Cirrhosis and its Complication: other Clinical Complications Except ACLF and Critical Illness
Article Information
Umair Akram1, Muhammad Faizan Iqbal 2, Priya3, Berkha4, Rumela5, Uma Devi6
1District Head Quarter Hospital Vehari
2Mohiuddin Teaching Hospital Mirpur
3Chandkaa Medical College Hospital Larkana
4Peoples Medical College
5Jinnah Postgraduate Medical Center Karachi
6Abbasi Shaheed Hospital Karachi
*Corresponding author: Umair Akram. District Head Quarter Hospital Vehari Pakistan
Received: 19 May 2023; Accepted: 24 May 2023; Published: 30 May 2023
Citation:
Umair Akram, Muhammad Faizan Iqbal, Priya, Berkha, Rumela, Uma Devi. Cirrhosis and its Complication: other Clinical Complications Except Aclf and Critical Illness. Archives of Clinical and Biomedical Research. 7 (2023): 382-386.
Share at FacebookAbstract
Cirrhosis results from chronic liver disease, and is characterized by advanced fibrosis, scarring, and formation of regenerative nodules leading to architectural distortion. The main objective of the study is to find the cirrhosis and its complication, other clinical complications except ACLF and critical illness. This descriptive study was conducted at DHQ hospital, Vehari, Pakistan during June 2022 to January 2023. A comprehensive literature search of the published data was performed in regard with the spectrum, diagnosis, and management of cirrhosis and its complications. Data was also collected from OPD of the hospital record. We include all patients suffering from liver cirrhosis and its complication. It is concluded that patients with cirrhosis have progressive disease and suffer from multiple complications like ascites, HE, variceal bleeding, hepatorenal syndrome, cirrhotic cardiomyopathy, pulmonary syndromes, sarcopenia, frailty, and HCC. The prevention, early diagnosis, treatment, and palliation of these complications are essential in comprehensive clinical care plans.
Keywords
ACLF; Cirrhosis; Patients
ACLF articles; Cirrhosis articles; Patients articles
Article Details
1. Introduction
Cirrhosis results from chronic liver disease, and is characterized by advanced fibrosis, scarring, and formation of regenerative nodules leading to architectural distortion. In the past cirrhosis was generally thought to be irreversible but recent studies have shown that treatments aimed at the underlying cause especially in earlier stages of the disease can improve or even reverse fibrosis. Patients with cirrhosis are at increased risk of numerous complications and have a decreased life expectancy [1]. In 2010, cirrhosis was the eight-leading cause of death in the United States and, combined with its complications accounted for approximately 49500 deaths.
Cirrhosis is characterized by fibrosis and nodule formation of the liver, secondary to a chronic injury, which leads to alteration of the normal lobular organization of the liver. Various insults can injure the liver, including viral infections, toxins, hereditary conditions, or autoimmune processes [2]. With each injury, the liver forms scar tissue (fibrosis), initially without losing its function. After a long-standing injury, most of the liver tissue gets fibrosed, leading to loss of function and the development of cirrhosis [3].
The occurrence of complications in patients with cirrhosis such as jaundice, ascites, encephalopathy, infection, renal dysfunction or variceal bleeding requiring hospitalization alters the natural history of the disease with an increase in 5-year mortality as high as 40–50%. A significant proportion of these patients with acute decompensation require management in the intensive care unit (ICU) with organ support and have a high rate of in-hospital mortality. This category of patients with cirrhosis, acute decompensation and organ failure has been recently classified by a consensus conference as having acute on chronic liver failure (ACLF) [4].
Cirrhosis-related portal hypertension (PH) leads to the formation of collateral channels and increased intermediaries like endogenous vasoconstrictors (norepinephrine, plasma renin activity, aldosterone, etc), vascular endothelial growth factor and splanchnic vasodilators like nitric oxide [5]. PH also leads to the expansion of plasma volume due to the activation of the renin angiotensin aldosterone pathway, which increases cardiac output and alters systemic hemodynamics, which is core to the pathogenesis of several complications. PH can be quantified by the measurement of the hepatic venous pressure (HVPG) [6].
