Comparing the Left Distal Transradial Artery Access to Traditional Access Methods For Coronary Angiography: A Single-Center Experience
Article Information
Maleeha Saleem*1, Steven A Hamilton1, Karan Pahuja2, Mohab Hassib2, Ahmed Elkhouly3, Muhammad Haseeb-ul-Rasool4, Justin Fox5
1Co-first authors - Resident physician, Internal medicine, Jersey Shore University Medical Center/Saint Francis Medical Center, Trenton, NJ, USA.
2Co-second authors- Resident physician, Internal medicine, Jersey Shore University Medical Center/Saint Francis Medical Center, Trenton, NJ, USA.
3Resident physician, Internal medicine, Jersey Shore University Medical Center/Saint Francis Medical Center, Trenton, NJ, USA.
4Resident physician, Internal Medicine, Icahn School of Medicine at Mount Sinai Queens Hospital Center, NY, USA
5Interventional Cardiologist, Medical Director, Hamilton Cardiology Associates’IAC Accredited Nuclear Cardiology Lab,Medical Director, Saint Francis Medical Center Chest Pain Center, Trenton, NJ, USA
*Corresponding author: Maleeha Saleem, Jersey Shore University Medical Center/ Saint francis Mediical Center, Trenton, New Jersey, USA
Received: 08 June 2022; Accepted: 16 June 2022; Published: 27 June 2022
Citation:
Maleeha Saleem, Steven A Hamilton, Karan Pahuja, Mohab Hassib, Ahmed Elkhouly, Muhammad Haseeb-ul-Rasool, Justin Fox. Comparing the Left Distal Transradial Artery Access to Traditional Access Methods For Coronary Angiography: A Single-Center Experience. Cardiology and Cardiovascular Medicine 6 (2022): 325-339.
Share at FacebookAbstract
Objective: The aim of this study was to compare the effectiveness and safety of left distal transradial (LdTRA) approach in patients who had prior coronary artery bypass grafting (CABG) with conventional femoral and radial access for coronary angiography. Background: The left distal transradial approach (LdTRA) is newer vascular access for coronary angiography. We hypothesized that LdTRA is superior to traditional femoral (TFA) and traditional right radial approaches for cardiac catheterization in patients who underwent prior bypass graft surgery (CABG).
Methods: We retrospectively evaluated 417 patients with prior CABG, undergoing coronary angiography at our institution between January 2018 and August 2020, to compare the type of intervention using site of access as the independent factor. We screened patients' charts using Xper IM. Analyses were performed by Statistical Product and Services Solution using Chi Square test and Pearson's correlation for categorical data and ANOVA test for nominal data, at a p value of <0.05. Predefined endpoints were time to access, procedure duration, mean length of hospital stay, fluoroscopy time and dose.
Results: The mean time for femoral access was 37.68±1.19 seconds (95% CI 35.3295-40.04), for LdTRA (snuffbox access) was 36.4±5.06 seconds (95% CI=26.03-46.81), and for proximal radial access was 40.71±4.17 seconds (95% CI=31.21-50.20).Mean procedural time via femoral access was 37.68±1.97 minutes, via snuffbox access was 36.43±5.06 minutes, and via radial access was 40.71±4.17 minutes. Mean length of stay for femoral access was 1.97±0.14 days, for radial access 2.13±0.31 days and for snuffbox access 1.68±0.27 days. The fluoroscopy time for femoral access was 10.23±0.41 minutes, for snuffbox access
Keywords
Snuffbox; coronary angiography; coronary artery bypass grafting; left distal radial artery; radial artery occlusion
Snuffbox; coronary angiography; coronary artery bypass grafting; left distal radial artery; radial artery occlusion articles
Article Details
1. Introduction
Percutaneous coronary intervention (PCI) is the recommended revascularization procedure for patients with acute coronary syndrome (ACS) [1]. Despite the advancements associated with the procedure, complications are known to occur and almost half of them are access site complications which can lead to prolonged hospital stay and increased mortality and morbidity [1]. CABG patients represent a subset of challenging coronary artery disease patients with multivessel disease, complex coronary anatomies [2], and high atherosclerotic disease burden in other arterial territories such as iliac and femoral arteries [3]. They tend to be older and have multiple comorbid conditions [4].
