Changes in the Hepatic Artery Resistive Index After A Meal and Hypertension in Pregnancy: Case Report
Article Information
Mônica Gomes de Almeida1*, André Guayanaz Lauriano1, Renato Augusto Moreira de Sá2,3
1Department of Obstetrics, ‘Antônio Pedro’ University Hospital, Fluminense Federal University, Rio de Janeiro, Brazil
32Research Department, ‘Fernandes Figueira’ Institute, Rio de Janeiro, Brazil
3Department of Obstetrics of the Perinatal Group, Rio de Janeiro, Brazil
*Corresponding author: Mônica Gomes de Almeida, Hospital Universitário Antônio Pedro - Rua Marquês de Paraná 303, 8º andar - Niterói - Rio de Janeiro – Brazil
Received: 04 July 2019; Accepted: 16 July 2019; Published: 19 July 2019
Citation: Almeida MG, Lauriano AG, Sá RAM. Changes in the Hepatic Artery Resistive Index After A Meal and Hypertension in Pregnancy: Case Report. Cardiology and Cardiovascular Medicine 3 (2019): 140-144.
Share at FacebookAbstract
In liver disease, the hepatic artery resistive index while fasting is higher, and there is less postprandial increase than in healthy subjects. The liver is one of the many organs that may be affected by endothelial dysfunction, vasospasm and ischemia that occur in pre-eclampsia. We report ten cases with hepatic artery resistive index (RI) variations in normotensive and hypertensive pregnant women. There was an increase in the RI in normotensive women and a reduction in hypertensive women after a mixed meal and an increase in the RI of more than 10% among normotensive women who ingested glucose. It is feasible to use any of the solutions during pregnancy. However, the 75 g glucose solution has greater potential for clinical application because it is routinely used in the prenatal period to screen for gestational diabetes. The incorporation of Doppler velocimetry of the hepatic artery in prenatal care, combined with screening for diabetes mellitus, would provide a low-cost alternative for predicting the unfavorable progression of hypertension, which would be especially valuable in places with limited resources. New studies may confirm the hypothesis raised in this case report that, as occurs in other causes of liver disease, a lower variation in the postprandial RI is associated with a higher probability of an unfavorable pregnancy outcome in hypertensive patients.
Keywords
Hepatic artery; Resistive index; Hypertension
Article Details
Introduction
Hypertensive disorders lead to complications in 5-10% of pregnancies worldwide. Although pre-eclampsia and eclampsia are associated with an increased risk of complications, any type of hypertension during pregnancy can result in increased maternal and perinatal morbidity and mortality [1]. The liver is one of the many organs that may be affected by endothelial dysfunction, vasospasm and ischemia that occur in pre-eclampsia. The liver receives oxygen via two pathways: 50% through the portal vein and 50% through the hepatic artery. The portal vein receives blood from
the abdominal portion of the digestive tract, including the gallbladder, pancreas and spleen. Portal venous flow increases physiologically after a meal and is reduced when fasting, after physical exercise and under pathological conditions. The hepatic artery is able to compensate for changes in portal venous flow, increasing or decreasing its own flow, a mechanism known as the ‘hepatic arterial buffer response’. The purpose of this mechanism is to reduce the impact of portal flow variations on liver function [2]. After a meal, when there is an increase in portal venous flow, there is decrease in flow and increase in resistance in the hepatic artery [3-5]. The effect of a meal on portal circulation can be observed indirectly through studies on superior mesenteric artery flow before and after meals. A study on the effect of different types of foods on the mesenteric circulation in healthy individuals concluded that the ingestion of a mixed meal (carbohydrates, proteins and fats; 300 ml, 355 kcal) was associated with a greater increase in postprandial flow, while ingestion of 300 ml of carbohydrates (355 kcal) was associated with an earlier and lower increase [6]. Another study that compared the superior mesenteric artery flow variation in healthy individuals after the intake of isocaloric and isovolemic solutions of carbohydrates, fats, and proteins (400 ml, 400 kcal) concluded that the magnitude of the response to the different meal types was similar but that the maximum responses were reached earlier with carbohydrates than with proteins or fats [3]. Among resistance measurements, the RI is the most used for analysis of the hepatic artery and is calculated from the spectral Doppler waveform using the equation RI = (PSV-EDV)/PSV, where PSV corresponds to the peak systolic velocity and EDV to the end-diastolic velocity. The hepatic artery at rest is a vessel with a low RI, ranging from 0.55 to 0.81 [7]. These values are the same as those observed in healthy pregnant women [8-10]. Studies conducted in nonpregnant women that compared the hepatic artery RI before and after a meal in healthy individuals with liver disease showed that the greater the severity of the disease was, the higher the RI during fasting and the lower the postprandial variation [11]. Individuals with liver disease had a higher fasting RI than did healthy individuals. However, there was an overlap of the RI values for the two groups, which limits the application of absolute values for clinical decision-making and, hence, emphasizes the importance of analyzing pre- and postprandial variations [12].
