Corticosteroids as a cause of Catastrophic Rheumatoid Arthritis
Article Information
Eleftherios Pelechas1*, Tereza Memi1, Nafsika Gerolymatou1, Georgios zouzos1, Panagiota Karagianni2
1Division of Rheumatology, Department of Internal Medicine, Medical School, University of Ioannina, Greece
2Biopathology Department, Medical School, University of Ioannina, Greece
*Corresponding Author: Eleftherios Pelechas, Division of Rheumatology, Department of Internal Medicine, Medical School, University of Ioannina, Greece
Received: 20 June 2019; Accepted: 03 July 2019; Published: 08 July 2019
Citation:
Eleftherios Pelechas, Tereza Memi, Nafsika Gerolymatou, Georgios zouzos, Panagiota Karagianni. Corticosteroids as a cause of Catastrophic Rheumatoid Arthritis. Fortune Journal of Rheumatology 1 (2019): 015-017.
Share at FacebookAbstract
A 71-year-old woman has been using corticosteroids since the age of 25. After a fall, she developed multiple compression fractures of the spine. Despite the obvious bone deformities during the physical examination in upper limbs, she denied any pain. Radiologic and a CT-scan evaluation revealed catastrophic lesions with a completely destroyed joint and many intra-articular free bodies. Long-term corticosteroid use can bring on catastrophic results in bone structures and patients must be properly informed regarding the side effects.
Keywords
Rheumatoid arthritis, Corticosteroids, Side effects
Rheumatoid arthritis articles Rheumatoid arthritis Research articles Rheumatoid arthritis review articles Rheumatoid arthritis PubMed articles Rheumatoid arthritis PubMed Central articles Rheumatoid arthritis 2023 articles Rheumatoid arthritis 2024 articles Rheumatoid arthritis Scopus articles Rheumatoid arthritis impact factor journals Rheumatoid arthritis Scopus journals Rheumatoid arthritis PubMed journals Rheumatoid arthritis medical journals Rheumatoid arthritis free journals Rheumatoid arthritis best journals Rheumatoid arthritis top journals Rheumatoid arthritis free medical journals Rheumatoid arthritis famous journals Rheumatoid arthritis Google Scholar indexed journals Corticosteroids articles Corticosteroids Research articles Corticosteroids review articles Corticosteroids PubMed articles Corticosteroids PubMed Central articles Corticosteroids 2023 articles Corticosteroids 2024 articles Corticosteroids Scopus articles Corticosteroids impact factor journals Corticosteroids Scopus journals Corticosteroids PubMed journals Corticosteroids medical journals Corticosteroids free journals Corticosteroids best journals Corticosteroids top journals Corticosteroids free medical journals Corticosteroids famous journals Corticosteroids Google Scholar indexed journals Side effects articles Side effects Research articles Side effects review articles Side effects PubMed articles Side effects PubMed Central articles Side effects 2023 articles Side effects 2024 articles Side effects Scopus articles Side effects impact factor journals Side effects Scopus journals Side effects PubMed journals Side effects medical journals Side effects free journals Side effects best journals Side effects top journals Side effects free medical journals Side effects famous journals Side effects Google Scholar indexed journals fractures articles fractures Research articles fractures review articles fractures PubMed articles fractures PubMed Central articles fractures 2023 articles fractures 2024 articles fractures Scopus articles fractures impact factor journals fractures Scopus journals fractures PubMed journals fractures medical journals fractures free journals fractures best journals fractures top journals fractures free medical journals fractures famous journals fractures Google Scholar indexed journals spine articles spine Research articles spine review articles spine PubMed articles spine PubMed Central articles spine 2023 articles spine 2024 articles spine Scopus articles spine impact factor journals spine Scopus journals spine PubMed journals spine medical journals spine free journals spine best journals spine top journals spine free medical journals spine famous journals spine Google Scholar indexed journals bone deformities articles bone deformities Research articles bone deformities review articles bone deformities PubMed articles bone deformities PubMed Central articles bone deformities 2023 articles bone deformities 2024 articles bone deformities Scopus articles bone deformities impact factor journals bone deformities Scopus journals bone deformities PubMed journals bone deformities medical journals bone deformities free journals bone deformities best journals bone deformities top journals bone deformities free medical journals bone deformities famous journals bone deformities Google Scholar indexed journals Radiologic articles Radiologic Research articles Radiologic review articles Radiologic PubMed articles Radiologic PubMed Central articles Radiologic 2023 articles Radiologic 2024 articles Radiologic Scopus articles Radiologic impact factor journals Radiologic Scopus journals Radiologic PubMed journals Radiologic medical journals Radiologic free journals Radiologic best journals Radiologic top journals Radiologic free medical journals Radiologic famous journals Radiologic Google Scholar indexed journals bone structures articles bone structures Research articles bone structures review