Minimizing the procedural risks while adequately cannulating the grafts remains a challenge [2]. For diagnostic angiography in general, transradial access (TRA) has increasingly become a more popular method than TFA and carries several advantages including faster mobilization [5], reduced access site bleeding complications [6], and greater patient comfort [7]. Nonetheless, TRA does come with some degree of risk including radial artery occlusion (RAO), increased radiation exposure [8], and, rarely, osteofascial compartment syndrome of the forearm [6]. Additionally, in patients with prior CABG, radial access is sometimes made more challenging due to the presence of IMA grafts, gastroepiploic artery grafts, and incidences where the radial artery had been harvested as a conduit [9].
After CABG, many patients require subsequent coronary angiograms, and TFA has traditionally been the most commonly used access site in cannulation in these patients [10]. Unfortunately, most studies comparing radial and femoral approaches excluded CABG patients and therefore limited studies are available regarding the ideal access site [2].
First introduced by Kiemeneij [10] in 2017, LdTRA, has increasingly been used for arterial access in PCI. This technique involves accessing the distal radial artery in the anatomical snuffbox of the hand [10]. It is a much more feasible approach in patients with prior CABG involving left inframammary artery (LIMA) grafts [11] and more ergonomic for both the operator and the patient as it requires the hand to remain pronated during the procedure [12] and spares the superficial palmar branch thus reducing the risk of RAO and compartment syndrome of forearm [13]. To the best of our knowledge, this is the first retrospective study addressing the simultaneous comparison of LdTRA, TRA, and TFA in post-CABG patients undergoing coronary angiography..
2. Methods
We retrospectively studied 417 patients with prior CABG who were undergoing coronary angiography at our institution’s cardiac catheterization lab between January 2018 and August 2020, to compare the type of intervention using the site of access as an independent factor. The study took place in consideration of ethical principles for medical research involving human subjects. No recruitment was needed as there was no intervention involved. The procedures were performed by board certified interventional cardiologists who were skilled in radial access. There was no consent taken as this was a retrospective chart review. Data collection was performed through chart review. Patients with no prior history of CABG were excluded from the study. The following information was obtained: Patient demographics (age, gender, BMI, smoking), pre-existing medical conditions (diabetes, hyperlipidemia, COPD, hypertension, CKD), family history of ischemic heart disease (IHD), prior PCI, prior history of heart failure, prior history of myocardial infarction (MI), information on catheterization procedure (eg time to gain access, access site, procedure duration, fluoroscopy dose and fluoroscopy time) and length of hospital stay.
These parameters were examined in three groups of patients who have had coronary angiography +- intervention; the first group who had their angiography access via the TFA to those with TRA versus those who had their access via LdTRA. We screened patients' charts using Xper IM. Analyses were performed by Statistical Product and Services Solution using the Chi-Square test and Pearson's correlation for categorical data and ANOVA test for nominal data. All the analyses were done using an alpha (α) level of <0.05. Pre-defined endpoints were time to access, procedure duration, fluoroscopy time, and dose and length of hospital stay. Mortality was not observed among the three groups.
3. Results
650 patients were screened from the hospital database using Prior CABG as screening criteria. (ICD 10 Codes: Z95.1). After an initial screening to include patients who had their right radial artery used as a graft during CABG, 398 patients were found eligible for study participation as shown in flow diagram.
