Determination of Serum Vitamin D3 Level by High Performance Liquid Chromatography (HPLC) in Patients with Coronary Artery Ectasia
Article Information
Naci Babat*, Yusuf Türkmen
Van Yuzuncu Yil University, Faculty of Medicine Department of Cardiology, Van, Turkey
*Corresponding author: Naci Babat, Van Yuzuncu Yil University, Faculty of Medicine Department of Cardiology, Van, 65090, Turkey
Received: 08 March 2020; Accepted: 16 March 2020; Published: 23 March 2020
Citation: Naci Babat, Yusuf Türkmen. Determination of Serum Vitamin D3 Level by High Performance Liquid Chromatography (HPLC) in Patients with Coronary Artery Ectasia. Cardiology and Cardiovascular Medicine 4 (2020): 097-104.
Share at FacebookAbstract
Background and Objectives: The net clinical effect of vitamin D on atherosclerosis and therefore coronary arteria ectasia (CEA) is controversial. While many trials have showed the favorable effects of vitamin-D others were related with negative outcomes and the exact levels of serum vitamin-D were not consistent with clinical outcomes. So therefore, we aimed to measure the levels of vitamin-D by HPLC technique which is better than conventional spectrophotometric methods.
Methods: A total of 202 patients were enrolled to our study and 102 of them were in patient group. They have diagnosed with CEA by angiographically and the level of vitamin-D was measured by High Performance Liquid Chromatography (HPLC) technique both in the patients of control and study group.
Results: There was no statistically meaningful difference between groups according to the basic but the serum levels of vitamin-D were lower in patients with CEA with a mean value of 20.5 ng/ml and the average amount of serum vitamin-D was 54.6 ng/ml in control subjects (p<0.001).
Conclusions: The serum levels of vitamin-D were detected as clearly lower by HPLC technique in patients with CEA and it has proved one more time the relation of lower levels of serum vitamin-D and CEA. At the same time, the method showed extremely high or totally normal values of vitamin-D levels in patients without CEA which has been not showed previous trials. Also, HPLC may yield more accurate results of serum vitamin-D than other spectrophotometric measuring techniques particularly in normal individuals.
Keywords
Coronary arteria; Ectasia; Vitamin-D; High performance liquid chromatography
Coronary arteria articles, Ectasia articles, Vitamin-D articles, High performance liquid chromatography articles
Article Details
Introduction
Cardiovascular diseases (CVD) have stayed the leading reasons of death globally in at least the past 30 years [1,2]. The vast majority of CVD are consisting of coronary artery disease, and a coronary arterial ectasia (CEA) is one of the well-known reason of CAD as result of atherosclerosis. Many studies have described the incidence of CEA between 1.7% and 5.4% [3,4]. The two recognized forms of CEA such as inflammatory and congenital types can be more frequent in early years of life, while atherosclerotic CAE is generally found in adults [4].
The net clinical effect of vitamin D on atherosclerosis and therefore CEA is controversial. Many years ago, it had been demonstrated that higher dose of vitamin-D result in vascular calcification [5]. Similarly, vascular calcinosis had detected in children as an outcome of vitamin-D therapy of rickets [6]. However, favorable effects of vitamin-D on cardiovascular system has also been showed in recent years [7]. Orally taken vitamin-D decreases the levels of serum triglycerides, pro-inflammatory mediators such as cytokines and regulates positively the hormone of parathyroid and improves flow mediated dilatation of arteries [8,9]. On the other hand, the lower levels of serum vitamin D were also associated with higher incidence of CAE [10]. All of these data clearly seem to conflicting to each other and it rises the suspicions of clinicians about the accuracy in the measurement of serum levels of vitamin-D.
Serum vitamin-D levels were measured by ELISA, standard liquid chromatography or chemiluminescence immunoassay techniques in previous trials [10-12]. However, high performance liquid chromatography (HPLC) is a technique which is superior than classical liquid chromatography (LC) in the separation of thermolabile and decomposable compounds and it is very applicable to separating substances such as amino acids, nucleic acids, carbohydrates, antibiotics, inorganic salts, and steroids. While classical LC able to isolate larger particles (>100 µm), HPLC technique can separate the particles even under 1,5 µm of diameter in a shorter time. In other words; the HPLC provides fast and efficient separation, separates and analyses very complex structures and gives accurate quantitative measurements. Therefore, HPLC is widely used for separation of molecules in biological, pharmaceutical, food, environmental and industrial process.
