Contraceptive Uptake among Adolescent Girls Attending Family Planning Units in Four Health Facilities in Cameroon
Article Information
Frankline Sevidzem Wirsiy1*, Eugene Vernyuy Yeika2
1Department of Public Health and Hygiene, University of Buea, Buea, Cameroon
2Bangangte District Hospital, Bangangte, Cameroon,
*Corresponding Author: Frankline Sevidzem Wirsiy, Department of Public Health and Hygiene, Faculty of Health Sciences, University of Buea, P.O. Box 63-Buea, Cameroon
Received: 03 June 2019; Accepted: 14 June 2019; Published: 17 June 2019
Citation:
Frankline Sevidzem Wirsiy, Eugene Vernyuy Yeika. Contraceptive Uptake among Adolescent Girls Attending Family Planning Units in Four Health Facilities in Cameroon. Journal of Women’s Health and Development 2 (2019): 048-057.
Share at FacebookAbstract
Background and aim: In Africa and particularly in Cameroon, a substantial number of adolescent girls experience the negative health consequences as a result of not using contraceptives. The aim of this study was to determine contraceptive uptake among adolescent girls; specifically, to determine the principal trends in contraceptive use from 2012-2017 in the family planning units of four health facilities in the Kumbo West Health District of Cameroon and to identify the effect of age, marital status and parity on the choice of contraceptive method.
Methods: A retrospective record of 886 adolescent girls who attended the family planning and general gynaecology outpatient departments units of the four health facilities were reviewed for the period between the years 2012-2017. Data analyzed with SPSS version 21. Pearson chi-square test was used as a test of significance and P value <0.05 was considered statistically significant.
Results: Within the study period, the contraceptive uptake was 10.7%. IUD was the most commonly used method of contraception (27.4%), followed by the progestogen only injectable contraceptives (26.3%), then vacuum aspiration (4.2%) and implants (3.2%). Late adolescents, married adolescents and adolescent mothers were more likely to use contraceptives than early adolescents, single adolescents and those with 0 parity. IUD and jadelle uptake were not statistically significant with age, parity and marital status (P>0.05). However, Progestin injection uptake was statistically significant with parity (P=0.011).
Conclusions: Contraceptive uptake is relatively low among the adolescent girls. There is a need to improve access, availability and delivery of family planning services in Cameroon.
Keywords
Contraception, Uptake, Adolescent girls, Kumbo, Cameroon
Contraception articles Contraception Research articles Contraception review articles Contraception PubMed articles Contraception PubMed Central articles Contraception 2023 articles Contraception 2024 articles Contraception Scopus articles Contraception impact factor journals Contraception Scopus journals Contraception PubMed journals Contraception medical journals Contraception free journals Contraception best journals Contraception top journals Contraception free medical journals Contraception famous journals Contraception Google Scholar indexed journals Uptake articles Uptake Research articles Uptake review articles Uptake PubMed articles Uptake PubMed Central articles Uptake 2023 articles Uptake 2024 articles Uptake Scopus articles Uptake impact factor journals Uptake Scopus journals Uptake PubMed journals Uptake medical journals Uptake free journals Uptake best journals Uptake top journals Uptake free medical journals Uptake famous journals Uptake Google Scholar indexed journals Adolescent girls articles Adolescent girls Research articles Adolescent girls review articles Adolescent girls PubMed articles Adolescent girls PubMed Central articles Adolescent girls 2023 articles Adolescent girls 2024 articles Adolescent girls Scopus articles Adolescent girls impact factor journals Adolescent girls Scopus journals Adolescent girls PubMed journals Adolescent girls medical journals Adolescent girls free journals Adolescent girls best journals Adolescent girls top journals Adolescent girls free medical journals Adolescent girls famous journals Adolescent girls Google Scholar indexed journals Kumbo articles Kumbo Research articles Kumbo review articles Kumbo PubMed articles Kumbo PubMed Central articles Kumbo 2023 articles Kumbo 2024 articles Kumbo Scopus articles Kumbo impact factor journals Kumbo Scopus journals Kumbo PubMed journals Kumbo medical journals Kumbo free journals Kumbo best journals Kumbo top journals Kumbo free medical journals Kumbo famous journals Kumbo Google Scholar indexed journals Cameroon articles Cameroon Research articles Cameroon review articles Cameroon PubMed articles Cameroon PubMed Central articles Cameroon 2023 articles Cameroon 2024 articles Cameroon Scopus articles Cameroon impact factor journals Cameroon Scopus journals Cameroon PubMed journals Cameroon medical journals Cameroon free journals Cameroon best