Case Description
Aiming to assess the fasting hepatic artery RI and the postprandial variation in normotensive and hypertensive pregnant women, we report here a series of ten cases. The study was approved by the Research Ethics Committee of the University Hospital of Fluminense Federal University, Rio de Janeiro, Brazil, and the patients signed informed consent forms. The inclusion criteria were pregnant women with singleton pregnancy, between 24 and 34 gestational weeks, nonsmokers, with a body mass index lower than 30 kg/m2, normotensive, with chronic hypertension or pre-eclampsia. The hepatic artery RI was measured at two time-points: when fasting and 30 minutes after a meal. Two groups were formed according to the order of inclusion in the case report. The first five participants ingested 200 ml of a mixed solution containing 62.5 g/l protein, 202 g/l carbohydrate and 49.2 g/l lipid, and the five subsequent participants ingested 300 ml of a solution containing 75 grams of glucose. The common hepatic artery was accessed with the transducer placed in the subxiphoid position, close to its origin at the coeliac trunk, with the participants in a supine position. For each subject, the averages of three measurements of the vessel were considered, before and after the meal. All tests were performed by the same sonographer using a 2-5.2 MHz Voluson S6 convex transducer (GE Healthcare). The results of the hepatic artery RI measurements before and after meals are summarized in Table 1. We observed that
after ingestion of the mixed solution, the RI increased in normotensive pregnant women and decreased in hypertensive women. Among the cases that ingested the glucose solution, we observed an increase in the RI; this increase was greater than 10% among the normotensive women.
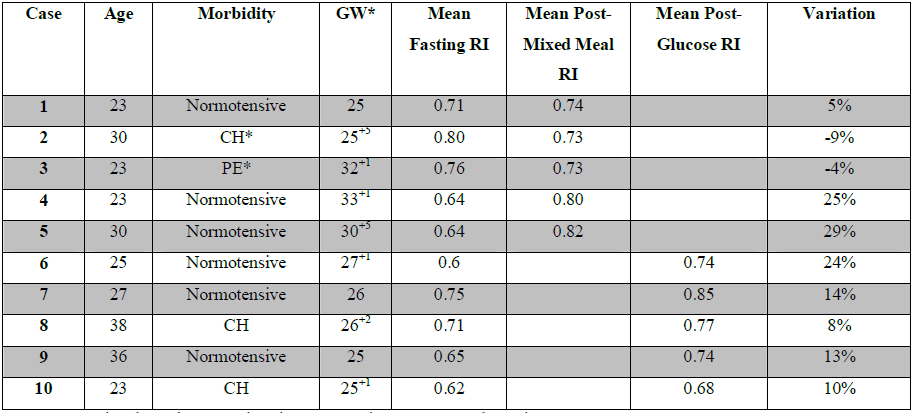
GW – Gestational Week; CH - Chronic Hypertension; PE - Pre-eclampsia
Table 1: Overview of cases according to the pregnant woman's age, morbidity, gestational week, meal type and fasting and postprandial hepatic artery RI.
Discussion
There are no published studies on pre- and postprandial variations in the hepatic artery RI in pregnant women. The study of hepatic circulation seems to have the potential to contribute to the monitoring of hypertensive pregnant women, according to studies correlating the reduction in fasting hepatic flow with pre-eclampsia and HELLP (hemolysis, elevated liver enzymes and low platelet) syndrome [13,14]. One study compared the pulsatility index (PI) of the common hepatic artery during fasting in three groups: healthy pregnant women, pregnant women with pre-eclampsia and pregnant women with HELLP syndrome. The PI was significantly higher in the groups with pre-eclampsia and HELLP syndrome than in the group of healthy pregnant women [9]. The evaluation of pre- and postprandial RI variations could help identify pregnant women at higher risk of developing severe forms of hypertensive disease, which would allow the establishment of different protocols for follow-up. There are studies on the correlation between demographic and pregnancy characteristics (such as gestational age), signs and symptoms of pre-eclampsia, blood pressure levels, laboratory tests and biomarkers for predicting adverse maternal outcomes in hypertension. However, the available studies are not conclusive, and there is a lack of indicators that can predict the progression to severe forms of the disease [15]. The study of these ten cases showed pre- and postprandial variation in the hepatic artery RI, both with the ingestion of a mixed meal and glucose. It is feasible to use any of the solutions during pregnancy; however, the 75 g glucose solution has greater potential for clinical application because it is
routinely used in the prenatal period to screen for gestational diabetes. Ultrasonography is a noninvasive method routinely used in prenatal care. The examination technique used in this case series has shown good intra- and interobserver reproducibility [16]. The incorporation of Doppler velocimetry of the hepatic artery in prenatal care, combined with screening for diabetes mellitus, would provide a low-cost alternative for predicting the unfavorable progression of hypertension, which would be especially valuable in places with limited financial resources. New studies may confirm the hypothesis raised in this case series that, as occurs in other causes of liver disease, a lower variation in the postprandial RI is associated with a higher probability of an unfavorable pregnancy outcome in hypertensive patients.