Multiple cells play a role in liver cirrhosis, including hepatocytes and sinusoidal lining cells such as hepatic stellate cells (HSCs), sinusoidal endothelial cells (SECs), and Kupffer cells (KCs). HSCs form a part of the wall of the liver sinusoids, and their function is to store vitamin A. When these cells are exposed to inflammatory cytokines, they get activated, transform into myofibroblasts, and start depositing collagen, which results in fibrosis. SECs form the endothelial lining and are characterized by the fenestrations they make in the wall that allow the exchange of fluid and nutrients between the sinusoids and the hepatocytes [7].
Defenestration of the sinusoidal wall can happen secondary to chronic alcohol use and promote perisinusoidal fibrosis. KCs are satellite macrophages that line the wall of the sinusoids as well. Studies mainly from animal models have shown that they play a role in liver fibrosis by releasing harmful mediators when exposed to injurious agents and acting as antigen-presenting cells for viruses. Hepatocytes are also involved in cirrhosis's pathogenesis, as damaged hepatocytes release reactive oxygen species and inflammatory mediators that can promote activating HSCs and liver fibrosis [8].
Objective: The main objective of the study is to find the cirrhosis and its complication, other clinical complications except ACLF and critical illness.
2. Materials and Methods
This descriptive study was conducted in DHQ hospital, Vehari, Pakistan during June 2022 to January 2023. A comprehensive literature search of the published data was performed in regard with the spectrum, diagnosis, and management of cirrhosis and its complications. Data was also collected from OPD of the hospital record. We include all patients suffering from liver cirrhosis and its complication.
Following are some complications which we observed in cirrhosis patients during analysis and study.
|
Complication |
Clinical Presentation |
|
Hepatic encephalopathy (HE) |
HE produces a wide spectrum of nonspecific neurological and psychiatric manifestations. Minimal HE is diagnosed by abnormal psychometric tests. Clinically overt HE includes personality changes, alterations in consciousness progressive disorientation in time and space, somnolence, stupor and, finally, coma. |
|
Hepatopulmonary syndrome (HPS) |
abnormal arterial oxygenation caused by intrapulmonary vascular dilatations (IPVDs) in the setting of liver disease, portal hypertension, or congenital portosystemic shunts |
|
Hepatorenal syndrome (HRS) |
HRS develops in patients with advanced cirrhosis so they will usually have jaundice and other stigmata of chronic liver disease such as finger clubbing, palmar erythema and spider naevi. Other clinical features include splenomegaly, bleeding tendency, hepatic encephalopathy, oedema and ascites. |
|
Variceal bleeding |
Once varices are bleeding, patients classically present with symptoms of an upper gastrointestinal hemorrhage such at hematemesis, passage of black or bloody stools, lightheadedness, or decreased urination. |
|
Hepatic hydrothorax |
Hepatic hydrothorax can present asymptomatically or with cough, dyspnea, hypoxia, or respiratory failure depending on the volume of fluid in the pleural space, the rapidity of the accumulation of the pleural fluid, and the presence of coexistent cardiopulmonary diseases. |
|
Porto-pulmonary hypertension |
Portopulmonary hypertension (PPHTN) refers to pulmonary arterial hypertension that is associated with portal hypertension; it is a well-recognized complication of portal hypertension due to chronic liver disease or extrahepatic causes |
Table 1: Cirrhosis and its complications in all selected patients
2.1 Epidemiology of Cirrhosis
Cirrhosis- and PH-related complications contribute to the public health burden of morbidity and mortality in Pakistan. Age, gender, family income, employment status, status of residence (rural or urban), lifestyle, alcohol, smoking, nutritional status, and education may all have bearing on the etiology. The major cause of morbidity and mortality in cirrhotic patients is the development of portal hypertension and hyperdynamic circulation. Portal hypertension develops secondary to fibrosis and vasoregulatory changes, both intrahepatically and systematically, leading to collateral circulation formation and hyperdynamic circulation [9].