Figure 1: Study Flow Diagram showing total and final number of patients in retrospective analysis after application of exclusion criteria
Based upon whether LdTRA, right TRA or femoral artery was used for vascular access, patients were classified into three groups. Out of the total sample size of 398 patients, 324 patients underwent coronary angiography using femoral approach, 28 patients had LdTRA and about 46 patients had right TRA. Out of 398 patients, 78.4% were identified as males and 21.6% were identified as females. The mean age was 71.6 years. 14.3% were smokers, 97.5% had hypertension, 50.5% had diabetes, 98.0% had hyperlipidemia, 35.2% had a family history of Ischemic heart disease, 52.3% had a prior myocardial infarction, and 27.6% had a history of prior heart failure. The distribution of the type of approach used during PCI using demographic characters was as follows:
Table1 A:
|
Femoral Approach |
Left distal Radial Approach |
Right proximal radial Approach |
||||
|
Number |
Percentage |
Number |
Percentage |
Number |
Percentage |
|
|
Number of patients |
324 |
81.4 |
28 |
7.0 |
46 |
11.6 |
Table 1 B:
Table 1: A: Distribution of total sample size with respect to type of access,
B: showing distribution of demographic risk factors in all three subgroups of arterial access
Considering BMI as a risk factor for ease of access, patients were classified based on BMI into further subgroups as
- Group 1: BMI = <18.5
- Group 2: BMI= 5-24.9
- Group 3: BMI= 0-29.9
- Group 4: BMI= 0-34.9
- Group 5: BMI= 0-39.9
- Group6: BMI= >40.0
Table 2: Distributions of BMI in the subgroups based on type of access
|
Femoral approach |
Left distal radial approach |
Right proximal radial approach |
||||
|
Sample |
Percentage |
Sample |
Percentage |
Sample |
Percentage |
|
|
Group 1 |
3 |
0.9 |
0 |
0.0 |
2 |
4.3 |
|
Group 2 |
65 |
20.1 |
5 |
17.9 |
6 |
13.0 |
|
Group 3 |
124 |
38.3 |
10 |
35.7 |
9 |
19.6 |
|
Group 4 |
93 |
28.7 |
8 |
28.6 |
17 |
37.0 |
|
Group 5 |
23 |
7.1 |
4 |
14.3 |
6 |
13.0 |
|
Group 6 |
16 |
4.9 |
1 |
3.6 |
6 |
13.0 |
Time of access, time of procedure, fluoroscopy time, fluoroscopy dose, length of post-procedural stay were the parameters used to judge the clinical difference between the approaches used. The results are as follows: The mean time for femoral access was 37.68±1.19 seconds (95% CI 35.3295-40.04), for snuffbox access 36.4±5.06 seconds (95% CI=26.03-46.81), and for proximal radial access 40.71±4.17 seconds (95% CI=31.21-50.20).Mean procedural time via femoral access was 37.68±1.97 minutes, via snuffbox access was 36.43±5.06 minutes, and via radial access was 40.71±4.17 minutes. Mean length of stay for femoral access was 1.97±0.14 days, for radial access 2.13±0.31 days and for snuffbox access 1.68±0.27 days. The fluoroscopy time for femoral access was 10.23±0.41 minutes, for snuffbox access was 11.28±2.00 minutes and for radial access was 13.23±1.74 minutes. The fluoroscopy dose for femoral access was 599.98±26.63 Gy/cm2, for snuffbox approach 722.71±112.94 Gy/cm2 and for radial access was 767.06±90.89 Gy/cm2. There were no complications noted in our study. We found no statistical significance difference between approaches with regards to time of access, procedure duration, fluoroscopy time and dose.
Table 3: showing the relationship between different measured parameters with reference to type of access
|
Femoral Approach |
Left Radial Approach |
Right proximal radial Approach |
||||
|
Mean time |
95% CI |
Mean time |
95% CI |
Mean time |
95% CI |
|
|
Time for access (Seconds) |
36.4±5.06 |
26.03-46.81 |
40.71±4.17 |
31.21-50.2 |
37.68±1.19 |
35.33-40.04 |
|
Procedural time (Seconds) |
36.43±5.06 |
26.52-46.34 |