journals Cameroon top journals Cameroon free medical journals Cameroon famous journals Cameroon Google Scholar indexed journals reproductive† articles reproductive† Research articles reproductive† review articles reproductive† PubMed articles reproductive† PubMed Central articles reproductive† 2023 articles reproductive† 2024 articles reproductive† Scopus articles reproductive† impact factor journals reproductive† Scopus journals reproductive† PubMed journals reproductive† medical journals reproductive† free journals reproductive† best journals reproductive† top journals reproductive† free medical journals reproductive† famous journals reproductive† Google Scholar indexed journals health services articles health services Research articles health services review articles health services PubMed articles health services PubMed Central articles health services 2023 articles health services 2024 articles health services Scopus articles health services impact factor journals health services Scopus journals health services PubMed journals health services medical journals health services free journals health services best journals health services top journals health services free medical journals health services famous journals health services Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals retrospective articles retrospective Research articles retrospective review articles retrospective PubMed articles retrospective PubMed Central articles retrospective 2023 articles retrospective 2024 articles retrospective Scopus articles retrospective impact factor journals retrospective Scopus journals retrospective PubMed journals retrospective medical journals retrospective free journals retrospective best journals retrospective top journals retrospective free medical journals retrospective famous journals retrospective Google Scholar indexed journals electronic articles electronic Research articles electronic review articles electronic PubMed articles electronic PubMed Central articles electronic 2023 articles electronic 2024 articles electronic Scopus articles electronic impact factor journals electronic Scopus journals electronic PubMed journals electronic medical journals electronic free journals electronic best journals electronic top journals electronic free medical journals electronic famous journals electronic Google Scholar indexed journals
Article Details
1. Introduction
The World Health Organization (WHO) reports that, 214 million women of reproductive age, including adolescent girls in developing countries who want to avoid pregnancy are not using a modern contraceptive method [1]. Also, it has been reported that about half of all pregnancies among adolescent females in developing regions are estimated to be unintended, and more than half of these unintended pregnancies result in induced, and often unsafe, abortion [2, 3]. In addition, unprotected sexual intercourse that can lead to unintended pregnancy exposes adolescents to the risk of sexually transmitted infections, including HIV, which is currently a large contributor to the overall disease burden among adolescents in Sub-Saharan Africa including Cameroon [4-6]. It is in this light that an improvement in the access to the use of contraceptives needs to be a key component of an overall strategy to prevention of risky adolescent pregnancies in our societies. Amidst increasing calls to prioritize adolescents’ girls contraceptive needs, understanding current patterns of adolescent FP service use is important to achieving universal access to sexo-reproductive health services [6]. Misconceptions about how contraception works, sociocultural and religious factors are frequently cited as reasons for not using a method among adolescent girls [4, 5]. It is worthy to note that, appropriate health education and counseling is important to addressing knowledge gaps around pregnancy prevention and consistent contraceptive use among adolescent girls.
However, adolescent girls encounter enormous barriers to accessing quality reproductive health care [1, 4-6], including health provider bias, age stigmatization or restrictions when seeking FP services, and issues about confidentiality, judgmental/intrusive attitudes of health workers towards the adolescents [5]. WHO guidelines re-iterated the improvement of adolescent health services [7], and interventions to make health services “youth friendly” have appeared in several small-scale initiatives, primarily led by nongovernmental organizations (NGOs) as well as government-run health facilities [7]. Much of the evidence on young people’s contraceptive uptake in sub-Saharan Africa comes from small-scale, often qualitative studies which are not nationally representative [1]. The private sector is an important source of FP care in the region for women of all ages [8], suggesting that public-sector efforts expanding youth-friendly services may miss a significant proportion of young people accessing private providers [8].