In this trial, we have also measured the serum levels of vitamin–D by HPLC technique and aimed to put forth the more accurate levels of vitamin-D in patients with CAE.
Method and patients
A total of 202 patients were enrolled to our study between June, 2018 and November, 2019. Patients divided into two groups which 102 of them have had CEA and other 100 patients were included to control group whose coronary angiography have showed no ectasia or significant stenosis. CEA described as an enlargement with a diameter of one and half times the contiguous normal coronary artery. Presence of all CEA was confirmed by angiographically. Visualization and evaluation of coronary arteries was performed by two cardiologists and the presence of narrowing more than 50% in epicardial major arteries was accepted as significant stenosis. Patients with kidney, liver and structural heart diseases were excluded. Vitamin-D or calcium treatments were also another exclusion criteria in this trial. The written informed consents of all patients were obtained prior to their enrollment. Also, the study was approved by the local ethics committee of the university, in accordance with the ethical principles for human investigations, as outlined in the second Declaration of Helsinki.
Sample collection and analysis
The patients both in control and study groups were stayed at night at the hospital and blood samples were collected after at least 10 hours of fasting into anticoagulant tubes. Serum was obtained by centrifugation at 5000 rpm for 15 minutes and stored at −80°C until assayed. Fasting blood glucose, aspartate aminotransferase, alanine aminotransferase, creatinine, low-density lipoprotein cholesterol, high-density cholesterol, and triglyceride levels were recorded. Additional blood was gathered into ethylene diaminetetraacetic acid contained tubes in order to count whole blood and examined by Coulter LH 780 Hematology Analyzer (Beckman Coulter Ireland Inc., Mervue, Galway, Ireland).
Analysis of vitamin-D levels by the HPLC Method
The quantitative analysis of serum vitamin-D (cholecalciferol) was determined by high performance liquid chromatography (HPLC, Agilent-1100 series, Germany) according to the procedure modified from the relevant literatures [13-15]. In the measurement of vitamin-D, 200 µl of ethanol was added to 200 µl of plasma and they have vortexed together. Then, 800 µl of hexane was added and the mixture was vortexed again for 2 min. After centrifugation, the lipophilic hexane phase was collected and dried under N2 gas. Then it was re-dissolved in 200 µl ethanol, and 20 µl of sample was injected into an HPLC system fitted with a 5µm C18 reverse-phase column (C18, 250 x 4.6 mm, Supelco, at room temperature). As a mobile phase, methanol-water (98:2) was used in 1.5 ml/min flow rate. In the quantitative determination of the vitamins D, diode-array detector was employed in 265 nm wavelength. Double distilled water was used during the procedure. All the chemical reagents were of analytical grade and commercially available (Merck Company).
Statistical analysis
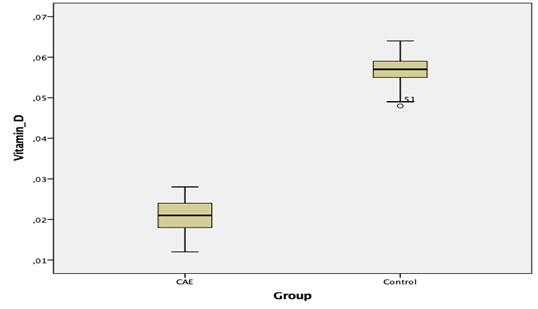
We were stated the statistical data as an average, standard deviation, minimum and maximum values. Student’s t-test was chosen in the comparison of the basic features of groups. Univariate and multivariate regression analyses were completed to guess (with a confidence interval [CI] of 95%) the existence of ectasia by considering age, gender, smoking, hypertension, hyperlipidemia, and vitamin D levels. Also, Box and Whisker Plot graph was obtained by the use of MedCalc®v15.4 package software. Statistically significance level accepted as 5% and SPSS (version:13 SPSS Inc., Chicago, IL, USA) package program was used.
