Covid-19 Impact on Mental Health of Egyptians Patients
Article Information
Abdel-Fattah HM1,2*, Hussein KA3, Bahary H4
1Neuropsychiatry Specialist, Abbassia Psychiatric Hospital, Cairo, Egypt
2The Egyptian Ministry of Health-General Secretariat for Mental Health and Addiction Treatment - Al-Abbassia psychiatric Hospital, Cairo, EGYPT
3Neuropsychiatry Free Specialist, TQM Specialist, Cairo, EGYPT
4Professor of psychiatry, Al-Azhar University, Cairo, EGYPT
*Corresponding Author: Dr. Hesham Maged abdelfatah, Neuropsychiatry Specialist, the Egyptian Ministry of Health-General Secretariat for Mental Health and Addiction Treatment - Al-Abbassia psychiatric Hospital, Cairo, EGYPT
Received: 02 June 2020; Accepted: 09 June 2020; Published: 16 June 2020
Citation: Abdel-Fattah HM, Hussein KA, Bahary H. Covid-19 Impact on Mental Health of Egyptians Patients. Journal of Psychiatry and Psychiatric Disorders 4 (2020): 87-93.
Share at FacebookAbstract
The current study is aimed to examine the rates of mental disorders in a sample of Egyptian patients due to environmental factors associated with the COVID-19 pandemic crisis which interacted with the historical and religious background of the Egyptian people. The research was performed in four different districts in Cairo and Giza before and during the outbreak of a pandemic. The Control group consisted of 1600 patients and extended from the first of October till the end of December 2019. The experimental group consisted of 1200 patients during the first four months of 2020. Mood disorders were the main psychiatric disorders that appeared during this period in the form of depression and anxiety disorders. Also, the cases of substance use disorder (SUD) and obsessive-compulsive disorders (OCD) were presented more in psychiatric clinics. The percentage of male patients was slightly higher in depressive cases, while it was significantly higher in SUD cases. On the other hand, the percentage of female patients was a little higher in anxiety disorders and OCD cases. The percentage of SUD cases was significantly higher among highly educated patients and also in OCD cases. Medium educated patients presented with depression and anxiety disorders were slightly higher than high educated patients and significantly higher than low educated ones.
Keywords
Psychiatry; COVID-19; Mood disorders; Egyptian mental health
Psychiatry articles, COVID-19 articles, Mood disorders articles, Egyptian mental health articles
Psychiatry articles Psychiatry Research articles Psychiatry review articles Psychiatry PubMed articles Psychiatry PubMed Central articles Psychiatry 2023 articles Psychiatry 2024 articles Psychiatry Scopus articles Psychiatry impact factor journals Psychiatry Scopus journals Psychiatry PubMed journals Psychiatry medical journals Psychiatry free journals Psychiatry best journals Psychiatry top journals Psychiatry free medical journals Psychiatry famous journals Psychiatry Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Mood disorders articles Mood disorders Research articles Mood disorders review articles Mood disorders PubMed articles Mood disorders PubMed Central articles Mood disorders 2023 articles Mood disorders 2024 articles Mood disorders Scopus articles Mood disorders impact factor journals Mood disorders Scopus journals Mood disorders PubMed journals Mood disorders medical journals Mood disorders free journals Mood disorders best journals Mood disorders top journals Mood disorders free medical journals Mood disorders famous journals Mood disorders Google Scholar indexed journals Egyptian mental health articles Egyptian mental health Research articles Egyptian mental health review articles Egyptian mental health PubMed articles Egyptian mental health PubMed Central articles Egyptian mental health 2023 articles Egyptian mental health 2024 articles Egyptian mental health Scopus articles Egyptian mental health impact factor journals Egyptian mental health Scopus journals Egyptian mental health PubMed journals Egyptian mental health medical journals Egyptian mental health free journals Egyptian mental health best journals Egyptian mental health top journals Egyptian mental health free medical journals Egyptian mental health famous journals Egyptian mental health Google Scholar indexed journals obsessive-compulsive disorders articles obsessive-compulsive disorders Research articles obsessive-compulsive disorders review articles obsessive-compulsive disorders PubMed articles obsessive-compulsive disorders PubMed Central articles obsessive-compulsive disorders 2023 articles obsessive-compulsive disorders 2024 articles obsessive-compulsive disorders Scopus articles obsessive-compulsive disorders impact factor journals obsessive-compulsive disorders Scopus journals obsessive-compulsive disorders PubMed journals obsessive-compulsive disorders medical journals obsessive-compulsive disorders free journals obsessive-compulsive disorders best journals obsessive-compulsive disorders top journals obsessive-compulsive disorders free medical journals obsessive-compulsive disorders famous journals obsessive-compulsive disorders Google Scholar indexed journals substance use disorder articles substance use disorder Research