Bloody Mystery After Vomiting
Article Information
Maryam Naser1, Farbod Nasseri2, Nafiseh Hashemi1,*
1Hashemi Eye Care, Encino, CA, USA
2Renaissance Imagine Medical Associates, Northridge, CA, USA
Corresponding Author: Nafiseh Hashemi, MD, Hashemi Eye Care, 5353 Balboa Blvd #110, Encino, CA, 91316, USA
Received: 23 July 2020; Accepted: 31 July 2020; Published: 03 August 2020
Citation: Maryam Naser, Farbod Nasseri, Nafiseh Hashemi. Bloody Mystery After Vomiting. Journal of Ophthalmology and Research 3 (2020): 38-40.
Share at FacebookAbstract
Abstract
A 71-year-old Asian female was referred to neuro-ophthalmology clinic with a history of redness in the right eye for six months and recent vision loss. There was a history of severe vomiting few months ago. The patient developed red eye following vomiting, which has been treated as conjunctivitis for few months with no improvement. After 6 months she noticed vision loss in the right eye because of CRVO. MRI brain showed carotidcavernous fistula.
Keywords
Carotid-Cavernous Fistula; Central Retinal Vein Occlusion; Chronic Red Eye; Proptosis; Vomiting; Double Vision
Article Details
Case Report:
A 71-year-old Asian female presented to neuro-ophthalmology clinic reporting redness in right eye and vision loss. Patient had redness in the right eye for 6 months. She was diagnosed and treated for infectious and allergic conjunctivitis with no improvement in redness. The patient states the redness started following severe retching and vomiting due to allergic reaction to Doxycycline which took her to ER in December 2019. Her initial evaluation was reported unremarkable. She had no history of eye problem and never had MRI brain before. The patient noticed her vision in right eye decreased since a week prior to presentation to neuro-ophthalmology clinic. She was complaining of redness and pressure feeling behind the right eye, proptosis, and lid edema for the last 6 months.
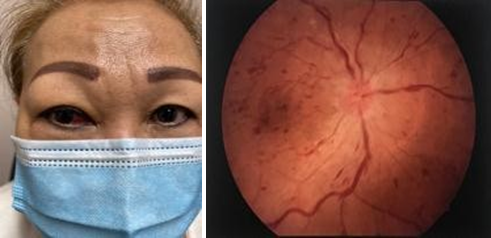
On eye exam, she has decreased vision in the right eye to 20/70. There is RAPD right eye. She has vertical double vision in up-gaze because of limitation in elevation right superior rectus muscle. Hertal exophthalmometry shows proptosis of the right eye (base:100, OD:18, OS:16). IOP is 19 OD and 16 OS. On slit lamp exam, there is corkscrew blood vessels nasally (Figure 1). Funds exam shows optic nerve swelling and widespread intraretinal hemorrhage (Figure 2).
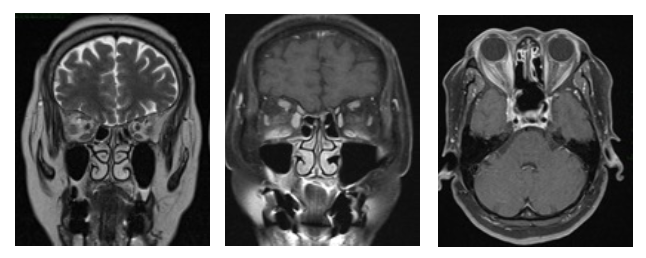
The patient had central retinal vein occlusion (CRVO) in the right eye due to inadequate drainage of the venous flow in the context of arteriovenous fistula. OCT macula shows macular edema. MRI brain and orbit was requested which confirmed CCF. The radiologic figures are including enlarged SOV on the right side (Figure 3), enlarged right medial rectus muscle (Figure 4), mild right proptosis and intraorbital fat infiltration (Figure 5). The patient was referred to interventional neurologist for treatment of CCF as well as retina specialist for treatment of CRVO.
Discussion
Carotid cavernous fistulas (CCFs) are abnormal arteriovenous connection that cause blood to flow from the carotid artery system into to the cavernous sinus directly or indirectly [1]. Etiologically, about 70 to 75% of CCFs can occur following trauma, such as base of skull fractures, accidents or iatrogenic injuries, which usually are shown in young males with high flow and direct fistulas. The remainder of CCFs occur spontaneously which are usually predisposed by genetic disorders or aneurysm rupture that are common in older females with low flow indirect fistula [2]. Differential diagnosis of CCF include orbital pathologies such as infection, inflammation, hemorrhage, tumor or vasculitis and thyroid eye disease. Patients with CCF may present with pulsatile exophthalmos, orbital bruit, diplopia, vision loss, limitation in eye movements, ptosis, eyelid edema, ringing in ears, and headache. The patient with episcleral congestion and chemosis may falsely get diagnosed with conjunctivitis or scleritis. High pressure in vortex and episcleral veins may result in elevated intraocular pressures and secondary glaucoma [3,4,5]. A retrospective study on signs and symptoms of 80 cases with CCF reported 93% with arterialization of conjunctival vein, 84% proptosis, 42% chemosis, 52% cranial nerve palsy, 51% elevated IOP and 31% optic neuropathy. Vision loss differed from 20/40 to no light perception [6]. We reported a case of CCF presents with CRVO. The patient’s chronic red eye and pressure feeling should have been a clue to her timely diagnosis to avoid her vision loss. In our case severe retching and vomiting is the suspected cause for the fistula. Taking accurate history and detailed examination, proper diagnostic tests and imaging and high clinical suspicion are key in timely diagnosis for the treatment of this disease.
Disclosure Statement
The Authors do not have any financial disclosures
Funding Sources:
None
References:
- Ellis JA, Goldstein H, Connolly ES, et al. Carotid-cavernous fistulas. Neurosurgical Focus 32 (2012): E9.
- Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye 32 (2018): 164-172.
- Bhatti MT, Peters KR. A red eye and then a really red eye. Survey of Ophthalmology 48 (2003): 224-229.
- Talks SJ, Salmon JF, Elston JS, et al. Cavernous-dural fistula with secondary angle-closure glaucoma. American Journal of Ophthalmology 124 (1997): 851-853.
- Buus DR, David TT, Parrish RK. Spontaneous carotid cavernous fistula presenting with acute angle closure glaucoma. Archives of Ophthalmology 107 (1989): 596-597.
- Preechawat P, Narmkerd P, Jiarakongmun P, et al. Dural carotid cavernous sinus fistula: ocular characteristics, endovascular management and clinical outcome. Medical Journal of the Medical Association of Thailand 91 (2008): 852.