Continuous Mechanical External Compression for Dural Leaks after Lumbar Spine Surgery by Stitching Pads to the Wound, A Conservative Treatment. Report of Two Cases
Article Information
Luis Díez-Albero1, María Tíscar García-Ortiz1, Miguel Bañuls-Pattarelli1*, Robert C Mulholland2, Fernando López-Prats1, 3
1Department of Orthopedics and Trauma, Elche University General Hospital, Elche, Spain
2Spinal Unit, Nottingham University Hospitals NHS, Nottingham, United Kingdom
3Department of Orthopaedics and Trauma, Miguel-Hernández University, San Juan de Alicante, Spain
*Corresponding Author: Miguel Bañuls-Pattarelli, Department of Orthopedics and Trauma, Elche University General Hospital, Carrer Almazara 11, 03203. Elche (Alicante), Spain
Received: 22 September 2021; Accepted: 29 September 2021; Published: 09 October 2021
Citation:
Luis Díez-Albero, María Tíscar García-Ortiz, Miguel Bañuls-Pattarelli, Robert C Mulholland, Fernando López-Prats. Continuous Mechanical External Compression for Dural Leaks after Lumbar Spine Surgery by Stitching Pads to the Wound, A Conservative Treatment. Report of Two Cases. Journal of Spine Research and Surgery 3 (2021): 106-112.
Share at FacebookAbstract
Purpose: Description of a non-operative technique for the repair of cerebrospinal (CSF) dural leaks after lumbar spine surgery.
Methods: Two patients, thirty-nine and seventy-six years old respectively, were previously operated of lum- bar discectomy/decompression, and in the following days developed leakage of clear CSF fluid in their surgical wounds. They were treated by means of stitched pads to their wounds, creating continuous external compression reducing the dead space for the CSF to get in.
Results: After, one and two weeks respectively and no evidence of leakage the sutures were removed. The patients were reviewed at 3 and 6-months post operation, where no clinical evidence of dural leaks was found and in one the MRI confirm their absence. At the end, the patients were asymptomatic of their original lumbar complaint.
Conclusion: An alternative simple technique that avoids the necessity of reoperation in the case of post-operative dural tears.
Keywords
CSF Dural Leaks, Dural Tears, Pseudo-Meningocele, Continuous Bed Rest, Surgical Wound, Stitching Pads, Continuous External Compression
CSF Dural Leaks articles CSF Dural Leaks Research articles CSF Dural Leaks review articles CSF Dural Leaks PubMed articles CSF Dural Leaks PubMed Central articles CSF Dural Leaks 2023 articles CSF Dural Leaks 2024 articles CSF Dural Leaks Scopus articles CSF Dural Leaks impact factor journals CSF Dural Leaks Scopus journals CSF Dural Leaks PubMed journals CSF Dural Leaks medical journals CSF Dural Leaks free journals CSF Dural Leaks best journals CSF Dural Leaks top journals CSF Dural Leaks free medical journals CSF Dural Leaks famous journals CSF Dural Leaks Google Scholar indexed journals Dural Tears articles Dural Tears Research articles Dural Tears review articles Dural Tears PubMed articles Dural Tears PubMed Central articles Dural Tears 2023 articles Dural Tears 2024 articles Dural Tears Scopus articles Dural Tears impact factor journals Dural Tears Scopus journals Dural Tears PubMed journals Dural Tears medical journals Dural Tears free journals Dural Tears best journals Dural Tears top journals Dural Tears free medical journals Dural Tears famous journals Dural Tears Google Scholar indexed journals Pseudo-Meningocele articles Pseudo-Meningocele Research articles Pseudo-Meningocele review articles Pseudo-Meningocele PubMed articles Pseudo-Meningocele PubMed Central articles Pseudo-Meningocele 2023 articles Pseudo-Meningocele 2024 articles Pseudo-Meningocele Scopus articles Pseudo-Meningocele impact factor journals Pseudo-Meningocele Scopus journals Pseudo-Meningocele PubMed journals Pseudo-Meningocele medical journals Pseudo-Meningocele free journals Pseudo-Meningocele best