosage, the vaccine should be given as soon as possible. A total of two doses of the vaccination are recommended. At the age of 6 weeks, the first dosage should be given, and no later than 12 weeks. At least four weeks should elapse between dosages one and two [30]. All of the studies found that rotavirus vaccination is cost-effective, but that it is now out of reach for poor countries. In order to establish rotavirus immunization, developing nations would undoubtedly need financial assistance from international organizations. Because bacteria were extremely resistant to different antimicrobial drugs, including co-trimoxazole and erythromycin, which are now indicated for empiric therapy of diarrhoea, constant antibiotic monitoring is required [9]. New strategies for diarrhoea prevention, management, and treatment, such as enhanced oral rehydration formulations, zinc supplements, and rotavirus vaccinations, have re-energized attempts to minimize diarrhoea mortality throughout the globe [33]. The addition of zinc and prebiotics to ORS reduces the length of diarrhoea in children. 51 With preventative zinc supplementation, the incidence of diarrhoea was reduced by 13%. In community settings in poor nations, preventive vitamin A supplementation lowers all-cause and diarrhea-specific mortality in children aged 6 to 59 months. In Finnish tourists visiting Morocco, it was discovered that the oral killed WC/rBS cholera vaccine (DukoralTM) prevented 23% of all diarrhoea bouts and 52% of ETEC events. However, it was said that this protection only lasted a few months. In two bigger placebo-controlled Phase III studies in American travelers to Mexico and Guatemala, the protective effect of the rCTB-CF ETEC vaccination was examined. In rural Egypt, 350 children aged 6 to 18 months participated in the sole pediatric research to examine the effectiveness of the rCTB-CF ETEC vaccination. A novel delivery technique, the transcutaneous immunization patch, is being used to generate particular ETEC vaccinations [35].
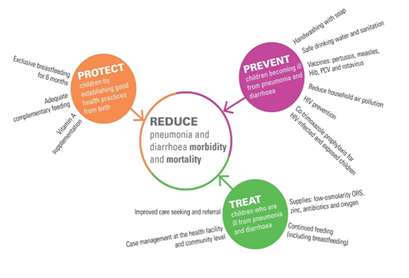
7. Protective Actions Provide the Groundwork for Keeping Kids Healthy and Disease-Free
7.1 Exclusive breastfeeding (no extra meals or drinks, including water)
It protects newborns from illness and ensures a food supply that is safe, clean, accessible, and properly matched to their requirements during the first six months of life. In poor and middle-income countries, increasing breastfeeding might prevent almost half of all diarrhoea bouts and one-third of all respiratory illnesses.
7.2 Continued breastfeeding and adequate supplemental feeding
Between the ages of 6 months and 2 years, proper supplemental feeding - giving children sufficient amounts of safe, nutritious, and age-appropriate meals while continuing to nurse - may help to prevent child mortality, especially those caused by pneumonia and diarrhoea.
7.3 Vitamin A Supplementation
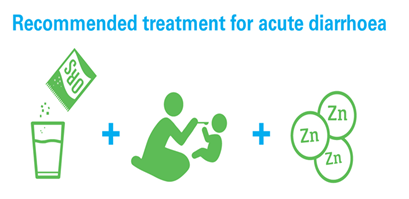
Taking a high-dose vitamin A supplement will help maintain a healthy immune system and decrease diarrhoea by 15%. In nations with high under-five mortality or where vitamin A insufficiency is a public health hazard, children aged 6 to 59 months should get two high-dose vitamin A supplements per year. Since 2004, UNICEF and the World Health Organization (WHO) have advocated restoring lost fluids with oral rehydration treatment to treat children’s diarrhoea. Oral rehydration salts (ORS) and zinc supplements, in addition to sustained meals, are suggested treatment options for diarrhea.
