Blood Pressure Discrepancy and Pulse Differential in Patients Undergoing CT Angiography for Suspected Acute Aortic Dissection
Article Information
Lucas Stefanelli*, Courtney Abbott, Michael Sloan, Angus Hartery
Discipline of Radiology, Faculty of Medicine, Memorial University of Newfoundland, Elizabeth Ave, St. John's, NL A1C 5S7, Canada
*Corresponding Author: Lucas Stefanelli, Discipline of Radiology, Faculty of Medicine, Memorial University of Newfoundland, Elizabeth Ave, St. John's, NL A1C 5S7, Canada.
Received: 02 November 2022; Accepted: 17 November 2022; Published: 25 November 2022
Citation:
Stefanelli L, Abbott C, Sloan M, Hartery A. Blood Pressure Discrepancy and Pulse Differential in Patients Undergoing CT Angiography for Suspected Acute Aortic Dissection. Journal of Radiology and Clinical Imaging 5 (2022): 53-64.
Share at FacebookAbstract
Purpose: To determine if blood pressure discrepancy between arms, pulse pressure, or other patient characteristics are more common in patients diagnosed with acute aortic dissection than those without, as confirmed on computed tomography angiography.
Methods: A retrospective chart review was conducted for patients who had undergone CTA for possible acute aortic dissection in Newfoundland and Labrador from 2012-2019. Each CTA-positive participant was sex, age (+/- 2 years), and technology-matched with CTA-negative controls.
Results: 61 participants met all inclusion criteria. Blood pressure discrepancy was not significant between acute aortic dissection types or between genders, with no impact on mortality rates. Pulse pressure was significantly higher in Stanford Type B aortic dissection (STB) than Stanford Type A Aortic Dissections (STA). Lower pulse pressures had lower mortality rates for STB respondents only. Abdominal pain was more frequent in STB than STA. Females with abdominal pain or back pain had increased mortality rates. Syncope was more common in STA than STB. Males with syncope had increased mortality rates. STA males had significantly increased mortality, while STB males had decreased mortality across all time points.
Conclusion: This was the first study to compare blood pressure differentials and pulse pressures together in conjunction with age-, sex- , and technology-matched controls, and the first to break these findings down further by AAD type and sex. Our findings demonstrate previously unidentified symptom- and sex-specific factors which could be invaluable in initial assessment and triage.
Aortic dissection articles; Pulse Pressure articles; Blood pressure discrepancy articles
Stanford Type B aortic dissection articles Stanford Type B aortic dissection Research articles Stanford Type B aortic dissection review articles Stanford Type B aortic dissection PubMed articles Stanford Type B aortic dissection PubMed Central articles Stanford Type B aortic dissection 2023 articles Stanford Type B aortic dissection 2024 articles Stanford Type B aortic dissection Scopus articles Stanford Type B aortic dissection impact factor journals Stanford Type B aortic dissection Scopus journals Stanford Type B aortic dissection PubMed journals Stanford Type B aortic dissection medical journals Stanford Type B aortic dissection free journals Stanford Type B aortic dissection best journals Stanford Type B aortic dissection top journals Stanford Type B aortic dissection free medical journals Stanford Type B aortic dissection famous journals Stanford Type B aortic dissection Google Scholar indexed journals Acute Aortic Dissection articles Acute Aortic Dissection Research articles Acute Aortic Dissection review articles Acute Aortic Dissection PubMed articles Acute Aortic Dissection PubMed Central articles Acute Aortic Dissection 2023 articles Acute Aortic Dissection 2024 articles Acute Aortic Dissection Scopus articles Acute Aortic Dissection impact factor journals Acute Aortic Dissection Scopus journals Acute Aortic Dissection PubMed journals Acute Aortic Dissection medical journals Acute Aortic Dissection free journals Acute Aortic Dissection best journals Acute Aortic Dissection top journals Acute Aortic Dissection free medical journals Acute Aortic Dissection famous journals Acute Aortic Dissection Google Scholar indexed journals Stanford Type A Aortic Dissections articles Stanford Type A Aortic Dissections Research articles Stanford Type A Aortic Dissections review articles Stanford Type A Aortic Dissections PubMed articles Stanford Type A Aortic Dissections PubMed Central articles Stanford Type A Aortic Dissections 2023 articles Stanford Type A Aortic Dissections 2024 articles Stanford Type A Aortic Dissections Scopus articles Stanford Type A Aortic Dissections impact factor journals Stanford Type A Aortic Dissections Scopus journals Stanford Type A Aortic Dissections PubMed journals Stanford Type A Aortic Dissections medical journals Stanford Type A Aortic Dissections free journals Stanford Type A Aortic Dissections best journals Stanford Type A Aortic Dissections top journals Stanford Type A Aortic Dissections