40.71±4.17 |
32.54-48.88 |
37.68±1.97 |
33.82-41.54 |
|
Fluoroscopy time (Seconds) |
11.28±2 |
7.36-15.2 |
13.23±1.74 |
9.82-16.64 |
10.23±0.41 |
9.63-11.04 |
|
Fluoroscopy dose (Gy/cm2) |
722.71±112.94 |
501.35-944.07 |
767.06±90.89 |
588.92-945.21 |
599.98±26.63 |
547.79-652.17 |
|
Length of stay (Days) |
1.68±0.27 |
1.15-2.21 |
2.13±0.31 |
1.53-2.74 |
1.97±0.14 |
1.7-2.24 |
Table 4: showing the results of Chi- square test to identify statistical significance of difference between the choice of site for access and the demographic risk factors
|
Access Site |
|||||||
|
Femoral |
Left Radial |
Right proximal radial |
Chi Square Value |
Asymp Sig. |
|||
|
Age |
<50 yrs |
Observed |
2 |
0 |
0 |
18.577 |
0.046 |
|
Expected |
1.81.8111.81. |
0.1 |
0.1 |
||||
|
50-60 yrs |
Observed |
24 |
3 |
9 |
|||
|
Expected |
29.1 |
2.6 |
4.3 |
||||
|
61-70 yrs |
Observed |
91 |
7 |
18 |
|||
|
Expected |
94.4 |
8.2 |
13.4 |
||||
|
71-80 yrs |
Observed |
113 |
11 |
16 |
|||
|
Expected |
114 |
9.8 |
16.2 |
||||
|
81-90 yrs |
Observed |
90 |
6 |
2 |
|||
|
Expected |
79.8 |
6.9 |
11.3 |
||||
|
91-100 yrs |
Observed |
4 |
1 |
1 |
|||
|
Expected |
4.9 |
0.4 |
0.7 |
||||
|
Gender |
Male |
Observed |
249 |
25 |
38 |
2.898 |
0.235 |
|
Expected |
254 |
21.9 |
36.1 |
||||
|
Female |
Observed |
75 |
3 |
8 |
|||
|
Expected |
70 |
6.1 |
9.9 |
||||
|
Smoker |
No |
Observed |
281 |
26 |
34 |
6.656 |
0.036 |
|
Expected |
277.6 |
24 |
39.4 |
||||
|
Yes |
Observed |
43 |
2 |
12 |
|||
|
Expected |
46.4 |
4 |
6.6 |
||||
|
Hypertension |
No |
Observed |
10 |
0 |
0 |
2.343 |
0.31 |
|
Expected |
8.1 |
0.7 |
1.2 |
||||
|
Yes |
Observed |
314 |
28 |
46 |
|||
|
Expected |
315.9 |
27.3 |
44.8 |
||||
|
Dyslipidemia |
No |
Observed |
7 |
0 |
1 |
0.618 |
0.734 |
|
Expected |
6.5 |
0.6 |
0.9 |
||||
|
Yes |
Observed |
317 |
28 |
45 |
|||
|
Expected |
317.5 |
27.4 |
45.1 |
||||
|
Family History of Cardiac Disease |
No |
Observed |
216 |
17 |
25 |
2.904 |
0.234 |
|
Expected |
210 |
18.2 |
29.8 |
||||
|
Yes |
Observed |
108 |
11 |
21 |
|||
|
Expected |
114 |
9.8 |
16.2 |
||||
|
Prior Myocardial Infarction |
No |
Observed |
154 |
17 |
19 |
2.659 |
0.265 |
|
Expected |
154.7 |
13.4 |
22 |
||||
|
Yes |
Observed |
170 |
11 |
27 |
|||
|
Expected |
169.3 |
14.6 |
24 |
||||
|
Prior Heart Failure |
No |
Observed |
236 |
20 |
32 |
0.229 |
0.892 |
|
Expected |
234.5 |
20.3 |
33.3 |
||||
|
Yes |
Observed |
88 |
8 |
14 |
|||
|
Expected |
89.5 |
7.7 |
12.7 |
||||
|
Prior PCI |
No |
Observed |
147 |
18 |
24 |
4.156 |
0.125 |
|
Expected |
153.9 |
13.3 |
21.8 |
||||
|
Yes |
Observed |
177 |
10 |
22 |
|||
|
Expected |
170.1 |
14.7 |
24.2 |
||||
|
Valve Surgery |
No |
Observed |
292 |
27 |
43 |
0.648 |
0.439 |
|
Expected |
294.7 |
25.5 |
41.8 |
||||
|
Yes |
Observed |
32 |
1 |
3 |
|||
|
Expected |
29.3 |
2.5 |
4.2 |
||||
|
BMI |
<18.5 |
Observed |
3 |
0 |
2 |
18.674 |
0.97 |
|
Expected |
4.1 |
0.4 |
0.6 |
||||
|
18.5-24.9 |
Observed |
65 |
5 |
6 |
|||
|
Expected |
61.9 |
5.3 |
8.8 |
||||
|
25.0-29.9 |
Observed |
124 |
10 |
9 |
|||
|
Expected |
116.4 |
10.1 |
16.5 |
||||
|
30.0-34.9 |
Observed |
93 |
8 |
17 |
|||
|
Expected |
961 |
8.3 |
13.6 |
||||
|
35.0-39.9 |
Observed |
23 |
4 |
6 |
|||
|
Expected |
26.9 |
2.3 |
3.8 |
||||
|
>40.0 |
Observed |
16 |
1 |
6 |
|||
|
Expected |
18.7 |
1.6 |
2.6 |
||||
|
CKD With Dialysis |
No |
Observed |
302 |
27 |
44 |
0.784 |
0.676 |
|
Expected |
303.6 |
26.2 |
43.1 |
||||
|
Yes |
Observed |
22 |
1 |
2 |
|||
|
Expected |
20.4 |
1.8 |
2.9 |
||||
|
COPD |
No |
Observed |
234 |
20 |
31 |
0.463 |
0.793 |
|
Expected |
232 |
20.1 |
32.9 |
||||
|
Yes |
Observed |
90 |
8 |
15 |
|||
|
Expected |
92 |
7.9 |
13.1 |
||||
|
DM |
No |
Observed |
155 |
16 |
26 |
1.919 |
0.383 |
|
Expected |