journals Pseudo-Meningocele top journals Pseudo-Meningocele free medical journals Pseudo-Meningocele famous journals Pseudo-Meningocele Google Scholar indexed journals Continuous Bed Rest articles Continuous Bed Rest Research articles Continuous Bed Rest review articles Continuous Bed Rest PubMed articles Continuous Bed Rest PubMed Central articles Continuous Bed Rest 2023 articles Continuous Bed Rest 2024 articles Continuous Bed Rest Scopus articles Continuous Bed Rest impact factor journals Continuous Bed Rest Scopus journals Continuous Bed Rest PubMed journals Continuous Bed Rest medical journals Continuous Bed Rest free journals Continuous Bed Rest best journals Continuous Bed Rest top journals Continuous Bed Rest free medical journals Continuous Bed Rest famous journals Continuous Bed Rest Google Scholar indexed journals Surgical Wound articles Surgical Wound Research articles Surgical Wound review articles Surgical Wound PubMed articles Surgical Wound PubMed Central articles Surgical Wound 2023 articles Surgical Wound 2024 articles Surgical Wound Scopus articles Surgical Wound impact factor journals Surgical Wound Scopus journals Surgical Wound PubMed journals Surgical Wound medical journals Surgical Wound free journals Surgical Wound best journals Surgical Wound top journals Surgical Wound free medical journals Surgical Wound famous journals Surgical Wound Google Scholar indexed journals Stitching Pads articles Stitching Pads Research articles Stitching Pads review articles Stitching Pads PubMed articles Stitching Pads PubMed Central articles Stitching Pads 2023 articles Stitching Pads 2024 articles Stitching Pads Scopus articles Stitching Pads impact factor journals Stitching Pads Scopus journals Stitching Pads PubMed journals Stitching Pads medical journals Stitching Pads free journals Stitching Pads best journals Stitching Pads top journals Stitching Pads free medical journals Stitching Pads famous journals Stitching Pads Google Scholar indexed journals Continuous External Compression articles Continuous External Compression Research articles Continuous External Compression review articles Continuous External Compression PubMed articles Continuous External Compression PubMed Central articles Continuous External Compression 2023 articles Continuous External Compression 2024 articles Continuous External Compression Scopus articles Continuous External Compression impact factor journals Continuous External Compression Scopus journals Continuous External Compression PubMed journals Continuous External Compression medical journals Continuous External Compression free journals Continuous External Compression best journals Continuous External Compression top journals Continuous External Compression free medical journals Continuous External Compression famous journals Continuous External Compression Google Scholar indexed journals cerebrospinal fluid articles cerebrospinal fluid Research articles cerebrospinal fluid review articles cerebrospinal fluid PubMed articles cerebrospinal fluid PubMed Central articles cerebrospinal fluid 2023 articles cerebrospinal fluid 2024 articles cerebrospinal fluid Scopus articles cerebrospinal fluid impact factor journals cerebrospinal fluid Scopus journals cerebrospinal fluid PubMed journals cerebrospinal fluid medical journals cerebrospinal fluid free journals cerebrospinal fluid best journals cerebrospinal fluid top journals cerebrospinal fluid free medical journals cerebrospinal fluid famous journals cerebrospinal fluid Google Scholar indexed journals Charnley Sponges articles Charnley Sponges Research articles Charnley Sponges review articles Charnley Sponges PubMed articles Charnley Sponges PubMed Central articles Charnley Sponges 2023 articles Charnley Sponges 2024 articles Charnley Sponges Scopus articles Charnley Sponges impact factor journals Charnley Sponges Scopus journals Charnley Sponges PubMed journals