8. Policies and Programs in the Field of Medicine
Several investigations were carried out at the Cholera Research Laboratory (now the International Centre for Diarrhoeal Disease Research, Bangladesh; icddr,b) in Dhaka throughout the 1960s, and the ground-breaking ORS was developed. This medication has been shown to reduce the risk of diarrhoeal illness mortality in children [36]. The National Oral Rehydration Project [35] began broad distribution of ORS in 1981 via health institutions and during epidemics. However, in rural regions, scale-up attempts were constrained since there was no commercial manufacture of ORS packets, resulting in limited supply [37]. During the same time period, BRAC launched a government-approved countrywide campaign to promote awareness of diarrhoeal sickness and train caregivers on how to manufacture Lobon-Gur Solution, a simple homemade version of ORS [36, 38]. Despite its enormous success in raising awareness of rehydration, the Lobon-Gur Solution has prompted questions about its safety and dependability [37]. As a result, the emphasis turned to ORS packets, which SMC (Social Marketing Firm), Bangladesh's biggest non-profit private social marketing company, distributes under the brand name ORSaline. SMC moved to OR Saline-N and constructed a manufacturing factory for mass production and distribution throughout the country. Low osmolality is now produced by all public and private sector enterprises. Bangladesh has the highest rate of ORS usage for diarrhoea in the world [34] non-governmental organizations (NGOs) and the corporate sector, as well as public sector governance, all had a role in popularizing ORS. Prior to the Lobon-Gur Solution project, it was common practice in the community to limit a diarrhea-stricken child's food and hydration intake [38].
BRAC community health professionals delivered door-to-door services as part of the Lobon-Gur Solution program to improve awareness of diarrhoea prevention and treatment, as well as the need of obtaining medical help from a qualified practitioner. This massive public awareness campaign significantly shifted community norms away from limited eating and toward the adoption of homemade dehydration solutions. According to a 1993 evaluation, 70% of mothers could produce Lobon-Gur Solution and utilized oral rehydration treatment (ORT) (premix ORS or Lobon-Gur Solution) in more than 50 percent of diarrhoeal episodes among children under the age of five [38]. SMC marketed packaged ORS with a nationwide media campaign and provided universal availability through community outlets/shops. Nonetheless, the CDD program began a large-scale ORT communication campaign in 1996, using a number of communication channels to raise community understanding and awareness of essential homecare guidelines such as increased fluid, sustained eating, and proper care-seeking during diarrhea [33] OR Saline became a widespread home item and the "go-to" dehydration treatment The proportion of under-five children who received ORS for a diarrhoea episode grew from 50% in 1993 to 77% in 2014. The use of zinc supplements during diarrhoeal sickness was shown to lower the usage of antibiotics while having no effect on the use of ORS [16]. Based on these results, significant national and international development efforts have been focused on scaling up the use of zinc in combination with ORS for diarrhoea care. icddr,b began the Scaling Up Zinc for Young Children (SUZY) initiative in 2003 in conjunction with the Government of Bangladesh [31, 33].
9. Policy and Programs to Avoid Diarrhea
In the 1970s, the Bangladeshi government, with the help of UNICEF, installed around 10 million deep tube-well (hand pump) wells at no cost to enhance access to clean drinking water [27]. During the mid-nineties, better sanitation became a focus. Between 1990 and 2014, several donor-supported large-scale sanitation programs with a variety of intervention approaches were implemented by both public and NGO sector initiatives, including providing free or partially subsidized construction materials for improved sanitation facilities, promoting hygiene practices through behavior change communication (BCC), and creating an enabling environment by eliminating improper sanitation practices [24]. The first National Policy for Safe Water Supply and Sanitation (NPSWSS) was formed in 1998 to coordinate the Water, Sanitation, and Hygiene (WASH) initiatives, and the National Sanitation Strategy was developed in 2005 [25]. The private sector's engagement in the manufacturing of inexpensive consumer-oriented latrines and tube wells has accelerated the transition to clean drinking water and community-led complete sanitation. The National Sanitation Campaign 2003-06 was effective in obtaining 100% latrine coverage in around 10 districts in a short period of time by using a successful combination of top-down and bottom-up tactics [24]. By 2014, almost every home in the nation had access to clean drinking water, and access to not-shared sanitary latrines had increased by 45%. To treat vitamin A deficiency, Bangladesh began supplementing infants with vitamin A in 1973 as part of the Nutritional Blindness Programme [7]. Between 1973 and 1993, frontline workers distributed vitamin A capsules to children during home visits and other service delivery interactions, attaining a coverage rate of 49% among children under the age of three [11].