Results
A total of 124 men and 78 women enrolled to our study. Study group included 102 (61 men) patients who were diagnosed with CEA by angiographically and there were 100 patients (63 men) in control group whose coronary arteries were normal. The average age of patients was 55.28±9.14 and 54.72±9.85 years in study and control group of patients respectively. Comparison of descriptive features and biochemical blood results of patients between groups have shown below (Table 1). There was no statistically meaningful difference between groups according to the basic features and blood results except the level of vitamin–D. The serum levels of vitamin-D were extremely lower in patients with CEA regarding to normal range of 30-100 ng/ml, with a mean value of 20.5 ng/ml irrespective of gender. On the other hand, in control subjects the average amount of serum vitamin-D was 54.6 ng/ml which corresponds to the totally normal ranges (p<0.001). In addition, we would like to evaluate the lower amounts of serum vitamin-D as an independent risk factor in the formation of CEA and so therefore, the well-known atherosclerotic risk factors such as age, hypertension, male gender, hyperlipidemia, and smoking as well as vitamin-D were analyzed by both univariate and multivariate logistic regression analysis. The lower serum levels of vitamin-D (odds ratio [OR]=0.879, 95% CI 0.836-0.949, p<0.001) was clearly found as independently correlated with the presence of isolated CEA. Furthermore, the analyzed values of serum vitamin-D has shown below by the help of Box and Whisker Plot graphics in both control and study group of patients and the enormous difference between groups were clearly visible in the mentioned box and graphics (Figure 1).
CEA (n=102) Control (n=100)
|
Parameters |
Average |
Min |
Max |
Average |
Min |
Max |
P-value |
|
|
Height (cm) |
172.46±6.56 |
160 |
188 |
172.34±7.3 |
160 |
190 |
0.931 |
|
|
Weight (kg) |
80.4±6.94 |
65 |
94 |
79.36±6.05 |
64 |
92 |
0.426 |
|
|
Age (year) |
55.28±9.14 |
35 |
70 |
54.72±9.85 |
35 |
70 |
0.769 |
|
|
Hemoglobin (gr/dl) |
13.44±2.03 |
8.5 |
16,5 |
13.95±1.74 |
9.3 |
16.9 |
0.181 |
|
|
Hematocrit (%) |
40.42±6.13 |
25 |
54.71 |
41.56±4.81 |
28.6 |
51.1 |
0.303 |
|
|
Platelet (x103/µl) |
246.36±65.32 |
113 |
394 |
246.38±68.09 |
119 |
414 |
0.999 |
|
|
Glucose (mg/dl) |
106.4±18.42 |
70 |
151 |
110.9±28.91 |
73 |
225 |
0.356 |
|
|
AST* (unit/L) |
18.36±9.08 |
6 |
54 |
19.92±7.87 |
6 |
44 |
0.361 |
|
|
ALT** (unit/L) |
19.84±6.83 |
4 |
46 |
20.96±8.18 |
9 |
50 |
0.459 |
|
|
Creatinine (mg/dl) |
0.89±0.29 |
0.47 |
1.5 |
0.86±0.24 |
0.21 |
1.53 |
0.504 |
|
|
Sodium (mEq/L) |
139.02±3.69 |
130 |
150 |
138.6±4.77 |
121 |
154 |
0.624 |
|
|
HDL-C§ (mg/dl) |
40.08±9.31 |
17 |
64 |
41.52±8.06 |
28 |
64 |
0.411 |
|
|
LDL-C¶ (mg/dl) |
119.5±36.26 |
49 |
203 |
124±48.62 |
13 |
223 |
0.601 |
|
|
Triglyceride (mg/dl) |
166.18±115.61 |
60 |
675 |
175.24±95.44 |
59 |
467 |
0.672 |
|
|
Vitamin-D (ng/mL) |
20.5±7.8 |
11 |
29.2 |
54.6±10.1 |
51 |
66.6 |
0.001 |
Table 1: Comparison of study and control group patients according to their basic clinical and biochemical features. *AST: Aspartate aminotransferase, **ALT: Alanine aminotransferase, §HDL-C: High density lipoprotein cholesterol, ‡LDL-C: Low density lipoprotein cholesterol.
|
Variables |
Univariate |
Multivariate |
||||||
|
OR* (95% CI**) |
p |
Adjusted OR (95% CI) |
p |
|||||
|
Age |
0.104 (0.957-1.082) |
0.817 |
1.039 (0.965-1.092) |
0.941 |
||||
|
Smoking |
1.017 (0.891-1.195) |
0.381 |
1.065 (0.904-1.251) |
0.109 |
||||
|
Male gender |
0.929 (0.905-0.986) |
0.576 |
0.918 (0.901-0.971) |
0.239 |
||||
|
Hypertension |
0.968 (0.792-1.271) |
0.716 |
0.988 (0.782-1.353) |
0.897 |
||||
|
Hyperlipidemia |
0.880 (0.425-1.867) |
0.745 |
0.665 (0.310-1.713) |
0.372 |
||||
|
Vitamin-D |
0.899 (0.849-0.953) |
0.001 |
0.879 (0.836-0.949) |
0.001 |
||||
Table 2: Independent predictors for the occurrence of CEA in both univariate and multivariate logistic regression analysis. *OR: odds ratio, **CI: confidence interval.