Maternal mortality can only occur in the presence of a pregnancy [9]. Family planning is therefore an indispensable tool in reducing maternal mortality and morbidity [10]. Contraceptive uptake is one of the most pertinent associative factors of pregnancy/birth rates in the world, so contraceptive profiles provide useful information for policy makers [1]. The aim of this study was to determine contraceptive uptake among adolescent girls; specifically, to determine the principal trends in contraceptive use from 2012-2017 in the family planning units of four health facilities in the Kumbo West Health District of Cameroon and to identify the effect of age, marital status and parity on the choice of contraceptive method.
2. Materials and Methods
2.1 Study design
This was a retrospective chart review. A retrospective record of 886 adolescent girls who attended the family planning and general gynaecology outpatient departments units of the four health facilities were reviewed for the period between the years 2012-2017. Information about age, marital status, parity and choice of contraception were extracted using a structured proforma.
2.2 Study area
This study was specifically carried out in four randomly selected health facilities of the Kumbo West Health District namely Banso Baptist Hospital, Kitiwum Integrated Health Centre, Kumbo_Urban Medicalised Health Centre and Melim Integrated Health Centre. Kumbo is the second-largest city in the North West region of Cameroon. Kumbo is split into three distinctive hilly settlements of Tobin, Mbveh, and Squares. Figure 1 shows the Health Map of the Kumbo-West Health District of Cameroon.

Figure 1: Health Map of the Kumbo-West Health District (KWHD).
2.3 Data management
Research structured forms and other study materials were stored safely in a locker in a safe location and secured by locking it with a lock. After collection of the data, the forms were checked visually for completeness, obvious errors, and inconsistencies and then corrected. Data collected was entered daily into an electronic questionnaire (template) created in Epi info version 7 by the investigator. During the data entry process, 10% of data entered at the beginning was checked to ensure that the data was correctly entered. For confidentiality, the computer in which the data was stored was password protected and the information was accessible only to the researcher. Data was backed-up in an external hard drive and email box. The data was then imported into Microsoft excel spreadsheet for cleaning/editing.
2.4 Data analysis
Analysis was done with respect to contraceptive prevalence use over the years of study. The influence of age, parity and marital status was considered on the choice and patterns of contraceptive use. Data was analyzed with social science package statistical software (SPSS) version 21, Pearson Chi-square test was used as test of significance where applicable and a P value <0.05 was considered statistically significant.
2.5 Ethical and administrative considerations
Ethical approval was obtained from the Institutional Review Board of the Faculty of Health Sciences (IRB-FHS No: 765-03) of the University of Buea. The administrative approval was obtained from the managers of the various health facilities and the from Regional Delegate of Public Health for the North West Region of Cameroon.
3. Results
3.1 Uptake of contraceptive methods
We obtained data from four health facilities that is Banso Baptist Hospital, Kitiwum Integrated Health Centre, Kumbo_Urban Medicalised Health Centre and Melim Integrated Health Centre in the Kumbo West Health District-KWHD of Cameroon. It is worthy to note that in the health facilities, incomplete records on family planning (FP) especially for adolescents were observed. We didn’t include records that were incomplete. Due to illegal health care practice, we found that some of these health facilities actually had active family planning units across the years but when they administered FP to the adolescent girls, it was not registered in the hospital records as money was collected at individual levels (Private practice schemes). Such acts impede the health systems functioning and obviously affects the quality of data. Within the study period (2012-2017), 95 adolescent girls visited and obtained various forms of contraceptives from the Family planning units while a total of 886 adolescent girls visited the general gynaecology outpatient departments; giving a contraceptive uptake of 10.7% (Figure 2). The available modern methods of contraception at the centers were: Intrauterine Contraceptive Device (IUD) insertion, jadelle insertions, Progestin injections, Pills, implants, manual vacuum aspiration and condoms.
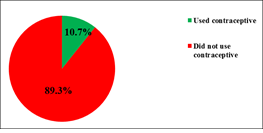
Figure 2: Uptake of contraceptives among adolescent girls visiting the family planning units, Kumbo West Health District, 2012-2017.