However, in 1995, vitamin A capsules were distributed in large quantities, both in conjunction with national vaccination days and separately during vitamin A weeks [39]. The GoB agreed in 2003 to hold the National Vitamin a Plus Campaign once a year; however, since 2004, the campaign has been held twice a year. Vitamin A supplementation coverage among children under the age of five peaked at 82% in 2004 and has subsequently fallen to 62% in 2014. The National Infant and Young Child Feeding IYCF strategy was developed in 2007 [17], and the 3rd Health Population Nutrition Sector Development Programme 2011-2016 prioritized growth monitoring and promotion, as well as counseling for infant and young child feeding, early initiation, and exclusive breastfeeding [28]. In addition to government initiatives, non-governmental organizations (NGOs) have played an important role in developing community knowledge of IYCF practices. Bangladesh's Integrated Nutrition Programme, which ran from 1995 to 2002, and its successor, the National Nutrition Programme, collaborated with NGOs to undertake direct nutrition interventions, including IY promotion [27]. Several NGOs, like BRAC, continued to promote IYCF practices by a significant number of their own community volunteers, despite the fact that the 3rd Sector Programme mainstreamed nutrition services delivery via the health system [35]. Although current data indicates a decline in 55 multi-sectoral initiatives to enhance infant feeding habits seems to have resulted in an increase in the prevalence of exclusive breastfeeding in the first six months of life from 46 percent in 1993 to 64 percent in 2011. 2014 BDHS.
10. Discussion
Bangladesh has led the way in reducing diarrhea-related fatalities among children under the age of five in poor and middle-income nations. The important elements that have contributed to the decrease in diarrhea-related mortality in children under the age of five are identified in our article. The most significant impacts came from improving nutritional status and attaining high coverage of ORS and zinc for diarrhoeal episode treatment, however, vitamin A and minor effects from most of the other interventions also had a role. This was made possible by reforms in the health system, such as the timely implementation of evidence-based policies and programs, successful engagement with the business sector, NGO and social marketing activities, and general socio-economic growth. Between 2000 and 2015, improvements in water and sanitation helped to reduce diarrhea-related mortality by around 10%. From 2000 to 2015, its influence was greater than from 1980 to 2000. Bangladesh's formulation and acceptance of a pro-poor water and sanitation strategy in 2005, as well as the widespread application of proven measures, may explain this. Between 1980 and 2015, access to better sanitation and soap-based hand washing increased from 41% to 61% and 3% to 17%, respectively. Improvements in hand hygiene habits, on the other hand, are still on Bangladesh's to-do list.
According to data from hospital-based research in Bangladesh, just 4% (4/103) of cholera patients and their family members had followed all important measures, including hand washing with soap [17]. The greatest motivation for developing hand cleanliness behaviors has been suggested as spreading hand hygiene messaging emphasizing nutritional advantages [26]. Undernutrition has been linked to enteric illnesses that cause severe or chronic diarrhoea and mortality [34]. Over the last two decades, Bangladesh has made tremendous progress in reducing childhood malnutrition; stunting among children under the age of five has decreased from 55% in 1996 to 36 percent in 2014. The decrease in stunting contributed the most to the reduction in diarrhoea mortality among children under the age of five between 1980 and 2015. Recent research suggests that preventing a child's development from halting might minimize the occurrence of diarrhoea and its related negative outcomes, such as mortality [21]. Pro-poor economic growth, improvements in agricultural production and diversification, prioritizing nutrition-sensitive interventions in policy, implementation of vertical programs improving community awareness of women's rights and empowerment issues, response to nutritional emergencies, and support from the NGO sector in nutrition service delivery are all factors in Bangladesh's progress in nutrition [27].