Discussion
To our knowledge, this is the first study in literature which investigates the level of serum vitamin-D by HPLC technique in patients with CEA and we have found significantly lower levels of vitamin-D in study group of patients than patients of control group. Many trials have demonstrated previously the negative cardiovascular effects of vitamin-D insufficiency [16-18] but there is no consensus about the right levels of vitamin-D in patients with CEA. For this purpose, it was an obligation to measure the exact levels of serum vitamin-D by more accurate method. Vitamin-D accepted as hormone in the body and it has a steroid structure [19]. As mentioned above, HPLC is more applicable and useful in the measurement of foods, antibiotics, steroids, and many other soluble. Galleli et al. have used HPLC and other techniques in the detection of vitamin-D levels in patients with migraine and they have found that HPLC was the most appropriate method in the accurately detection of serum vitamin-D levels [20]. We have not directly compared the HPLC with other spectrophotometric techniques but according to the study of Cagirci et al, the level of vitamin-D was found as 15.1±8.2 ng/ml and 24.3±7.4 ng/ml in the study and control group of patients respectively [10]. Whereas both of these levels are not in normal ranges in fact according to the Institute of Medicine [21]. Levels lower than 21 ng/ml and 30 ng/ml were defined as deficiency and insufficiency of vitamin-D separately. One of another study showed the levels of vitamin-D as 18.9±8.5 ng/ml in the presence of CEA and 31.2±11.2 ng/ml in patients whose coronary arteries were totally normal [22]. Enzymatic-colorimetric assay was used in the detection of vitamin-D levels in both of these mentioned trials. However, we have detected the average amount of serum vitamin-D as 20.5±7.8 ng/ml in patients with CEA which was obviously lower than normal values, but it was 54.6±10.1 ng/ml in patients of control group and the latter is undoubtedly well-matched with totally normal values of serum vitamin-D. In other words, there was serious differences of serum vitamin-D levels between patients with and without CEA. We believe that, these enormous differences were obtained as a result of the measurement of vitamin-D by HPLC technique. During HPLC, substances are expose to the very high levels of pressure and it can decompose the structures from each other and gives an opportunity to measure the exact levels of the compounds.
On the other hand, we have obviously detected lower levels of vitamin-D in subjects with CEA. It was an expected result actually and was compatible with the results of previous studies [10,19]. The demonstration of lower levels of vitamin-D by HPLC technique in patients with CEA was important because of higher accuracy levels of the technique. For the first time, we have proved the relation of CEA and lower levels of vitamin-D which measured by HPLC technique.
In conclusion, the serum levels of vitamin-D were detected as clearly lower by HPLC technique in patients with CEA and it proves one more time the relation of lower levels of serum vitamin-D and CEA. At the same time, the method showed extremely high or totally normal values of vitamin-D levels in patients without CEA. Also, HPLC may yield more accurate results of serum vitamin-D than other spectrophotometric measuring techniques particularly in normal individuals.
Limitations of the study
We have measured the levels of vitamin-D during whole part of the year regardless of its seasonal variations but blood samples of both control and study group patients were obtained at the same day and so therefore, the seasonal effects may not take an important role in the comparison of vitamin-D levels between the groups. Furthermore, we could have detected the correlation of serum vitamin-D levels and the severity of ectasia in order to show the potential effect of vitamin-D to ectasia but it was not in the scope of this trial. Also, this was the first trial which measures the levels of vitamin-D by HPLC method in patients with CEA and definitely we need more trails in this field to decide the superiority of HPLC than traditional methods.
Acknowledgments
We are grateful to Prof. Dr. Demir because of his unlimited support in the understanding of HPLC method and the measurement of serum vitamin-D levels both in control and study group of patients.
Conflict of interest
The authors declare that there is no conflict of interest.
Financial support
Current trial was financially supported by the Chemistry Department of Yuzuncu Yil University.
References
- Colin D. Mathers,Ties Boerma,Doris Ma Fat. Global and regional causes of death. British Medical Bulletin 92 (2009): 7-32.
- Murray CJ,Lopez AD. Mortality by cause for eight regions of the world: Global Burden ofDiseaseStudy. Lancet349 (1997): 1269-76.