Charnley Sponges medical journals Charnley Sponges free journals Charnley Sponges best journals Charnley Sponges top journals Charnley Sponges free medical journals Charnley Sponges famous journals Charnley Sponges Google Scholar indexed journals Orthopaedics articles Orthopaedics Research articles Orthopaedics review articles Orthopaedics PubMed articles Orthopaedics PubMed Central articles Orthopaedics 2023 articles Orthopaedics 2024 articles Orthopaedics Scopus articles Orthopaedics impact factor journals Orthopaedics Scopus journals Orthopaedics PubMed journals Orthopaedics medical journals Orthopaedics free journals Orthopaedics best journals Orthopaedics top journals Orthopaedics free medical journals Orthopaedics famous journals Orthopaedics Google Scholar indexed journals
Article Details
1. Introduction
Incidental duraltears and cerebrospinal fluid (CSF) leaks are one of the most common intraoperative complications inlumbarspine surgery [1-7]. In the case of awareness of a leak in the operating room, most surgeons recommend immediate repair. Tiny tears may often be missed and could manifest days or weeks after the operation. In those cases, there is controversy about conservative or surgical repair. Conservative treatment is mainly based on bed rest, local compression by padded dressings, sometimes in Trendelenburg position, periodical checking of the wound and antibiotic therapy to prevent infection [8, 9]. Others prefer different measures like blood patches or continuous aspiration [10]. Most spinal surgeons nowadays choose direct surgical repair [11]. However, for the patient means a new major operation, sometimes not very successful [12]. A dural leak will only causea problem ifthere is a dead space for the fluid to flow into.The use of a firm compression pad, enhanced by Charnley sponges or a gauze pad with a suture through the deep fascia to provide continuous firm pressure on the dressing after operation will closethe dead space and will prevent fluid escaping. We describe a simple surgical technique that consist of anchoring 4 to 6 stitches 2 cm parallel to each side of the surgical wound into the sub-fascial plane (Figure 1). Once anchored, tying the knots over a pad like a roll of gauze (Figure 2), will secure a stable continuous compression of the area of the leak. and close any dead space following a spinal procedure where a dural leak has occurred or it is suspected.
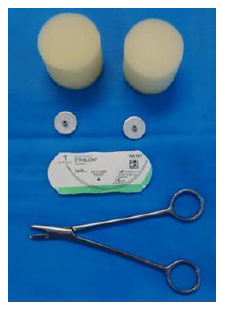
Figure 1: Charnley Sponges.
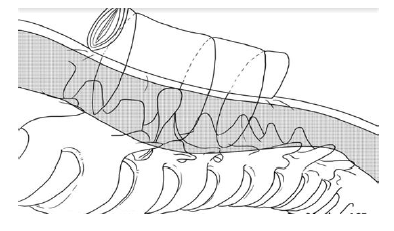
Figure 2: Demonstration of the technique: A gauze-roll of a 5cm diameter by 20 cm length gauze was attached to the skin by means of transcutaneous stitches inserted deep into the sub-facial plane, closing the dead space. Image courtesy of Elloboiberico.com.
2. Case Report
2.1 Case number 1
A thirty-nine-year-old woman who had had a partial laminectomy for a disc herniation two weeks previously presented to the Accident and Emergency department with a severe headache and clear fluid leaking from her surgical wound, identified as CSF. After admission to the Hospital, under local anaesthetic a firm gauze pad was placed onto the wound and firmly compressed using Charnley sponges with four deep sub-fascial nylon sutures (Figure 3). When assessed six hours after the procedure her headache has ceased and against nursing advice has walked herself out of bed. Following the above, the patient was in bedrest for three days. Then on the absence of CSF leakage, she was discharged home taken oral antibiotics with the stitched pressure dressing in place. At one week at the outpatient’s follow-up there was no clinical evidence of CSF leakage, then the deep sutures and the pads were removed. At three months follow-up there was no clinical evidence of CSF leakage or fluid collection around the area of the wound. The symptoms leading to her original laminectomy have ceased.