11. Conclusion
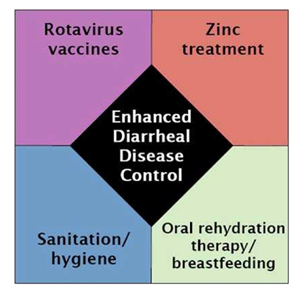
Owing to the high morbidity and death rates among children in underdeveloped countries due to diarrheal infections, reaching Millennium Development Goal 4 (MDG 4) would need extra effort. MDG 4 seeks to lower the worldwide under-five mortality rate by two-thirds between 1990 and 2015. Governments should prioritize a comprehensive diarrhoeal disease control strategy that includes improved water quality, hygiene, and sanitation, as well as the provision of oral rehydration solution and zinc supplements, as well as improved case management and research in the field of cost-effective interventions. Existing public health initiatives should devise cost-effective methods for encouraging people to wash their hands that can reach millions of people who are at risk. For the management of pediatric diarrhoeal illnesses in underdeveloped countries, strong political will, suitable financial allocation, monitoring, and follow-up assessment are required. Because of Bangladesh's evident success in reducing diarrhoeal sickness, diarrhoea has become a forgotten concern, with the popular notion that it is no longer a priority. To continue the momentum of saving lives from preventable and treatable diseases like diarrhoea, intervention packages that optimize coverage of direct diarrhoeal interventions and promote nutrition and WASH initiatives are essential. Some of the obstacles that remain to further decreasing the burden of sickness and mortality from diarrhoea include improving hand hygiene practices, boosting zinc coverage for diarrhoea treatment, and maintaining nutritional improvement. To expand coverage of interventions and accelerate the end of children’s diarrhoeal fatalities in Bangladesh, ongoing collaboration with NGOs and the commercial sector is required, as well as the use of pluralistic health system platforms for preventative and curative service delivery.
References
- Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000– 15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388 (2016): 3027- 3035.
- Ahmed NU, Zeitlin MF, Beiser AS, et al. Assessment of the impact of a hygiene intervention on environmental sanitation, childhood diarrhoea, and the growth of children in rural Bangladesh. Food Nutr Bull 15 (1994): 1-14.
- Baqui AH, Black RE, El Arifeen S, et al. Effect of zinc supplementation started during diarrhoea on morbidity and mortality in Bangladeshi children: community randomized trial. BMJ 325 (2002): 1059.
- Chowdhury MK, Gupta V, Bairagi R, et al. Does malnutrition predispose to diarrhoea during childhood? Evidence from a longitudinal study in Matlab, Bangladesh. Eur J Clin Nutr (1990).
- Pecenka C, Parashar U, Tate JE, et al. Impact and cost-effectiveness of rotavirus vaccination in Bangladesh (2017).
- Paul RC, Faruque A, Alam M, et al. Incidence of severe diarrhoea due to Vibrio cholerae in the catchment area of six surveillance hospitals in Bangladesh. Epidemiol Infect 144 (2016): 927-939.
- Rahman A, Chowdhury S. Determinants of chronic malnutrition among preschool children in Bangladesh. J Biosoc Sci 39 (2007): 161-173.
- Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371 (2008): 243-260.
- Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6-59 months of age in pastoral community of Dollo Ado District, Somali region, Ethiopia. Sci J Public Health (2013).
- Nizame FA, Unicomb L, Sanghvi T, et al. Handwashing before food preparation and child feeding: a missed opportunity for hygiene promotion. Am J Trop Med Hyg 89 (2013): 1179-1185.
- Masibo PK, Makoka D. Trends and determinants of undernutrition among young Kenyan children: Kenya demographic and health survey; 1993, 1998, 2003 and 2008–2009. Public Health Nutr (2012).
- Alaimo K, Olson CM, Frongillo EA. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics 108 (2001): 44-53.
- Mitra SN, Al-Sabir A, Cross AR, et al. Bangladesh Demographic and Health Survey, 1996-1997. Dhaka and Calverton, Maryland: National Institute of Population Research and Training (NIPORT), Mitra and Associates, and Macro International Inc (1997).
- Das SK, Faruque ASG, Chisti MJ, et al. Changing trend of persistent diarrhoea in young children over two decades: observations from a large diarrhoeal disease hospital in Bangladesh. Acta Paediatr 101 (2012): e452-e457.
- Das SK, Rahman A, Chisti M, et al. Changing patient population in Dhaka Hospital and Matlab Hospital of icddr, b. Trop Med Int Health 19 (2014): 240-243.
- Implementing the new recommendations on the clinical management of diarrhoea. Geneva: World Health Organization (2006).