3.2 Contraceptive options and uptake from family planning unit
Table 1 shows the frequency of the various contraceptive methods obtained at the health facility over the study period. Twenty-six (27.4%) of the clients opted for Intrauterine Device (IUD) followed by the progestin injections (26.3%). Less popular were implants (3.2%) and manual vacuum aspiration (4.2%).
|
Contraceptives |
Frequency |
Percentage (%) |
|
Condoms |
6 |
6.3 |
|
IUD insertions |
26 |
27.4 |
|
Implants |
3 |
3.2 |
|
Progestin injections |
25 |
26.3 |
|
Jadelle insertion |
21 |
22.1 |
|
Pills |
10 |
10.5 |
|
Manual vacuum aspirator |
4 |
4.2 |
Table 1: Contraceptive options and uptake, Kumbo West Health District 2019.
3.3 Variation of contraceptive uptake with sociodemographic factors
Table 2 shows a summary of variation of contraceptive uptake with sociodemographic factors over five years (2012-2017) retrospectively. From the table, we can see that Banso Baptist Hospital got the highest number of adolescent girls who obtained contraception that is 85 (89.5%). This was due to the fact that, at the Kumbo West Health District, there was only one trained midwife specialized in administering FP to women. This contributed in many young women visiting the hospital for her services. Also, it shows that majority of those who obtained contraceptive were single and having a parity status that is 60.0% and 53.7% respectively.
|
Characteristic |
Frequency |
Percentage (%) |
|
Age (years) |
16.04 ± 2.2 (Mean ± SD) |
10-19 (Range) |
|
10-14 |
9 |
9.5 |
|
15-19 |
86 |
90.5 |
|
Marital status |
||
|
Single |
57 |
60.0 |
|
Married |
38 |
40.0 |
|
Parity |
||
|
0 |
51 |
53.7 |
|
≥ 1 |
44 |
46.3 |
|
Health area |
||
|
BBH |
85 |
89.5 |
|
Kitiwum |
1 |
1.1 |
|
Kumbo Urban |
8 |
8.4 |
|
Melim |
1 |
1.1 |
|
Year |
||
|
2012 |
22 |
23.2 |
|
2013 |
3 |
3.2 |
|
2014 |
1 |
1.0 |
|
2015 |
6 |
6.3 |
|
2016 |
22 |
23.2 |
|
2017 |
41 |
43.2 |
Table 2: Variation of contraceptive uptake with sociodemographic factors.
3.4 Variation of IUD, Jadelle and Progestin injection uptake by age, parity and marital status
Table 3, 4 and 5 shows the variation of IUD, Jadelle and Progestin injection uptake by age, parity and marital status. Table 3 and 4 indicates that IUD and jadelle uptake were not statistically significant with age, parity and marital status. However, Progestin injection uptake was statistically significant with parity as shown in Table 5.
|
Category |
IUD uptake: n (%) |
χ 2 |
p-value |
|
|
Yes |
No |
|||
|
By age (in years) |
||||
|
10 - 14 |
3 (33.3) |
6 (66.7) |
0.178 |
0.673 |
|
15 - 19 |
23 (26.7) |
63 (73.3) |
||
|
By parity |
||||
|
0 |
15 (29.4) |
36 (75.0) |
0.231 |
0.548 |
|
≥ 1 |
11 (25.0) |
33 (75.0) |
||
|
Marital status |
||||
|
Married |
10 (26.3) |
28 (73.7) |
0.035 |
0.851 |
|
Single |
16 (28.1) |
41 (71.9) |
||
Table 3: Variation of IUD uptake by age, parity and marital status, KWHD 2012-2017.
|
Category |
Jadelle uptake: n (%) |
χ 2 |
p-value |
|
|
Yes |
No |
|||
|
By age (in years) |
||||
|
10 - 14 |
2 (22.2) |
7 (77.8) |
0.001 |
0.993 |
|
15 - 19 |
19 (22.1) |
67 (77.9) |
||
|
By parity |
||||
|
0 |
12 (23.5) |
39 (76.5) |
0.130 |
0.719 |
|
≥ 1 |
9 (20.5) |
35 (79.5) |
||
|
Marital status |
||||
|
Married |
9(23.7) |
29 (76.3) |
0.092 |
0.76 |
|
Single |
12 (21.1) |
45 (78.9) |
||
Table 4: Variation of Jadelle insertion uptake by age, parity and marital status, KWHD 2012-2017.