Intrahepatically, SECs synthesize both nitric oxide (NO) and endothelin-1 (ET-1), which act on HSCs, causing relaxation or contraction of the sinusoids, respectively, and controlling sinusoidal blood flow. In patients with cirrhosis, there is an increase in ET-1 production, as well as an increase in the sensitivity of its receptors with a decrease in NO production. This leads to increased intrahepatic vasoconstriction and resistance, initiating portal hypertension. Vascular remodeling mediated by the contractile effects of HSCs in the sinusoids augments the increase in vascular resistance. To compensate for this increase in intrahepatic pressure, collateral circulation is formed [10].
In systemic and splanchnic circulation, the opposite effect happens, with an increase in NO production, leading to systemic and splanchnic vasodilation and decreased systemic vascular resistance. This promotes the activation of the renin-angiotensin-aldosterone system (RAAS), leading to sodium and water retention and resulting in a hyperdynamic circulation. Thus, in cirrhosis with portal hypertension, there is depletion of vasodilators (predominantly NO) intra-hepatically but an excess of NO extrahepatically in the splanchnic and systemic circulation, leading to sinusoidal vasoconstriction and splanchnic (systemic) vasodilation. The collaterals also contribute to the hyperdynamic circulation by increasing the venous return to the heart [11].
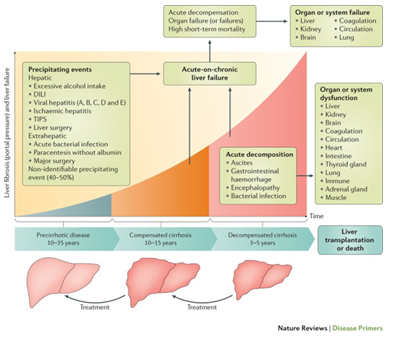
Figure 1: The clinical course of cirrhosis.
2.2 Histopathology of Liver Cirrhosis
Morphologically, cirrhosis is (1) micronodular, (2) macronodular, or (3) mixed. This classification is not as clinically useful as etiologic classification [12].
- Micronodular cirrhosis (uniform nodules less than 3 mm in diameter): Cirrhosis due to alcohol, hemochromatosis, hepatic venous outflow obstruction, chronic biliary obstruction, jejunoileal bypass, and Indian childhood cirrhosis.
- Macronodular cirrhosis (irregular nodules with a variation greater than 3 mm in diameter): Cirrhosis due to hepatitis B and C, alpha-1 antitrypsin deficiency, and primary biliary cholangitis.
- Mixed cirrhosis (when features of both micronodular and macronodular cirrhosis are present): Usually, micronodular cirrhosis progresses into macronodular cirrhosis over time.
2.3 Etiology Classification
Based on the cause of cirrhosis which is sub-classified as follows:
- Viral - hepatitis B, C, and D
- Toxins - alcohol, drugs
- Autoimmune - autoimmune hepatitis
- Cholestatic - primary biliary cholangitis, primary sclerosing cholangitis
- Vascular - Budd-Chiari syndrome, sinusoidal obstruction syndrome, cardiac cirrhosis
- Metabolic - hemochromatosis, NASH, Wilson disease, alpha-1 antitrypsin deficiency, cryptogenic cirrhosis [13].
2.4 Complications of Cirrhosis
The main complications in cirrhosis warranting periodic screening are gastrointestinal varices, ascites, and HCC.13 In a large Asia–Pacific database, about 54.3% of global deaths attributable to cirrhosis were reported from Asia. About 72.7% of HCC-related mortality and two-third of the global burden of chronic hepatitis B and C were recorded from this region. Despite the availability of a safe and cost-effective vaccine, chronic HBV infection remains the cause of >50% of deaths attributable to cirrhosis from Asia. Alcohol (20.8%), NAFLD (12.1%), and chronic HCV infection (15.7%) are the next three etiologies. In 2015, HBV accounted for 50% of mortality due to HCC in Asia [13].