- Kundu DK, van Vliet BJ, Gupta A. The consolidation of deep tube well technology in safe drinking water provision: the case of arsenic mitigation in rural Bangladesh. Asian J TechnolInnov 24 (2016): 254-273.
- Winfrey W, McKinnon R, Stover J. Methods used in the lives saved tool (LiST). BMC Public Health 11 (2011): S32.
- National Institute of Population Research and Training (NIPORT), Mitra and Associates (MA), ORC Macro (ORCM). Bangladesh Demographic and Health Survey 1999-2000. Dhaka, Bangladesh and Calverton, Maryland [USA]: National Institute of Population Research and Training, Mitra and Associates, and ORC Macro (2001).
- El Arifeen S, Christou A, Reichenbach L, et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet 382 (2013): 2012-2026
- Chowdhury A, Cash R. A Simple Solution: Teaching Millions to Treat Diarrhoea at Home. University Press Limited, Dhaka (1996).
- National Institute of Population Research and Training (NIPORT) MaA, and ICF International, Bangladesh Demographic and Health Survey 2014 Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT, Mitra and Associates, and ICF International (2016).
- Sørup S, Benn CS, Poulsen A, et al. Live vaccine against measles, mumps, and rubella and the risk of hospital admissions for nontargeted infections. JAMA 311 (2014): 826-835.
- Ahmed F. Vitamin A deficiency in Bangladesh: a review and recommendations for improvement. Public Health Nutr 2 (1999): 1-14.
- Zohura F, Bhuyian SI, Monira S, et al. Observed handwashing with soap practices among cholera patients and accompanying household members in a hospital setting (CHoBI7 Trial). Am J Trop Med Hyg 95 (2016): 1314-1318.
- Winicki J, Jemison K. Food insecurity and hunger in the kindergarten classroom: its effect on learning and growth. Contemp Econ Policy (2003).
- Alom J, Quddus MA, Islam MA. Nutritional status of under-five children in Bangladesh: a multilevel analysis. J Biosoc Sci 44 (2012): 525-535.
- Mosley WH, Gray R. Childhood precursors of adult morbidity and mortality in developing countries: implications for health programs. Epidemiol Transit 1 (1993): 69-100.
- Das S, Gulshan J. Different forms of malnutrition among under-five children in Bangladesh: a cross-sectional study on prevalence and determinants. BMC Nutrition 3 (2017): 1.
- Ahsan KZ, El Arifeen S, Al-Mamun MA, et al. Effects of individual, household and community characteristics on child nutritional status in the slums of urban Bangladesh. Archives Public Health 75 (2017): 9.
- Alasfoor D, Traissac P, Gartner A, et al and improvements in health services in Oman. J Health Popul Nutr (2007): 359-369.
- Bangladesh Multiple Indicator Cluster Survey 2012-2013. ProgotirPathey: Final Report. Dhaka: Bangladesh Bureau of Statistics (BBS) and UNICEF Bangladesh (2014).
- Henry FJ, Briend A, Fauveau V, et al. Gender and age differentials in risk factors for childhood malnutrition in Bangladesh. Ann Epidemiol 3 (1993): 382-386.
- Chisti MJ, Hossain MI, Malek MA, et al. Characteristics of severely malnourished under-five children hospitalized with diarrhoea, and their policy implications. Acta Paediatr 96 (2007): 693-696.
- Handa S. Maternal education and child height. Econ Dev Cult Chang 47 (1999): 421-439.
- Tekce B, Shorter FC. Determinants of child mortality: a study of squatter settlements in Jordan. PopulDev Rev 10 (1984): 257-280.
- Bicego GT, Boerma JT. Maternal education and child survival: a comparative study of survey data from 17 countries. SocSci Med 36 (1993): 1207-1227.
- Caldwell JC, Reddy PH, Caldwell P. The social component of mortality decline: an investigation in South India employing alternative methodologies. Popul Stud 37 (1983): 185-205.
- Hossain MI, Yasmin R, Kabir I. Nutritional and immunization status, weaning practices and socio-economic conditions of under-five children in three villages of Bangladesh. Indian J Public Health 43 (1999): 37-41.