Carotid Body Tumour Misdiagnosed as a Traumatic Carotid Pseudoaneurysm
Article Information
Harvey J1,2*, Boles B1,3, Ipeson K1
Department of Radiology, Townsville Hospital, Douglas, Queensland, Australia
*Corresponding Author: Dr. James Harvey, Department of Radiology, Townsville Hospital, Douglas, Queensland, Australia
Received: 16 March 2020; Accepted: 02 April 2020; Published: 09 April 2020
Citation: Harvey J, Boles B, Ipeson K. Carotid Body Tumour Misdiagnosed as a Traumatic Carotid Pseudoaneurysm. Journal of Radiology and Clinical Imaging 3 (2020): 050-055.
Share at FacebookAbstract
Blunt carotid injury that occurs as a result of near-hanging or strangulation carries a significant morbidity as a result of subsequent ischaemic stroke. Clinical examination is poorly predictive in identifying patients with vascular injuries and imaging plays a central role in screening these patients in the emergency setting. We present the case of young woman who presented to the emergency department following near-hanging. CT angiogram examination of the neck demonstrated an enhancing focus at the carotid bifurcation which was initially misidentified as a carotid artery pseudoaneurysm. Ultrasound demonstrated absence of flow within the mass which was interpreted as thrombosis of the pseudoaneurysm. Following an unsuccessful attempt at embolisation, the imaging was reviewed and the correct diagnosis of a carotid body tumour reached. Differentials for an enhancing mass within the carotid space include a pseudoaneurysm, carotid body tumour, enhancing lymph node, schwannoma or neurofibroma. General radiologists should be aware of the imaging distinctions between these carotid space pathologies.
Keywords
Carotid body tumour; Paraganglioma; Pseudoaneurysm; Trauma; Carotid bifurcation
Carotid body tumour articles, Paraganglioma articles, Pseudoaneurysm articles, Trauma articles, Carotid bifurcation articles
Carotid body tumour articles Carotid body tumour Research articles Carotid body tumour review articles Carotid body tumour PubMed articles Carotid body tumour PubMed Central articles Carotid body tumour 2023 articles Carotid body tumour 2024 articles Carotid body tumour Scopus articles Carotid body tumour impact factor journals Carotid body tumour Scopus journals Carotid body tumour PubMed journals Carotid body tumour medical journals Carotid body tumour free journals Carotid body tumour best journals Carotid body tumour top journals Carotid body tumour free medical journals Carotid body tumour famous journals Carotid body tumour Google Scholar indexed journals Paraganglioma articles Paraganglioma Research articles Paraganglioma review articles Paraganglioma PubMed articles Paraganglioma PubMed Central articles Paraganglioma 2023 articles Paraganglioma 2024 articles Paraganglioma Scopus articles Paraganglioma impact factor journals Paraganglioma Scopus journals Paraganglioma PubMed journals Paraganglioma medical journals Paraganglioma free journals Paraganglioma best journals Paraganglioma top journals Paraganglioma free medical journals Paraganglioma famous journals Paraganglioma Google Scholar indexed journals Pseudoaneurysm articles Pseudoaneurysm Research articles Pseudoaneurysm review articles Pseudoaneurysm PubMed articles Pseudoaneurysm PubMed Central articles Pseudoaneurysm 2023 articles Pseudoaneurysm 2024 articles Pseudoaneurysm Scopus articles Pseudoaneurysm impact factor journals Pseudoaneurysm Scopus journals Pseudoaneurysm PubMed journals Pseudoaneurysm medical journals Pseudoaneurysm free journals Pseudoaneurysm best journals Pseudoaneurysm top journals Pseudoaneurysm free medical journals Pseudoaneurysm famous journals Pseudoaneurysm Google Scholar indexed journals Trauma articles Trauma Research articles Trauma review articles Trauma PubMed articles Trauma PubMed Central articles Trauma 2023 articles Trauma 2024 articles Trauma Scopus articles Trauma impact factor journals Trauma Scopus journals Trauma PubMed journals Trauma medical journals Trauma free journals Trauma best journals Trauma top journals Trauma free medical journals Trauma famous journals Trauma Google Scholar indexed journals Carotid bifurcation articles Carotid bifurcation Research articles Carotid bifurcation review articles Carotid bifurcation PubMed articles Carotid bifurcation PubMed Central articles Carotid bifurcation 2023 articles Carotid bifurcation 2024 articles Carotid bifurcation Scopus articles Carotid