2.2 Case number 2
Three weeks after a two-level lumbar decompression, a seventy-six-year-old man presented himself at the Accident and Emergency department. He has developed a lump in the operated site that was by mistake treated as a hematoma by means of draining it by a small puncture with a scalpel. The drainage caused a permanent spontaneous leakage of CSF. The patient was then immediately admitted to hospital. At the time of admission, he had no temperature, no headache or any another neurological symptom. An MRI taken the next day showed a large fluid collection in the paravertebral soft tissues at L4-L5 and L5-S1 levels (Figure 4). The patient was placed in bed rest in supine position with local padded dressings in the site of the lump. After 4 days and in the view of no improvement, he was taken to the operating room. A roll of a 5cm diameter by 20 cm length gauze was attached to the skin by means of 6 mattress stitches inserted deep into the sub-fascial plane, closing the dead space. The following days, gradually the volume of the leakage reduced until the area became dry. At two weeks, the sutures were removed. By then the wound was healed with no evidence of palpable lump or CSF leakage. The patient was discharged home letting with no postural or mobility restrictions. Six months after, an MRI showed the disappearance of the CSF collection (Figure 5). The patient was again seen in the out-patients at 9 months without evidence of local fluid collection. By then his original symptoms were relieved without the need of reopening the operated site.
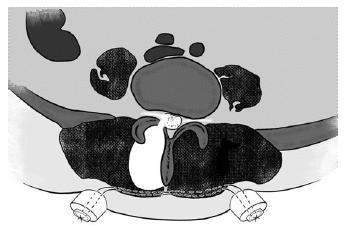
Figure 3: A firm gauze pad placed onto the wound and firmly compressed using Charnley sponges with four deep sub-fascial nylon sutures.
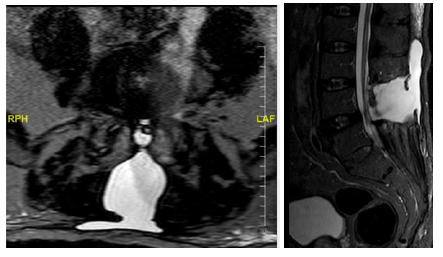
Figure 4a and 4b: Three weeks postoperative MRI. STIR and T2 weighted images obtained weeks after surgery showed abnormal fluid collection in paravertebral soft tissues at L4-L5 and L5-S1 levels.
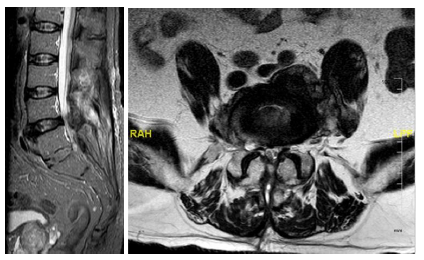
Figure 5a and 5b: MRI 6 months after the surgery. STIR and T2 weighted images at the same level obtained 6 months after surgery showed no evidence of cerebrospinal fluid leaks.
3. Discussion
When a dural leak is detected in the postoperative period, the primary option is non-operative postural treatment by means of continuous bedrest in supine position pressing onto a well-padded wound creating external compression. The above reduces the space filled by CSF, created between the dura and the wound, therefore avoiding leakage. However, it has the incon-venience that sometimes it is not always effective and bears the usual complications of continuous bed rest, such as pressure sores or increased risk of thromboem-bolic episodes [13]. Many patients do not tolerate a pro-longed static position and some of them do not comply. It is unrealistic to expect that bedrest alone, will main-tain the continuous pressure that allows a dural defect to heal, as patients naturally reposition themselves in the bed, and need to tend their necessities, even with high standard nursing care. If the above postural treatment fails, there is no consensus regarding the goal standard of care for this problem. There is yet to be established an algorithmic approach or a universally accepted method of treatment. Several treatments have been suggested in the literature such as epidural blood patches [14-16]. and continuous dural drainage [17].
Being the latest, not exempt from complications such as continuous headaches, infection such as meningitis, discitis, and wound infection, transient nerve root irritation, and recurrence [18-20]. The authors used the stitched pressure pads to avoid surgical repair, consider-ing that damage of the neural structures is much more common in revision procedures, usually because of adhesions in the epidural space and dural scarring and fibrosis [21]. The authors believe that using a stitched pad as described above, provides the continuous pressu-re needed for a dural defect to heal. Our experience with the two reported cases has highlighted the possibility to avoid re-operation in the treatment of post-operative dural leakages. Also,obliterating the dead space proph-ylactically after a procedure where there is a suspected tear or if one has been repaired is a valuable precaution. This concept of obliterating the dead space can be used when a leak declares itself days or even weeks after operation. Clearly the longer the dead space is present and dilated by fluid the efficacy of compression to reduce it becomes less as the walls become organized.