160.4 |
13.9 |
22.8 |
||||
|
Yes |
Observed |
169 |
12 |
20 |
|||
|
Expected |
163.6 |
14.1 |
23.2 |
||||
The Chi Square Test shows that there is a significant difference between choice of site of access and Age and smoking status (p <0.05). ANOVA test was run using Site of access, categorical age, categorical BMI and smoking as independent factor and procedural time, time of access, length of Hospital stay, fluoroscopy time and fluoroscopy dose as dependent factors. One way ANOVA revealed that there was a statistical significant difference in fluoroscopy dose between at least two groups based on BMI. (F(5,392)=[12.153], p<0.001). Similarly, there was a statistically significant difference in the time of access in patients grouped based on smoking (F(1,396)=[6.795], p=0.009).
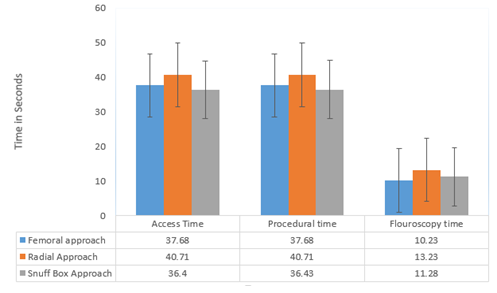
Figure 1: Bar chart showing the relationship between access time, procedure time and fluoroscopic time in all three approaches
Student-Newman-Keuls Post-Hoc Analysis was conducted to see the statistically significant difference between subgroups. Post Hoc Analysis could not be carried out for the relationship of smoking and time of access. However, Post Hoc Analysis showed that the mean dose of fluoroscopy significantly varies between patients with BMI <30 and those with >30. All the analysis were done using alpha (α) level of <0.05. Based on the findings as stated above, our study did not find any statistical significant difference the choice of site of access, the demographic factors, time of access, procedural time, fluoroscopy time, fluoroscopy dose and length of Hospital stay, except for a significant increased fluoroscopy dose in patients with BMI >30. Therefore, the null hypothesis holds stating that there is no difference in outcome of patient regardless of site of access use.
4. Discussion
Radial access remains the most preferred way of coronary angiography by operators today [14]. Multiple studies, including randomized trials that compared TRA with TFA have shown that TRA is associated with greater patient satisfaction, reduced bleeding and vascular complications [15], reduced morbidity and mortality [16-19], and cost reductions [20].
However, although infrequent, TRA is associated with some known complications such as asymptomatic and symptomatic RAO, perforation, spasm, nonocclusive injury, pseudoaneurysm and arteriovenous fistulae [21-22]. These complications may prevent future utilization of the radial artery, including use as the grafting vessel in coronary artery bypass graft (CABG), repeat access for staged or repeat PCI and establishing arteriovenous fistulae in chronic renal dysfunction [23]. The right TRA is more commonly used as compared to the left TRA, because performing catheterization through the left TRA approach is ergonomically challenging for operators, especially in cases of obese patients and short operators [6]. In patients whom the left radial is chosen (e.g. right radial tortuosity, spasm or occlusion and in the left internal mammary angiography graft), these technicalities may be overcome by using the left distal transradial approach (LdTRA), otherwise called the anatomical snuffbox approach [23, 24]. First introduced in 2017 by Kiemencij [10], this approach was found to be more convenient for both parties involved because patients can keep their left hand pronated near their right groin, which allows the operator to cannulate the artery at the snuffbox without reaching across the patient [12]. The risk of complications was also lower with LdTRA as it spares the palmar branch that supplies the deep palmar arch, reducing ischemic hand events and also facilitates early hemostasis [6].