2.5 Hepatic encephalopathy (HE)
Hepatic encephalopathy is an often-temporary neurological (nervous system) disorder due to chronic, severe liver disease. A diseased liver struggles to filter toxins (substances created from the breakdown of food, alcohol, medications and even muscle) from the bloodstream. These toxins build up in the body and travel to the brain. Toxicity affects brain function and causes cognitive impairment [14].
People with hepatic encephalopathy may seem confused or have difficulty processing their thoughts. Treatments can remove the toxins and reverse the problem. As liver disease progresses, the condition may worsen and become less treatable. Hepatic encephalopathy is also known as portosystemic encephalopathy (PSE) [15].
Hepatopulmonary syndrome (HPS)
Hepatopulmonary syndrome was first proposed in 1977 based on autopsy and clinical findings. Autopsies showed dilated pulmonary vasculature in patients with liver cirrhosis and were thought to cause some of the pulmonary manifestations seen in patients with chronic liver disease. The definition of hepatopulmonary syndrome (HPS) is a reduced arterial oxygen saturation due to dilated pulmonary vasculature in the presence of advanced liver disease or portal hypertension [16].
2.6 Diagnostic criteria for HPS
- Partial pressure of oxygen (PaO2) <80 mm Hg while breathing room air, or alveolar-arterial oxygen gradient (A-aO2) ≥ 15 mm while breathing room air. In patients over 64 years of age, A-aO2 >20 mm Hg is considered diagnostic. The patient should be in a sitting position and at rest.
- Pulmonary vascular dilatation as shown by positive contrast-enhanced echocardiography or by radioactive lung-perfusion scanning (showing brain shunt fraction >6%)
- Portal hypertension (with or without cirrhosis).
2.7 Hepatorenal syndrome (HRS)
Hepatorenal syndrome (HRS) is a life-threatening complication of advanced liver disease that affects your kidney function. It causes prerenal acute kidney failure. That means that it comes on suddenly, without any previous kidney disease or any physical changes to the kidneys themselves. Your kidneys may be healthy, but they lose the ability to function because their blood supply has been compromised [17].
People with hepatorenal syndrome have narrowed and constricted blood vessels in their kidneys in response to liver failure, which reduces blood flow to the kidneys. This progressively slows down kidney functions. Hepatorenal syndrome requires urgent intervention, and in most cases, a liver transplant is the only cure.
2.8 Variceal bleeding
Varices are dilated submucosal veins, most commonly detected in the distal esophagus or proximal stomach. Varices are associated with portal hypertension of any cause including presinusoidal (portal vein thrombosis), sinusoidal (cirrhosis) and postsinusoidal (Budd Chiari syndrome) causes the commonest being cirrhosis. Despite advances in therapy over the last decade, variceal hemorrhage is associated with a mortality of at least 20% at 6 weeks [18].
Hepatic hydrothorax
Hepatic hydrothorax refers to the presence of a pleural effusion (usually >500 mL) in a patient with cirrhosis who does not have other reasons to have a pleural effusion (eg, cardiac, pulmonary, or pleural disease) [19]. Hepatic hydrothorax occurs in approximately 5 to 15 percent of patients with cirrhosis. Patients who develop hepatic hydrothorax are more likely to have ascites, hepatic encephalopathy, acute kidney injury (AKI), and increased risk of mortality. In a retrospective analysis of 495 patients with cirrhosis and pleural effusion, 16 percent had hepatic hydrothorax. While patients with ascites can often tolerate up to 5 to 10 L of fluid with only mild symptoms, those with a pleural effusion can have severe symptoms (such as shortness of breath, cough, and hypoxemia) with as little as 500 mL of fluid [20].
4. Conclusion
It is concluded that patients with cirrhosis have progressive disease and suffer from multiple complications like ascites, HE, variceal bleeding, hepatorenal syndrome, cirrhotic cardiomyopathy, pulmonary syndromes, sarcopenia, frailty, and HCC. The prevention, early diagnosis, treatment, and palliation of these complications are essential in comprehensive clinical care plans. The incorporation of patient-reported outcomes, quality of life assessment and patient driven management algorithms are the need of the hour. Importantly, access to specialized care like locoregional therapy, liver transplantation, advanced imaging and endoscopy, public health programmes for viral hepatitis, alcohol use reduction, obesity, and non-communicable disease policy frameworks can improve disease outcomes in cirrhosis.