articles bone structures PubMed articles bone structures PubMed Central articles bone structures 2023 articles bone structures 2024 articles bone structures Scopus articles bone structures impact factor journals bone structures Scopus journals bone structures PubMed journals bone structures medical journals bone structures free journals bone structures best journals bone structures top journals bone structures free medical journals bone structures famous journals bone structures Google Scholar indexed journals antirheumatic drugs articles antirheumatic drugs Research articles antirheumatic drugs review articles antirheumatic drugs PubMed articles antirheumatic drugs PubMed Central articles antirheumatic drugs 2023 articles antirheumatic drugs 2024 articles antirheumatic drugs Scopus articles antirheumatic drugs impact factor journals antirheumatic drugs Scopus journals antirheumatic drugs PubMed journals antirheumatic drugs medical journals antirheumatic drugs free journals antirheumatic drugs best journals antirheumatic drugs top journals antirheumatic drugs free medical journals antirheumatic drugs famous journals antirheumatic drugs Google Scholar indexed journals joint pain articles joint pain Research articles joint pain review articles joint pain PubMed articles joint pain PubMed Central articles joint pain 2023 articles joint pain 2024 articles joint pain Scopus articles joint pain impact factor journals joint pain Scopus journals joint pain PubMed journals joint pain medical journals joint pain free journals joint pain best journals joint pain top journals joint pain free medical journals joint pain famous journals joint pain Google Scholar indexed journals
Article Details
1. Introduction
Rheumatoid arthritis (RA) is a lifelong immune-mediated inflammatory disease characterized by synovial inflammation causing a symmetrical, polyarticular arthritis, which leads to cartilage damage and joint destruction [1]. The prevalence of RA worldwide is approximately 1%, with an apparent reduction from north to south (in the northern hemisphere) and from urban to rural areas [2]. Treatment of RA includes three different classes of medications: conventional synthetic (cs) disease-modifying antirheumatic drugs (DMARDs) such as methotrexate (MTX), sulfasalazine (SSZ), and hydroxychloroquine; biological (b) DMARDs; and targeted synthetic (ts) DMARDs [3]. Corticosteroids are used in low doses to control inflammation as “bridge therapy” when starting DMARDs until DMARDs become effective or to treat sudden flares of joint pain.
2. Case Report
A 71-year-old woman has been using corticosteroids since the age of 25, after she was first diagnosed with rheumatoid arthritis. She was living in a rural, isolated area. Since then, she was controlling the pain on her own using methylprednisolone tablets. After a fall, she was unable to walk and has been admitted to the rheumatology department for severe back pain. A computed tomography (CT)-scan of the spine revealed multiple compression fractures at the level of C7, T8 and L5. Interestingly, despite the obvious bone deformities during the physical examination in both elbows, wrists and fingers (Figure 1), she denied any pain in these joints while she was able to move them. Radiologic evaluation of the hands and elbows revealed catastrophic lesions (Figures 2). Moreover, the CT-scan of the left elbow showed a completely destroyed joint with many intra-articular free bodies (Figure 3). Long-term corticosteroid use can bring on catastrophic results in bone structures and patients must be properly informed regarding the side effects [4]. This patient developed side effects on conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), and finally she was treated with an anti-tumor necrosis factor agent [5].

Figure 1: Bone deformities in both elbows, wrists and fingers.
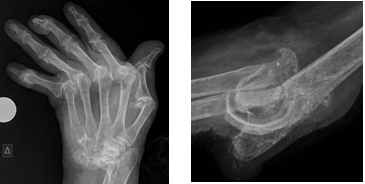
Figure 2: Radiologic evaluation of the hands and elbows.

Figure 3: CT-scan of the left elbow.
3. Discussion
RA is the most common autoimmune inflammatory arthritis in adults and has a negative impact on the ability to perform activities on a daily basis. In the last few years, significant advances have been made in our understanding of the molecular mechanisms underlying RA pathogenesis. Thus, better and more effective treatments and strategies are constantly being added to the clinician’s armamentarium in order to combat the knotty disease progression. Treat-to-target and tight control strategies are currently recommended in order to avoid cases such as the one presented above.
References
- Pelechas E, Voulgari PV, Drosos AA. Sirukumab: a promising therapy for rheumatoid arthritis. Expert Opin Biol Ther 17 (2017): 755-763.
- Alamanos Y, Voulgari PV, Drosos AA. Incidence and prevalence of rheumatoid arthritis, based on the 1987 American College of Rheumatology criteria: a systematic review. Semin Arthritis Rheum 36 (2006): 182-188.
- Singh JA, Saag KG, Bridges SL, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 68 (2016): 1-25.
- Mullen MB, Saag KG. Evaluating and mitigating fracture risk in established rheumatoid arthritis. Best Pract Res Clin Rheumatol 29 (2015): 614-627.
- Wu C, Wang S, Xian P, et al. Effect of Anti-TNF Antibodies on Clinical Response in Rheumatoid Arthritis Patients: A Meta-Analysis. Biomed Res Int 2016 (2016): 7185708.