The patients with prior history of CABG undergoing PCI are traditionally approached using the femoral artery and are often excluded from the studies comparing the TFA and TRA [2]. In this subgroup of prior CABG, several factors have to be taken into account such as graft anatomy, graft degeneration, long standing atherosclerosis and diffusely diseased aortic wall [2]. The novel LdTRA has proven to have a better safety profile and higher satisfaction in recent years [4]. This is mainly due to shortened compression time, better hemostasis and lower incidence of RAO and spasm [4,13]. It was previously thought that LdTRA was associated with increased rate of cannulation failure and increased time of access when compared to TRA [25]. However, recent studies and meta-analysis have shown no difference in access success rate and puncture time between TRA and LdTRA approaches when performed by experienced operators [6].
Our study population was heterogeneous with mostly elderly patients with a mean age of 71.6 years. We also had a large number of patients with hypertension (97.5%), almost fifty percent had diabetes and 25% receiving hemodialysis. In end stage renal disease patients on hemodialysis, operators may prefer to use distal transradial access, as it will preserve the proximal artery for a future arteriovenous fistula [26]. Almost 35 % of patients were overweight (BMI 25-29) and almost thirty percent of patients were obese (BMI >/= 30). Central obesity may preclude the patient from being able to place their left arm across their lower abdomen in position for the operator to cannulate the artery [27]. Advancing the wire at the point of the elbow can be troublesome especially when patients are obese and must bend their elbow to place their hand at their right groin [27]. Additionally, using post hoc analysis, the mean dose of fluoroscopy significantly varies between patients with BMI <30 and those with >30 and it showed significantly increased fluoroscopy doses in patients with BMI >30.
The main results of our study did not show any statistically significant difference between the three approaches for invasive coronary procedures in terms of set endpoints. Ghose T et al reported that with LdTRA, there was a statistically significant increased mean procedure time, mean fluoroscopic time and similar fluoroscopic dose compared with TRA [28]. With regards to radiation exposure, the LdTRA approach places the operator farther away from the radiation source as the patient's hand is placed at the right groin, which may reduce radiation exposure to the operator [29]. Our study did not show any statistically significant difference between all three accesses for the aforementioned outcomes. A possible explanation for this difference could be due to the experience of the operators or the fact that our study had fewer participants. Similar to our retrospective study, Stefano et al reported in their meta-analysis that, in patients with previous CABG undergoing coronary procedures, TRA is associated with similar procedural and fluoroscopy times compared with TFA [11]. Several observational studies comparing TRA with TFA showed there are reduced complications with the transradial approach [30]. Data from the triangle registry [31] showed that there was a longer puncture time and a longer fluoroscopic time in LdTRA compared with rdRA (right distal radial access). The registry used no randomization or control group [31].
Coughlan ct. al [27] found that LdTRA could shorten length of stay for patients from a post-procedural standpoint. This was secondary to shortened post procedural radial compression time as compared with TRA. Our study in comparison with LdTRA, TRA and TFA did not show any difference between length of hospital stay. At this time there are no studies in the literature comparing LdTRA with conventional access methods in patients with prior CABG. Considering that most patients with CABG have in-situ left internal mammary artery (IMA) grafts and a variable number of aortocoronary saphenous vein grafts, LdTRA would probably be most appropriate given the ergonomic benefit to the operator, particularly in what can be a longer procedure in which several grafts need to be cannulated.
5. Study Limitation:
Our study is limited by a relatively small study sample, single-center experience with two operators performing the vast majority of the distal radial cases, and the retrospective nature of the analysis. To best answer the question of which access site is best for patients with prior CABG undergoing coronary angiography, a randomized trial would be needed.