4. Conclusion
The authors conclude that stitching an external pad onto a wound that leaks CSF closes the dead space and favours the resolution of dural tears. The simplicity of the technique makes a good alternative with minimal intervention.
Declarations
Funding
Not applicable.
Conflicts of interest/Competing interests
We do not have any conflict of interest.
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
- Mazda F, Aichmair A, Wanivenhaus F, et al. No benefit of early versus late ambulation after incidental durotomy in lumbar spine surgery: a randomized controlled trial. Eur Spine J 29 (2020): 141-146.
- Cammisa FP Jr, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine 25 (2020): 2663-2667.
- Du JY, Aichmair A, Kueper J, et al. Incidental durotomy during spinal surgery: a multivariate analysis for risk factors. Spine 39 (2014): 1339-1345.
- Goodkin R, Laska LL. Unintended "incidental" durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol 43 (1995): 4-12.
- Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management, and complications. A retrospective review. Injury 43 (2012): 397-401.
- McMahon P, Dididze M, Levi AD. Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine 17 (2012): 30-36.
- Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J 14 (2005): 287-290.
- Waisman M, Schweppe Y. Postoperative cerebrospinal fluid leakage after lumbar spine operations. Conservative treatment. Spine 16 (1991): 52-53.
- Leis AA, Leis JM, Leis JR. Pseudom-eningoceles: a role for mechanical compression in the treatment of dural tears. Neurology 56 (2001): 1116-1117.
- Abouleish E, Vega S, Blendinger I, et al. Long-term follow-up of epidural blood patch. Anesth Analg 54 (1975): 459-463.
- Bosacco SJ, Gardner MJ, Guille JT. Evaluation and Treatment of Dural Tears in Lumbar Spine Surgery. Clin Orthop Relat Res 389 (2001): 238-247.
- Eismont FJ, Wiesel S, Rothman RH. Treatment of dural tears associated with spinal surgery. J Bone Joint Surg 63 (1981): 1132-1136.
- Ibarra-Cornejo JL, Fernandez-Lara MJ, Aguas- Alveal EV, et al. Efectos del reposo prolongado en adultos mayores hospitalizados. An Fac med 78 (2017): 439-444.
- Tubben RE, Jain S, Murphy P. Epidural Blood Patch. Treasure Island (FL): StatPearls Publishing (2021).
- Özütemiz C, Köksel YK, Huang H, et al. The efficacy of fluoroscopy-guided epidural blood patch in the treatment of spontaneous and iatrogenic cerebrospinal fluid leakage. Eur Radiol (2019).
- Levi V, Di Laurenzio NE, Franzini A, et al. Lumbar epidural blood patch: effectiveness on orthostatic headache and MRI predictive factors in 101 consecutive patients affected by spontaneous intracranial hypotension. J Neurosurg 132 (2019): 809-817.
- Bròdano GB, Serchi E, Babbi L, et al. Is lumbar drainage of postoperative cerebrospinal fluid fistula after spine surgery effective? J Neurorosurg Sci 58 (2014): 23-27.
- Couture D, Banch CI. Spinal pseudomen-ingoceles and cerebrospinal fluid fistulas. Neurosurg focus 15 (2003): 1-5.
- Takenaka S, Makino T, Sakai Y, et al. Prognostic impact of intra- and postoperative management of dural tear on postoperative complications in primary degenerative lumbar diseases. Bone Joint J 101 (2019): 1115-1121.
- Açikbas SC, Akyüz M, Kazan S, et al. Complications of Closed Continuous Lumbar Drainage of Cerebrospinal Fluid. Acta Neurochir 144 (2002): 475-480.
- Bosacco SJ, Gardner MJ, Guille JT. Evaluation and Treatment of Dural Tears in Lumbar Spine Surgery. A review. Clin Orthop Relat Res 389 (2001): 238-247.