articles substance use disorder review articles substance use disorder PubMed articles substance use disorder PubMed Central articles substance use disorder 2023 articles substance use disorder 2024 articles substance use disorder Scopus articles substance use disorder impact factor journals substance use disorder Scopus journals substance use disorder PubMed journals substance use disorder medical journals substance use disorder free journals substance use disorder best journals substance use disorder top journals substance use disorder free medical journals substance use disorder famous journals substance use disorder Google Scholar indexed journals human immunodeficiency virus articles human immunodeficiency virus Research articles human immunodeficiency virus review articles human immunodeficiency virus PubMed articles human immunodeficiency virus PubMed Central articles human immunodeficiency virus 2023 articles human immunodeficiency virus 2024 articles human immunodeficiency virus Scopus articles human immunodeficiency virus impact factor journals human immunodeficiency virus Scopus journals human immunodeficiency virus PubMed journals human immunodeficiency virus medical journals human immunodeficiency virus free journals human immunodeficiency virus best journals human immunodeficiency virus top journals human immunodeficiency virus free medical journals human immunodeficiency virus famous journals human immunodeficiency virus Google Scholar indexed journals psychiatric articles psychiatric Research articles psychiatric review articles psychiatric PubMed articles psychiatric PubMed Central articles psychiatric 2023 articles psychiatric 2024 articles psychiatric Scopus articles psychiatric impact factor journals psychiatric Scopus journals psychiatric PubMed journals psychiatric medical journals psychiatric free journals psychiatric best journals psychiatric top journals psychiatric free medical journals psychiatric famous journals psychiatric Google Scholar indexed journals Analysis of Variance articles Analysis of Variance Research articles Analysis of Variance review articles Analysis of Variance PubMed articles Analysis of Variance PubMed Central articles Analysis of Variance 2023 articles Analysis of Variance 2024 articles Analysis of Variance Scopus articles Analysis of Variance impact factor journals Analysis of Variance Scopus journals Analysis of Variance PubMed journals Analysis of Variance medical journals Analysis of Variance free journals Analysis of Variance best journals Analysis of Variance top journals Analysis of Variance free medical journals Analysis of Variance famous journals Analysis of Variance Google Scholar indexed journals mental disorders articles mental disorders Research articles mental disorders review articles mental disorders PubMed articles mental disorders PubMed Central articles mental disorders 2023 articles mental disorders 2024 articles mental disorders Scopus articles mental disorders impact factor journals mental disorders Scopus journals mental disorders PubMed journals mental disorders medical journals mental disorders free journals mental disorders best journals mental disorders top journals mental disorders free medical journals mental disorders famous journals mental disorders Google Scholar indexed journals
Article Details
1. Introduction
In just a few months, the COVID-19 pandemic has taken the entire world by storm. From the political North to the South, within economically poor and rich countries, the mortality rate from the pandemic has reached a scale hitherto not seen in a generation. Health systems and economies in both developed and developing countries are challenged in ways not imagined. The global efforts to mitigate the effects of the pandemic are moving at a very fast pace. Therefore, it is very essential to focus on psychiatric disorders that appear before and during the crisis. Also in order to deal with these problems and to enhance the individuals’ psychological rigidity as well as the community consolidation in facing, accepting, and living with reality [1].
Chronic infectious diseases such as tuberculosis and human immunodeficiency virus (HIV) are associated with higher levels of mental illness as compared with the general population [2].
COVID-19 has rippling effects like stigma, and medical mistrust especially based on current public reactions. Psychiatrists have a great role to help their patients and the greater communities. Stigmatization of affected individuals and health care professionals has been seen in multiple countries including Egypt [3].
Mistrust of medical organizations due to untruthful information comes from untruthful sites and rumors which reinforce the stigma and perceived discrimination and result in lower adherence to health recommendations. Clinicians must maintain a scientific, fact-based, and emphasizing the importance of overall infection control practices in the wake of COVID-19 [4].
Our research was performed on 2800 patients in four different psychiatric private clinics in different areas in Cairo and Giza in EGYPT. The data were collected before and during the outbreak of COVID-19 in the period from October 2019 until April 2020.