6. Conclusion:
Due to the lack of statistical significance between outcomes of either approach, all approaches remain reasonable access options in post-CABG patients. Clinically, the left distal radial approach may be superior and is recommended by the authors of this study because it avoids the risks of femoral access complications in these complex patients, allows an easy approach to the LIMA graft, and is more ergonomic for the operator than left proximal radial access.
References
- Marbach JA, Alhassani S, Wells G, Le May M. Radial access first for PCI in acute coronary syndrome : Are we propping up a straw man? Herz 45 (2020): 548-556.
- Burzotta F, Trani C, Hamon M, Amoroso G, Kiemeneij F. Transradial approach for coronary angiography and interventions in patients with coronary bypass grafts: tips and tricks. Catheter Cardiovasc Interv 72 (2008): 263-72.
- Imori Y, Akasaka T, Ochiai T, Oyama K, Tobita K, Shishido K, Nomura Y, Yamanaka F, Sugitatsu K, Okamura N, Mizuno S, Arima K, Suenaga H, Murakami M, Tanaka Y, Matsumi J, Takahashi S, Tanaka S, Takeshita S, Saito S. Co-existence of carotid artery disease, renal artery stenosis, and lower extremity peripheral arterial disease in patients with coronary artery disease. Am J Cardiol 113 (2014): 30e35.
- Oliveira MDP, Navarro EC, Caixeta A. Distal transradial access for post-CABG coronary and surgical grafts angiography and interventions. Indian Heart J 73 (2021): 440-445.
- Amin AP, Patterson M, House JA, et al. Costs associated with access site and same-day discharge among medicare beneficiaries undergoing percutaneous coronary intervention: an evaluation of the current percutaneous coronary intervention care pathways in the United States. JACC Cardiovasc Interv 10 (2017): 342.
- Cao J, Cai H, Liu W, Zhu H, Cao G. Safety and Effectiveness of Coronary Angiography or Intervention through the Distal Radial Access: A Meta-Analysis. J Interv Cardiol 12 (2021): 4371744.
- Cooper CJ, El-Shiekh RA, Cohen DJ, Blaesing L, Burket MW, Basu A, Moore JA. Effect of transradial access on quality of life and cost of cardiac catheterization: A randomized comparison. Am Heart J 138 (1999): 430-6.
- Plourde G, Pancholy SB, Nolan J, Jolly S, Rao SV, Amhed I, Bangalore S, Patel T, Dahm JB, Bertrand OF. Radiation exposure in relation to the arterial access site used for diagnostic coronary angiography and percutaneous coronary intervention: a systematic review and meta-analysis. Lancet 386 (2015): 2192e2203.
- Locker C, Schaff HV, Dearani JA, Joyce LD, Park SJ, Burkhart HM, Suri RM, Greason KL, Stulak JM, Li Z, Daly RC. Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery: analysis of 8622 patients with multivessel disease. Circulation 126 (2012):1023e1030.
- Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention 13 (2017): 851-857.
- Rigattieri S, Sciahbasi A, Brilakis ES, Burzotta F, Rathore S, Pugliese FR, Fedele S, Ziakas AG, Zhou YJ, Guzman LA, Anderson RA. Meta-Analysis of Radial Versus Femoral Artery Approach for Coronary Procedures in Patients With Previous Coronary Artery Bypass Grafting. Am J Cardiol 117 (2016): 1248-55.
- Al-Azizi KM, Grewal V, Gobeil K, Maqsood K, Haider A, Mohani A, Giugliano G, Lotfi AS. The Left Distal Transradial Artery Access for Coronary Angiography and Intervention: A US Experience. Cardiovasc Revasc Med 20 (2019): 786-789.
- Sgueglia GA, Lee BK, Cho BR, Babunashvili A, Lee JB, Lee JW, Schenke K, Lee SY, Harb S. Distal Radial Access: Consensus Report of the First Korea-Europe Transradial Intervention Meeting. JACC Cardiovasc Interv 14 (2021): 892-906.
- Balaban Y, Akbas MH, Akbas ML, Özerdem A. Efficacy and Safety of "Coronary Artery Bypass Graft Angiography" with Right Transradial Access versus Left Transradial Access and Femoral Access: a Retrospective Comparative Study. Braz J Cardiovasc Surg 34 (2019): 48-56.