- Hartnell GG,Parnell BM,Pridie RB.Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients.Br Heart J54 (1985): 392-395.
- VP Demopoulos, CD Olympios, CN Fakiolas, EG Pissimissis, NM Economides, E Adamopoulou, etal.The natural history of aneurysmal coronary artery disease.Heart78 (1997): 136-141.
- Jahreis G, Hesse V. Vitamin D-induced tissue calcinosis and arteriosclerosis changes. I: a contribution to the 60-year history of vitamin D research with special reference to childhood. Padiatr Grenzgeb 29 (1990): 203-11.
- Kobylinski S, Häfer B, Kohde G. Correlative pathologic studies on the role of vitamin D in vascular calcinosis in childhood. Zentralbl Allg Pathol 129 (1984): 137-47.
- Zittermann A, Gummert JF. Sun, vitamin D, and cardiovascular disease. J Photochem Photobiol B 101 (2010): 124-9.
- Zittermann A, Frisch S, Berthold HK, Götting C, Kuhn J, Kleesiek K, et al. Vitamin D supplementation enhances the beneficial effects of weight loss on cardiovascular disease risk markers. Am J Clin Nutr 89 (2009): 1321-7.
- Harris RA, Pedersen-White J, Guo DH, Stallmann-Jorgensen IS, Keeton D, Huang Y, et al. Vitamin D3 supplementation for 16 weeks improves flow-mediated dilation in overweight African–American adults. Am J Hypertens 24 (2011): 557-62.
- Cagirci G, Kucukseymen S, Yuksel IO, Bayar N, Koklu E, Guven R, et al. The Relationship between Vitamin D and Coronary Artery Ectasia in Subjects with a Normal C-Reactive Protein Level. Korean Circ J 47 (2017): 231-237.
- Enko D, Kriegshäuser G, Stolba R, Worf E, Halwachs-Baumann G. Method evaluation study of a new generation of vitamin D assays. Biochem Med (Zagreb) 25 (2015): 203-12.
- Lupton JR, Faridi KF, Martin SS, Sharma S, Kulkarni K, Jones SR, et al. Deficient serum 25-hydroxy vitamin D is associated with an atherogenic lipid profile: The Very Large Database of Lipids (VLDL-3) Study. J Clin Lipidol 10 (2016): 72-81.
- Rodriguez-Porcel M, Lerman LO, Herrmann J, Sawamura T, Napoli C, Lerman A. Hypercholesterolemia and hypertension have synergistic deleterious effects on coronary endothelial function. Arterioscler Thromb Vasc Biol 23 (2003): 885-891.
- Serdar Z, Aslan K, Dirican M, Sarandöl E, Yeşilbursa D, Serdar A. Lipid andprotein oxidation and antioxidant status in patients with angiographically proven coronary artery disease. Clin Biochem 39 (2006): 794-803.
- Odeh RM, Cornish LA. Natural antioxidants for the prevention of atherosclerosis. Pharmacotherapy 15 (1995): 648-59.
- Kota SK, Kota SK, Jammula S, Meher LK, Panda S, Tripathy PR, et al. Renin-angiotensin system activity in vitamin D deficient, obese individuals with hypertension: an urban Indian study. Indian J Endocrinol Metab 4 (2011): 395-401.
- Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP. 1, 25-Dihydroxyvitamin D3 is a negative endocrine regulator of the renin-angiotensin system.Journal of Clinical Investigation110 (2002): 229-38.
- Zittermann A, Ernst JB, Prokop S, Fuchs U, Dreier J, Kuhn J, et al. Effects of Vitamin D Supplementation on Renin and Aldosterone Concentrations in Patients with Advanced Heart Failure: The EVITA Trial. Int J Endocrinol 2018: 5015417.
- Linda L. Demer, Jeffrey J. Hsu, Yin Tintut. Steroid hormone vitamin D. Circulation research 122 (2018): 1576-1585.
- Gallelli L, Michniewicz A, Cione E, Squillace A, Colosimo M, Pelaia C, et al. 25-Hydroxy Vitamin D Detection Using Different Analytic Methods in Patients with Migraine. J Clin Med8 (2019): 895.
- Catharine Ross. The 2011 report on dietary reference intakes for calcium and vitamin D. Public Health Nutr 14 (2011): 938-9.
- Demir M, Demir C, Keçeoğlu S. The relationship between vitamin D deficiency and coronary artery ectasia. Postepy Kardiol Interwencyjnej 10 (2014): 238-41.