2. Patients and Methods
Total sample collected (2800 cases) from four private psychiatric clinics; two in Cairo and two in Giza divided into two groups, the first is control group sample number (1600 patients) attended from the period of Oct., Nov. and Dec. 2019 which represent the period before the appearance of COVID-19.
The second is experimental group sample number (1200 patients) from the same psychiatric clinics during the invasion of COVID-19 attended from the beginning of Jan. till the end of April 2020.
We study the impact of COVID-19 on the mental health map. Data were statistically analyzed by Analysis of Variance (ANOVA) test using a computer software SAS [5].
3. Results and Discussion
3.1 Main common mental disorders before COVID-19 invasion
(Figure 1) shows the percentage of common mental illnesses in the control group sample before the invasion of COVID-19 where depression represents 23%, anxiety disorders represent 14%, SUD equals 8% and OCD is 5%, while psychotic patients and other mental illnesses represent 50% of the cases. These findings are matching with estimates of preference of the common mental disorders in normal time [6].
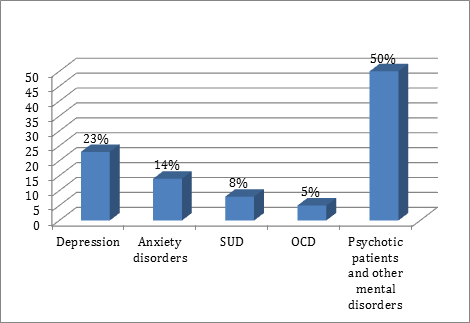
Figure 1: Percentage of common mental disorders in the control group sample.
3.2 Main common mental disorders during COVID-19 invasion
(Figure 2) shows that the percentage of cases presented with depression, anxiety disorders, SUD, and OCD are increasing somehow especially during the first four months of 2020, which represent the era of COVID-19. The percentage of patients with other mental disorders has declined by the start of 2020 up till the end of April 2020 (50.0 and 15.5%, respectively). About one-third of the cases were presented by depressive disorders followed by anxiety disorders (26%) and substance use disorders (SUD) (16%) Obsessive-compulsive disorder (OCD) presented 12% of the cases.
In the current study, the high rate of seeking treatment inpatient diagnosed as SUS may be due to many factors connected with the Egyptian community norms as religious standards leading to fear from death by COVID-19. It could be also associated with the depressive and anxiety symptoms accompanying and leakage of money due to worldwide financial crisis or a maladaptive behavior to stress and anxiety caused by COVID-19 by increasing the consumption of alcohol and substance use disorders then seeking help to treatment. Noticeable decreases in psychotic patients during this time may be attributed to the home as a safe zone for this type of patient; some of them are not orientated by the crisis or lack of fair judgment.
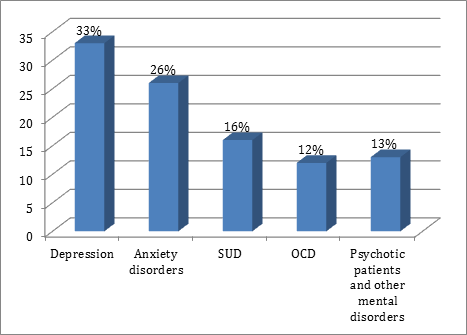
Figure 2: Percentage of common mental disorders in the experimental group sample.
3.3 Gender differences and mental disorders in the pandemic
(Figure 3) illustrates that the male cases presented by depressive symptoms were slightly higher than female cases (19 and 14% for male and female cases, respectively). This difference could be attributed to staying home as a stressor for depression in males as well as the financial problems in contrast with normal timing where the rate of depression is almost equal between males and females. The same finding was found to regard SUD, where male cases were significantly higher (14%) than the female ones (2%) as it is almost the same ratio in normal situations. The reverse was found regarding anxiety disorders where the female cases were 15% while the male cases were 11%. A highly significant increase of the female cases presented by OCD (9%) than the male cases (3%) was recorded. Despite the ratio of OCD is almost the same between males and females in normal timing but during the COVID-19 era three folds in females due to higher emotion in females and fear about children, family, and relatives.