bifurcation impact factor journals Carotid bifurcation Scopus journals Carotid bifurcation PubMed journals Carotid bifurcation medical journals Carotid bifurcation free journals Carotid bifurcation best journals Carotid bifurcation top journals Carotid bifurcation free medical journals Carotid bifurcation famous journals Carotid bifurcation Google Scholar indexed journals Computer Tomography articles Computer Tomography Research articles Computer Tomography review articles Computer Tomography PubMed articles Computer Tomography PubMed Central articles Computer Tomography 2023 articles Computer Tomography 2024 articles Computer Tomography Scopus articles Computer Tomography impact factor journals Computer Tomography Scopus journals Computer Tomography PubMed journals Computer Tomography medical journals Computer Tomography free journals Computer Tomography best journals Computer Tomography top journals Computer Tomography free medical journals Computer Tomography famous journals Computer Tomography Google Scholar indexed journals vascular neuroendocrine tumour articles vascular neuroendocrine tumour Research articles vascular neuroendocrine tumour review articles vascular neuroendocrine tumour PubMed articles vascular neuroendocrine tumour PubMed Central articles vascular neuroendocrine tumour 2023 articles vascular neuroendocrine tumour 2024 articles vascular neuroendocrine tumour Scopus articles vascular neuroendocrine tumour impact factor journals vascular neuroendocrine tumour Scopus journals vascular neuroendocrine tumour PubMed journals vascular neuroendocrine tumour medical journals vascular neuroendocrine tumour free journals vascular neuroendocrine tumour best journals vascular neuroendocrine tumour top journals vascular neuroendocrine tumour free medical journals vascular neuroendocrine tumour famous journals vascular neuroendocrine tumour Google Scholar indexed journals vascular injury articles vascular injury Research articles vascular injury review articles vascular injury PubMed articles vascular injury PubMed Central articles vascular injury 2023 articles vascular injury 2024 articles vascular injury Scopus articles vascular injury impact factor journals vascular injury Scopus journals vascular injury PubMed journals vascular injury medical journals vascular injury free journals vascular injury best journals vascular injury top journals vascular injury free medical journals vascular injury famous journals vascular injury Google Scholar indexed journals carotid articles carotid Research articles carotid review articles carotid PubMed articles carotid PubMed Central articles carotid 2023 articles carotid 2024 articles carotid Scopus articles carotid impact factor journals carotid Scopus journals carotid PubMed journals carotid medical journals carotid free journals carotid best journals carotid top journals carotid free medical journals carotid famous journals carotid Google Scholar indexed journals vertebral arteries articles vertebral arteries Research articles vertebral arteries review articles vertebral arteries PubMed articles vertebral arteries PubMed Central articles vertebral arteries 2023 articles vertebral arteries 2024 articles vertebral arteries Scopus articles vertebral arteries impact factor journals vertebral arteries Scopus journals vertebral arteries PubMed journals vertebral arteries medical journals vertebral arteries free journals vertebral arteries best journals vertebral arteries top journals vertebral arteries free medical journals vertebral arteries famous journals vertebral arteries Google Scholar indexed journals
Article Details
1. Case Presentation
A 24-year-old woman was brought to the emergency department following a suicide attempt through hanging. She was cut down and two rescue breaths were administered. GCS was 15 at the scene. Due to agitation, she was sedated to facilitate transfer. A feint ligature mark was evident on the anterior neck. Arterial phase CT neck was performed to investigate for a vascular injury. An enhancing focus was seen adjacent to to the left carotid bulb. Delayed phase imaging was subsequently performed.
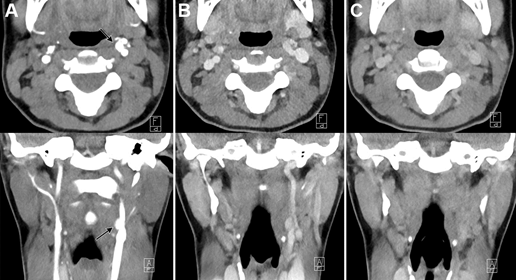
Figure 1: CT neck with axial and coronal projections. A (arterial phase), B (60 second delay) and C (3 minute delay) demonstrated a 6 x 8 mm contrast-enhancing structure anteromedial to the left carotid bulb. Appearance was compatible with extraluminal contrast leak.