|
Category |
Progestin uptake: n (%) |
χ 2 |
p-value |
|
|
Yes |
No |
|||
|
By age (in years) |
||||
|
10 - 14 |
3 (33.3) |
6 (66.7) |
0.252 |
0.615 |
|
15 - 19 |
22 (25.6) |
64 (74.4) |
||
|
By parity |
||||
|
0 |
8 (15.7) |
43 (84.3) |
6.416 |
0.011 |
|
≥ 1 |
17 (38.6) |
27 (61.4) |
||
|
Marital status |
||||
|
Married |
10 (26.3) |
28 (73.7) |
0.000 |
1.000 |
|
Single |
15 (26.3) |
42 (73.7) |
||
Table 5: Variation of Progestin injection uptake by age, parity and marital status, KWHD 2012-2017.
4. Discussion
4.1 Contraceptive uptake and its stakes
A contraceptive uptake of 10.7% among adolescent girls shows that uptake is low. This phenomena of low contraception uptake among adolescents had been reported by Ann et al. [11] of the Guttmacher Institute that a great proportion of adolescent girls than older women discontinued using a contraceptive method within a year or experienced contraceptive failure. In the samelight, contraceptive uptake is relatively low among the married (40%) compared to the single (60%). This may be due to the fact that married adolescents are less likely to source for contraception openly because of cultural and religious factors in this part of Cameroon [4]. It has been reported by Chandra et al. [12] that sexually active adolescents whether married/unmarried need contraception. Many adolescents in Low middle income countries face significant barriers in obtaining contraception as well as using them consistently and correctly [1].
4.2 Adolescent girls face significant barriers to accessing contraception
According to WHO 2018 [13], adolescent girls face significant barriers in accessing contraception including health worker bias and/or lack of willingness to acknowledge adolescent girls’ sexo-reproductive health needs, restrictive laws/policies regarding provision of contraceptive based on age or marital status, and adolescent girls’ own inability to access contraceptives because of knowledge, transportation, and financial constraints. Additionally, adolescent girls face barriers that prevent use and/or consistent and correct use of contraception, even when they are able to obtain contraceptives: stigma surrounding non-marital sexual affairs and/or contraceptive use; fear of side effects; lack of knowledge on correct use; and factors contributing to discontinuation (for example, laxity to go back and seek contraceptives because of negative first experiences with health care providers, changing reproductive needs, changing reproductive intentions) [5, 6].
4.3 Sexual debut and contraception
Though the sexual activity of adolescents (ages 10-19) varies markedly for boys versus girls and by countries, a significant number of adolescents are sexually active; such that other studies have reported sexual activity increases steadily from mid-to-late adolescence [6, 14]. This is reflected in the study as only 9.5% of early adolescents visited the family planning unit for contraception, an indication for sexual debut compared to late adolescents (90.5%).
4.4 Available contraceptive methods
From the available contraceptive methods, IUD was the most popular choice accounting for 27.4% of the clients, followed by the injectables (26.3%), then the jadelle insertions (22.1%) and pills (10.5%). Less popular were Condoms, manual vacuum aspirator and implants (6.3%, 4.2% and 3.2%). This may probably reflect the relative availability of each method and cost variations. Adolescent girls in Africa including Cameroon have an unmet need for contraception, which can contribute to poor reproductive health outcomes as reported by Wirsiy et al. [6] and Gottschalk and Ortayli [15].