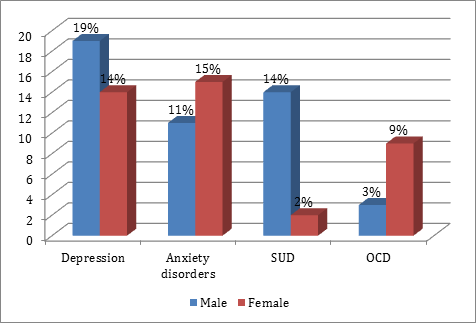
Figure 3: Comparison between male and female mental disorders in the experimental group sample.
3.4 Educational levels and mental disorders in the pandemic
(Figure 4) illustrates that the numbers of substance use disorders (SUD) cases were significantly higher between highly educated patients than medium and low education (9, 5, and 2%, respectively). The same figure could be noticed as regard OCD cases (7, 4, and 1% for high, medium, and low education, respectively). On the other hand, medium education patients who were presented with depression and anxiety disorders in the psychiatric clinics were slightly higher than high education cases and significantly higher than low education cases. The higher educational level seems to have a protective effect against anxiety and depression, which accumulates throughout life [7]. Low educational level had the lowest rate of depression and GAD that could be attributed to insufficient awareness and perhaps they may still in the denial phase of crisis. High incidence of OCD in higher education level might be because of increasing awareness and the insight. Increasing the seeking for treatment for patients of SUD in high education level could be due to higher awareness and the insight about dangerous of COVID-19 and its subsequent mortality.
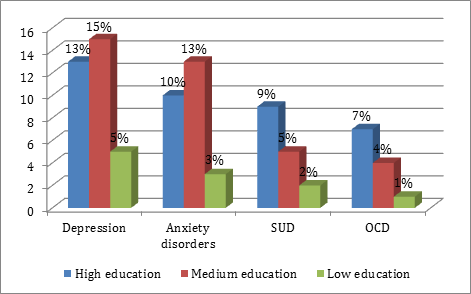
Figure 4: Comparison between different educational levels of mental disorders in the experimental group sample.
Summary and Recommendations
The main mental disorders that appeared in pandemic COVID-19 are depression and anxiety disorders and also SUD and OCD cases. The number of psychotic patients declined during the pandemic period. Males are subjected to depressive disorders slightly more than females, while females are more easily to suffer from anxiety disorders and OCD so due to its biopsychosocial origins we must focus on the different types of Psychotherapy as Cognitive Therapy, Behavioral Therapy, Cognitive-Behavioral Therapy, Dialectical Behavior Therapy, Psychodynamic Therapy, Interpersonal Therapy, and Educational Therapy.
Male patients with SUD seeking treatment are much higher than female ones during the crisis so It is important to focus on addiction treatment in crisis due to increasing the rate of seeking treatment and this is ideal the time to use of the addicts’ motivation and enthusiasm to reach a successful addiction management plan and programs either in-home or in addictions treatment hospitals and centers.
Medium educated patients presented with depression and anxiety disorders were slightly higher than high educated cases and significantly higher than low educated ones so we must focus on medical awareness and health promotion programs that match and reached all educational levels.
We also need to focus on training and psychological support programs and open the door to volunteers and community stars for training in this area for all patients suspected of being infected or who have been diagnosed with COVID-19 and their relatives, and psychological support for other medical services providers.
We also advise the presence of recommended written guidelines for psychological treatment criteria for patients of this epidemic who suffer from mental illnesses and to determine the treatment plans and medications allowed so we avoiding the drug-drug interactions with other medical treatments which reflected negatively on the prognosis of the disease.
Finally, studies and research must continue during this epidemic, as well as after it is over to know all the psychological effects that can be overcome in order to protect and the well-being of humanity.
References
- Moukaddam N, Shah A. Psychiatrists beware: the impact of COVID-19 and pandemics on mental health. Psychiatric Times: MH Life Sciences 37 (2020):1-3.
- van den Heuvel L, Chishinga N, Kinyanda E. Frequency and correlates of anxiety and mood disorders among TB- and HIV-infected Zambians. AIDS Care 25 (2013):1527-1535.
- Shigemura J, Ursano RJ, Morganstein JC. Public responses to the novel 2019 coronavirus in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. Epub ahead of print (2019).
- Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav. Med 45 (2019):79-85.
- SAS (Statistical Analysis System). SAS Release 9.1 for windows, SAS Institute INC. Cary, NC, USA (2003).
- WHO/MSD/MER/2. Depression and other common mental disorders, global health estimated (2017).
- Bjelland I, Krokstad S, Mykletun A, et al. Does a higher educational level protect against anxiety and depression? Soc. Sci. Med 66 (2008):1334-1345.