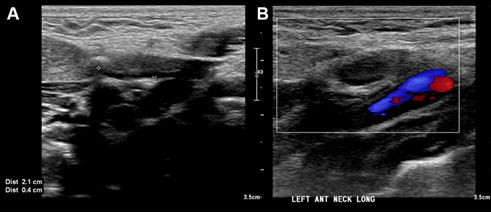
Figure 2: Ultrasound demonstrated an ill-defined abnormality posterior to the common carotid artery which was suspicious for a thrombosed pseudoaneurysm arising from the external carotid artery.
The patient was transferred to a tertiary centre for vascular surgery review and underwent angiogram to investigate the presumed traumatic carotid artery injury.
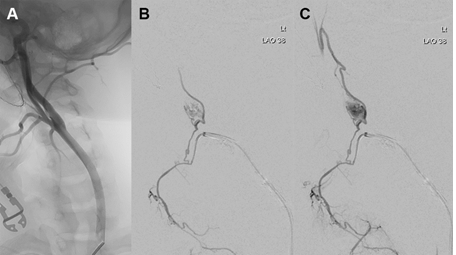
Figure 3: A: Left common carotid angiogram did not show a pseudoaneurysm. B, C: selective angiogram of the left external carotid artery demonstrated a mass arising from a branch of the superior thyroid artery. Unsuccessful attempts were made to coil the vessel before the procedure was abandoned.
Due to the small size of the tumour, MR imaging was non-contributory.
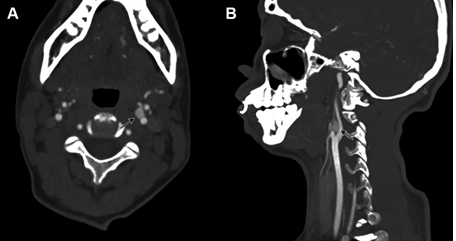
Figure 4: A (axial), B (sagittal). On review of the initial presentation CT, with appropriate windowing, the mass is seen to incompletely follow the arterial pool. The feeding branch arising from the superior thyroid artery is evident anterior to the mass.
2. Discussion
Near-hanging and strangulation may result in arterial dissections, haematoma, stenosis or pseudoaneurysm formation involving the carotid or vertebral arteries. These injuries are poorly predicted based on examination alone, mandating a low-threshold for radiological evaluation in patients presenting following high-risk mechanisms. Arterial injury is not uncommon, occurring in 2% of non-fatal hangings [1]. Treatment is intended to minimise the risk of ischaemic stroke, which occurs in half of untreated patients with blunt carotid artery injuries. Where patients do become symptomatic following traumatic carotid artery injury, neurological defect was identified an average of 10-72 hours following patient presentation in one study. Anticoagulation remains the mainstay of therapy, however endovascular treatments are becoming increasingly commonplace in managing these injuries [2].
Arterial-phase CT is the most frequently performed investigation in the emergency setting. Sensitivity of CT in detecting blunt carotid injuries is reported between 82% and 100% when compared with the gold-standard conventional angiogram. Modern CT scanners with 16-64 channel technology demonstrate higher sensitivities and specificities, allowing the detecting of almost all clinically significant blunt vascular injuries [3, 4]. CT has the additional advantage of identifying associated injuries, and in particular cervical spine fractures, which occur more commonly than vascular injuries.
No direct comparison between the sensitivity of CT or ultrasound in the detection of traumatic vascular injuries have been reported. The portability of ultrasound means that it can be employed at the bedside to rapidly assess the unstable patient. The lack of need for intravenous contrast also provides an advantage in patients where contrast is contraindicated. Despite these advantages, interobserver variability and difficulty in visualising the entire vertebral arteries limits its use in the emergency setting [5]. Sensitivities between MRI and CT appear comparable but scanning time and availability currently make MRI impractical in screening unstable patients [4].
The differentials for an enhancing mass at the carotid bifurcation include a carotid body tumour, lymph node, schwannoma or neurofibroma arising from the lower four cranial nerves, carotid sheath meningioma and carotid pseudoaneurysm [6-8]. Enhancing lymph nodes should prompt consideration of thyroid malignancy or squamous cell carcinoma of the head or neck. Large lesions centred within the carotid space will displace the ipsilateral parapharyngeal fat anteromedially. Second brachial cleft cysts external to the carotid sheath may also have a similar location [6].