- Rao SV, Tremmel JA, Gilchrist IC, Shah PB, Gulati R, Shroff AR, Crisco V, Woody W, Zoghbi G, Duffy PL, Sanghvi K, Krucoff MW, Pyne CT, Skelding KA, Patel T, Pancholy SB; Society for Cardiovascular Angiography and Interventions Transradial Working Group. Best practices for transradial angiography and intervention: a consensus statement from the society for cardiovascular angiography and intervention's transradial working group. Catheter Cardiovasc Interv 83 (2014): 228-36.
- Valgimigli, Marco, et al. "Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial." The Lancet9986 (2015): 2465-2476.
- Valgimigli, Marco, et al. "Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial." The Lancet10150 (2018): 835-848.
- Chase, Alex J., et al. "Association of the arterial access site at angioplasty with transfusion and mortality: the MORTAL study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg)." Heart8 (2008): 1019-1025.
- Vorobcsuk, András, et al. "Transradial versus transfemoral percutaneous coronary intervention in acute myocardial infarction: systematic overview and meta-analysis." American heart journal5 (2009): 814-821.
- Anjum I, Khan MA, Aadil M, Faraz A, Farooqui M, Hashmi A. Transradial vs. Transfemoral Approach in Cardiac Catheterization: A Literature Review. Cureus 9 (2017): e1309.
- Kanei Y, Kwan T, Nakra NC, Liou M, Huang Y, Vales LL, Fox JT, Chen JP, Saito S. Transradial cardiac catheterization: a review of access site complications. Catheter Cardiovasc Interv 78 (2011): 840-6.
- Bhat T, Teli S, Bhat H, Akhtar M, Meghani M, Lafferty J, Gala B. Access-site complications and their management during transradial cardiac catheterization. Expert Rev Cardiovasc Ther 10 (2012): 627-34.
- Cai G, Huang H, Li F, Shi G, Yu X, Yu L. Distal transradial access: a review of the feasibility and safety in cardiovascular angiography and intervention. BMC Cardiovasc Disord 20 (2020): 356.
- Sgueglia G, Summaria F, Gioffrè G, et al. TCT-782 Slender Distal Transradial Access for Complex Percutaneous Coronary Intervention: A Case-Matched Comparison With Classical Radial Approach. J Am Coll Cardiol 74 (2019): B766.
- Hammami R, Zouari F, Ben Abdessalem MA, Sassi A, Ellouze T, Bahloul A, Mallek S, Triki F, Mahdhaoui A, Jeridi G, Abid L, Charfeddine S, Kammoun S, Jdidi J. Distal radial approach versus conventional radial approach: a comparative study of feasibility and safety. Libyan J Med 16 (2021): 1830600.
- Sgueglia GA, Di Giorgio A, Gaspardone A, et al. Anatomic Basis and Physiological Rationale of Distal Radial Artery Access for Percutaneous Coronary and Endovascular Procedures. JACC Cardiovasc Interv 11 (2018): 2113-9.
- Coughlan JJ, Zebrauskaite A, Arnous S, Kiernan TJ. Left distal trans-radial access facilitates earlier discharge post-coronary angiography. J Interv Cardiol 31 (2018): 964-968.
- Ghose T, Kachru R, Dey J, et al. Safety and Feasibility of Ultrasound-Guided Access for Coronary Interventions through Distal Left Radial Route. J Interv Cardiol (2022): 2141524.
- Liang C, Han Q, Jia Y, Fan C, Qin G. Distal Transradial Access in Anatomical Snuffbox for Coronary Angiography and Intervention: An Updated Meta-Analysis. J Interv Cardiol 22 (2021): 7099044.
- Januszek R, Siudak Z, Malinowski KP, Wanha W, Wojakowski W, Gasior M, Bartus S, Dudek D. Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting. J Clin Med 12 (2020): 764.
- Schenke K, Viertel A, Joghetaei N, Prog R, Matthiesen T, Ohm S, Dill T, Bott-Flügel L, xGrönefeld G. Distal Transradial Access for Coronary Angiography and Interventions in Everyday Practice: Data From the TRIANGLE Registry (TwitteR Initiated registry for coronary ANgiography in Germany via distaL radial accEss). Cardiol Ther 10 (2021): 241-253.