References
- Dhiman RK, Grover GS, Premkumar M, et al. Decentralized care with generic direct-acting antivirals in the management of chronic hepatitis C in a public health care setting. J Hepatol 71(2019): 1076–1085.
- Jindal A, Bhardwaj A, Kumar G, et al. Clinical decompensation and outcomes in patients with compensated cirrhosis and a hepatic venous pressure gradient $20 mm Hg. Am J Gastroenterol 115(2020): 1624–1633.
- Thuluvath PJ, Alukal JJ, Zhang T. Impact of hyponatremia on morbidity, mortality, and resource utilization in portal hypertensive ascites: a nationwide analysis. J Clin Exp Hepatol 12(2022):871–875.
- Baijal R, Praveenkumar HR, Amarapurkar DN, et al. Prevalence of tuberculosis in patients with cirrhosis of liver in western India. Trop Doct 40(2010): 163–164.
- Yoshiji H, Nagoshi S, Akahane T, et al. Evidence-based clinical practice guidelines for Liver Cirrhosis 2020. J Gastroenterol 56(2021): 593–619.
- Reynolds TB, Lieberman FL, Goodman AR. Advantages of treatment of ascites without sodium restriction and without complete removal of excess fluid. Gut 19(1978): 549–553.
- Perez Ruiz de Garibay A, Kortgen A, Leonhardt J, et al. Critical care hepatology: definitions, incidence, prognosis and role of liver failure in critically ill patients. Crit Care 26 (2022): 289.
- Nadim Mitra, et al. "Management of the critically ill patient with cirrhosis: A multidisciplinary perspective." Journal of Hepatology 64(2016): 717-735,
- Khanam Arshi, and Kottilil "Acute-on-Chronic Liver Failure: Pathophysiological Mechanisms and Management." Frontiers in Medicine 8(2021).
- Passi Neha, and McPhail "The patient with cirrhosis in the intensive care unit and the management of acute-on-chronic liver failure." Journal of the Intensive Care Society 10 (2020).
- Sarin SK, Kedarisetty CK, Abbas Z, et al. APASL ACLF Working Party. Acute-on-chronic liver failure: consensus recommendations of the Asian pacific association for the study of the liver (APASL). Hepatol Int 8(2014): 453–471.
- McPhail MJW, Shawcross DL, Abeles RD, et al. Increased survival for patients with cirrhosis and organ failure in liver intensive care and validation of the chronic liver failure-sequential organ failure scoring system. Clin Gastroenterol Hepatol 13(2015): 1353–1360.
- Arroyo V, Moreau R, Kamath P, et al. Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Primers 2 (2016): 16041.
- Nusrat S, Khan MS, Fazili J, et al. Cirrhosis and its complications: evidence based treatment. World J Gastroenterol 20(2014): 5442-60.
- Friedman R, Mears JG, Barst RJ. Continuous infusion of prostacyclin normalizes plasma markers of endothelial cell injury and platelet aggregation in primary pulmonary hypertension. Circulation 96(1997): 2782–2784.
- Tan HP, Markowitz JS, Montgomery RA, et al. Liver transplantation in patients with severe portopulmonary hypertension treated with preoperative chronic intravenous epoprostenol. Liver Transpl 7(2001): 745–749.
- Almeida JA, Riordan SM, Liu J, et al. Deleterious effect of nitric oxide inhibition in chronic hepatopulmonary syndrome. Eur J Gastroenterol Hepatol 19(2007): 341–346.
- tiegmann GV, Goff JS, Michaletz-Onody PA, et al. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med 326(1992): 1527–1532.
- Garcia-Pagán JC, Bosch J. Endoscopic band ligation in the treatment of portal hypertension. Nat Clin Pract Gastroenterol Hepatol 2(2005): 526–535.
- Olson JC, Wendon JA, Kramer DJ, et al. Intensive care of the patient with cirrhosis. Hepatology 54(2011): 1864–1872.