Carotid body tumours are rare, highly vascular neuroendocrine tumours that arise from the paraganglion cells of the carotid body. Incidence is estimated at 1-2 per 100,000 with presentation most common within the fifth and sixth decades, with a slight female predominance described [9]. The majority of tumours are asymptomatic, being diagnosed incidentally on imaging or presenting as a painless, rubbery masses in the lateral neck. Where symptomatic, patients may present with dysphagia, odynophagia or hoarseness of voice due to compression of the adjacent glossopharyngeal or vagus nerve [10]. Paragangliomas may be treated surgically or with radiation. Risk of vascular injury and nerve damage increases with tumour size and hence radiation therapy is typically reserved for extensive tumours where surgical would result in significant morbidity [11, 12]. As 10% of cases are malignant and aggressive lesions are poorly differentiated from benign lesions on imaging, long-term follow-up is mandated where resection is not performed.
When large, these tumours classically splay the internal and external carotid arteries. They display rapid enhancement on arterial phase CT [10]. On MRI, they classically demonstrate a 'salt and pepper' appearance on T1 with areas of punctate high intensity areas due to haemorrhage and low intensity areas due to flow voids [13, 14]. The lesions are usually higher signal than muscle on T2. Schwannomas and neurofibromas are generally slightly less avidly enhancing than paragangliomas. Schwannomas may demonstrate a target sign with high T2 signal peripherally and central hypointensity [6].
In this case, the site of the enhancing focus is typical of a carotid body tumour location. The mass did not completely match arterial phase enhancement on CT and the walls of both the internal and external artery appeared intact, without thrombus or other secondary features of traumatic injury. Additionally, the absence of internal vascularity on Doppler ultrasound mandates consideration of a solid lesion in addition to a thrombosed pseudoaneurysm. The majority of carotid body lesions are supplied by the ascending pharyngeal artery or via other branches of the external carotid artery and as such, the presence of a large vessel arising from the external carotid artery should also raise suspicion for a mass rather than a vascular injury [15].
This case also highlights the importance of appropriate windowing in vascular studies. An initial radiological diagnosis of a mass is likely to have prevented this patient from undergoing an unnecessary angiogram.
References
- Martin MJ, Weng J, Demetriades D, Salim A. Patterns of injury and functional outcome after hanging: analysis of the National Trauma Data Bank. Am J Surg 90 (2005): 836-840.
- Shahan CP, Sharpe JP, Stickley SM, et al. The changing role of endovascular stenting for blunt cerebrovascular injuries. J Trauma Acute Care Surg 84 (2018): 308-311.
- Paulus EM, Fabian TC, Savage SA, et al. Blunt cerebrovascular injury screening with 64-channel multidetector computed tomography: more slices finally cut it. Journal of Trauma and Acute Care Surgery 76 (2014): 279-285.
- Brommeland T, Helseth E, Aarhus M, et al. Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med 26 (2018): 90.
- Nagpal P, Policeni B, Bathla G, et al. Blunt cerebrovascular injuries: advances in screening, imaging, and management trends. American Journal of Neuroradiology 39 (2018): 406-414.
- Chengazi HU, Bhatt AA. Pathology of the carotid space. Insights into imaging 10 (2019): 10-21.
- Ibeh C, Potigailo V. Enhancing carotid space mass. J Am Osteopath Coll Radiol 4 (2015): 24-26.
- Kuwada C, Mannion K, Aulino JM, et al. Imaging of the carotid space. Otolaryngol Clin North Am 45 (2012): 1273-1292.
- Dua A, Spees TC, Hernandez FC, et al. Trends in the incidence of carotid body tumors in the United States from 1998 to 2011. Vasc Dis Manag 11 (2014): E298-E302.
- Wieneke JA, Smith A. Paraganglioma: carotid body tumor. Head and neck pathology 3 (2009): 303-306.
- Gad A, Sayed A, Elwan H, et al. Carotid body tumors: a review of 25 years experience in diagnosis and management of 56 tumors. Ann Vasc Dis 7 (2014): 292-299.
- Pacheco-Ojeda LA. Carotid body tumors: Surgical experience in 215 cases. Journal of Cranio-Maxillofacial Surgery 45 (2017): 1472-1477.
- Baez JC, Jagannathan JP, Krajewski K, et al. Pheochromocytoma and paraganglioma: imaging characteristics. Cancer Imaging 12 (2012): 153.
- Lee KY, Oh YW, Noh HJ, et al. Extraadrenal paragangliomas of the body: imaging features. AJR Am J Roentgenol 187 (2006): 492-504.
- Van den Berg R, Rodesch G, Lasjaunias P. Management of paragangliomas. Clinical and angiographic aspects. Interventional neuroradiology: journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences 8 (2002): 127-134.