5. Conclusion
It is worthy to re-iterate that, adolescent girl’s fertility regulation and pregnancy prevention is an important health-care issue of the twenty-first century. Significant numbers of adolescent girls experience the negative health consequences of early unintended pregnancy, unsafe abortions, unprotected sexual activity, pregnancy-related mortality and morbidity and Sexually Transmitted Infections; including its social and economic costs. Enhancing access to and use of contraceptives needs to be a key component of an overall strategy to preventing adolescent pregnancy. Effective and sustainable interventions to improve access and use of contraception include building community support for the provision of contraception to adolescent girls, providing sexo-reproductive health education within and outside school settings, enacting/implementing laws and policies requiring the provision of sexo-reproductive health education and contraceptive services for adolescent girls, integrating family planning services with other health services, and providing contraception through a variety of outlets and increasing the access to and use of contraception by making the health services adolescent-friendly. Emerging data on sexo-reproductive health suggest mobile phones as well as social media are promising means of increasing contraception uptake among adolescent girls. Also, family planning is a veritable tool in the efforts geared at improving maternal health, reducing maternal and under-five mortality. To reach these goals, there is a need to improve access, availability and delivery of family planning services across the nation especially for all adolescent girls in their reproductive age group and their partners.
Acknowledgements
This is part of my Ph.D. thesis in Public Health in the Department of Public Health and Hygiene of the University of Buea. I acknowledge all stakeholders including my supervisors, the District Medical Officer of Kumbo West Health District, Regional Delegate for Public Health-North West Region, Chief of Health Centres, Community leaders and colleagues for their contributions in the realisation of this study.
Authors’ contributions
FSW as Principal Investigator, designed and executed the research study. FSW and EVY analysed and interpreted the data. FSW and EVY wrote the manuscript, reviewed and approved the final manuscript.
Funding
No funding for the study was available.
Disclaimer
The views expressed are those of the authors.
Competing Interests
The authors declare no conflicts of interest.
Ethics Approval
The study was approved by the Institutional Review Board of the Faculty of Health Sciences, Buea in Cameroon under study number 765-03.
References
- World Health Organization (WHO). Family planning/Contraception (2019).
- Biddlecom A, Riley T, Darroch JE, et al. Future Scenarios of Adolescent Contraceptive Use, Cost and Impact in Developing Regions. Guttmacher Institute (2018).
- Wirsiy FS, Nsagha DS, Njajou OT, et al. Prevalence and Associated Risk Factors of HIV among Pregnant Adolescents and Adolescent Mothers in the Kumbo West Health District of Cameroon. Journal of Infectious Diseases and Epidemiology 5 (2019): 10.
- Wirsiy FS, Nsagha DS, Njajou OT, et al. Determinants of Reproductive Health Needs of Adolescent Girls in Africa. African Journal of Integrated Health 8 (2018): 7.
- Wirsiy FS, Nsagha DS, Njajou OT, et al. Determinants of Sexo-Reproductive Health Needs of Adolescent Girls in the Kumbo West Health District of Cameroon. Journal of Environmental Science and Public Health 3 (2019): 28.
- Wirsiy FS, Nsagha DS, Njajou OT, et al. A Qualitative Analysis of Predictors of Sexo-Reproductive Health Needs of Adolescent Girls in the Kumbo West Health District of Cameroon. Journal of Environmental Science and Public Health 3 (2019): 24.
- World Health Organisation (WHO). Engaging young people in their own care is key to improving adolescent health (2017).
- Chakraborty NM, Sprockett A. Use of family planning and child health services in the private sector: an equity analysis of 12 DHS surveys. International Journal of Equity Health 2 (2018): 17-18.
- World Health Organisation (WHO). Maternal health (2019).
- Chola L, McGee S, Tugendhaft A, et al. Scaling Up Family Planning to Reduce Maternal and Child Mortality: The Potential Costs and Benefits of Modern Contraceptive Use in South Africa. PLoS ONE 10 (2015).
- Ann K, Amy O, Trevor N, et al. Patterns and Trends in Adolescents’ Contraceptive Use and Discontinuation in Developing Countries and Comparisons With Adult Women. Guttmacher Institute 35 (2009).
- Chandra-MV, McCarraher DR, Phillips SJ, et al. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health 11 (2014): 1.
- World Health Organisation (WHO). Adolescent pregnancy (2018).
- Salam RA, Faqqah A, Sajjad N, et al. Improving Adolescent Sexual and Reproductive Health: A Systematic Review of Potential Interventions. Journal of Adolescent Health 59 (2016): 11-28.
- Gottschalk LB, Ortayli N. Interventions to improve adolescents’ contraceptive behaviors in low- and middle-income countries: a review of the evidence base. Contraception 90 (2014): 211-225.