Acknowledgments
We thank the Municipal Health Foundation of Niterói, Rio de Janeiro, for the referral of pregnant women for the case series. We thank professor Dr. Fernanda C Silva, from the Federal University of the State of Rio de Janeiro, and the professors of the Escola de Ultrassonografia Rio de Janeiro (Ultrasound School of Rio de Janeiro), Dr. Eugênio PQ Ayres and Dr. Vitor M Marques, for providing training in hepatic artery Doppler velocimetry.
Conflicts of interest
None
References
- Magee LA, von Dadelszen P, Stones W, Mathai M. Introduction. In: Magee LA, von Dadelszen P, Stones W, Mathai M (ed).The FIGO textbook of Pregnancy Hypertension: An evidence-based guide to monitoring, prevention and management: The Global Library of Women’s Medicine, 2016.
- Eipel C, Abshagen K, Vollmar B. Regulation of hepatic blood flow: the hepatic arterial buffer response revisited. World J Gastroenterol 16 (2010): 6046-6057.
- 3 Qamar MI, Read AE. Effects of ingestion of carbohydrate, fat, protein, and water on the mesenteric blood flow in man. Scand J Gastroenterol 23 (1988): 26-30.
- Dauzat M, Lafortune M, Patriquin H, Pomier-Layargues G. Meal induced changes in hepatic and splanchnic circulation: a noninvasive Doppler study in normal humans. Eur J Appl Physiol 68 (1994): 373-380.
- Fisher A, Paulson EK, Kliewer MA, DeLong DM, Nelson RC. Doppler sonography of the portal vein and hepatic artery: measurement of a prandial effect in healthy subjects. Radiology 207 (1998): 711-715.
- Moneta GL, Taylor DC, Helton WS, Mulholland MW, Strandness Jr DE. Duplex ultrasound measurement of postprandial intestinal blood flow: effect of meal composition. Gastroenterology 95 (1988): 1294-301.
- McNaughton DA, Abu-Yousef MM. Doppler US of the Liver Made Simple. RadioGraphics 31 (2011): 161-188.
- Mandic-Markovic VD, Mikovic ZM, Djukic MK, Vasiljevic MD, Jankovic GL. Dopller parameters of the maternal hepatic artery blood flow in normal pregnancy: maternal hepatic artery blood flow in normal pregnancy. Eur J Obstet Gynecol Reprod Biol 181 (2014): 275-279.
- Oosterhof H, Voorhoeve PG, Aarnoudse JG. Enhancement of hepatic artery resistance to blood flow in preeclampsia in presence or absence of HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets). Am J Obstet Gynecol 171 (1994): 526-530.
- Nakai A, Sekiya I, Oya A, Koshino T, Araki T. Assessment of the hepatic arterial and portal venous blood flows during pregnancy with Doppler ultrasonography. Arch Gynaecol Obstet 266 (2002): 25-29.
- Numata K, Tanaka K, Kiba T, Mitsui K, Saito S, Sekihara H. Hemodynamic changes in hepatic artery after glucose ingestion in healthy subjects and patients with cirrhosis. J Clin Ultrasound 26 (1998): 137-42.
- Joynt L K, Platt JF, Rubin JM, Ellis JH, Bride RO. Hepatic artery resistance before and after standard meal in subjects with diseased and healthy livers. Radiology 196 (1995): 489-492.
- Kawabata I, Nakai A, Takeshita T. Prediction of HELLP syndrome with assessment of maternal dual hepatic blood supply by using Doppler ultrasound. Arch Gynecol Obstet 274 (2006): 303-309.
- Nasr A, Nafeh H. Decreased hepatic perfusion in patients with HELLP syndrome. J Obstet Gynaecol 29 (2009): 624-627.
- Ukah, UV, De Silva DA, Payne B et al. Prediction of adverse maternal outcomes from pre-eclampsia and other hypertensive disorders of pregnancy: A systematic review. Pregnancy Hypertens 11 (2017): 115-123.
- Aires EPQ, Almeida MG, Marques VM, Silva FC, Sá RAM, Velarde GC. A novel technique for the assessment of total liver blood flow in pregnancy: interrater and intrarater agreements. Br J Radiol 90 (2017): 20160805