free medical journals Stanford Type A Aortic Dissections famous journals Stanford Type A Aortic Dissections Google Scholar indexed journals Aortic Dissection Detection – Risk Score articles Aortic Dissection Detection – Risk Score Research articles Aortic Dissection Detection – Risk Score review articles Aortic Dissection Detection – Risk Score PubMed articles Aortic Dissection Detection – Risk Score PubMed Central articles Aortic Dissection Detection – Risk Score 2023 articles Aortic Dissection Detection – Risk Score 2024 articles Aortic Dissection Detection – Risk Score Scopus articles Aortic Dissection Detection – Risk Score impact factor journals Aortic Dissection Detection – Risk Score Scopus journals Aortic Dissection Detection – Risk Score PubMed journals Aortic Dissection Detection – Risk Score medical journals Aortic Dissection Detection – Risk Score free journals Aortic Dissection Detection – Risk Score best journals Aortic Dissection Detection – Risk Score top journals Aortic Dissection Detection – Risk Score free medical journals Aortic Dissection Detection – Risk Score famous journals Aortic Dissection Detection – Risk Score Google Scholar indexed journals CT Angiography articles CT Angiography Research articles CT Angiography review articles CT Angiography PubMed articles CT Angiography PubMed Central articles CT Angiography 2023 articles CT Angiography 2024 articles CT Angiography Scopus articles CT Angiography impact factor journals CT Angiography Scopus journals CT Angiography PubMed journals CT Angiography medical journals CT Angiography free journals CT Angiography best journals CT Angiography top journals CT Angiography free medical journals CT Angiography famous journals CT Angiography Google Scholar indexed journals Picture Archiving Communications System articles Picture Archiving Communications System Research articles Picture Archiving Communications System review articles Picture Archiving Communications System PubMed articles Picture Archiving Communications System PubMed Central articles Picture Archiving Communications System 2023 articles Picture Archiving Communications System 2024 articles Picture Archiving Communications System Scopus articles Picture Archiving Communications System impact factor journals Picture Archiving Communications System Scopus journals Picture Archiving Communications System PubMed journals Picture Archiving Communications System medical journals Picture Archiving Communications System free journals Picture Archiving Communications System best journals Picture Archiving Communications System top journals Picture Archiving Communications System free medical journals Picture Archiving Communications System famous journals Picture Archiving Communications System Google Scholar indexed journals CT scanner articles CT scanner Research articles CT scanner review articles CT scanner PubMed articles CT scanner PubMed Central articles CT scanner 2023 articles CT scanner 2024 articles CT scanner Scopus articles CT scanner impact factor journals CT scanner Scopus journals CT scanner PubMed journals CT scanner medical journals CT scanner free journals CT scanner best journals CT scanner top journals CT scanner free medical journals CT scanner famous journals CT scanner Google Scholar indexed journals Systolic Blood Pressure articles Systolic Blood Pressure Research articles Systolic Blood Pressure review articles Systolic Blood Pressure PubMed articles Systolic Blood Pressure PubMed Central articles Systolic Blood Pressure 2023 articles Systolic Blood Pressure 2024 articles Systolic Blood Pressure Scopus articles Systolic Blood Pressure impact factor journals Systolic Blood Pressure Scopus journals Systolic Blood Pressure PubMed journals Systolic Blood Pressure medical journals Systolic Blood Pressure free journals Systolic Blood Pressure best journals Systolic Blood Pressure top journals Systolic Blood Pressure free medical journals Systolic Blood Pressure famous journals Systolic Blood Pressure Google Scholar indexed journals
Article Details
1. Introduction
Acute Aortic Dissection (AAD) is a serious, potentially fatal condition which is the result of a tear in the intimal lining of the aorta. Prompt diagnosis is critical as mortality can reach 40-50% within 48 hours if untreated and increases with time. The classic presentation of AAD is one of immediate onset, tearing or ripping chest or back pain. If the dissection involves any of the aortic arch branch vessels, there may be neurologic, upper extremity, or other symptoms [1,2].
Clinical decision tools, such as the Aortic Dissection Detection – Risk Score (ADD-RS) aim to provide guidance on when to pursue advanced imaging when AAD is suspected. These have not been well adopted, and thus imaging for AAD is essentially at the discretion of the ordering physician [3].
A classic physical examination finding associated with AAD is that of blood pressure discrepancies between arms, typically greater than 20mmHg systolic. While blood pressures between arms may be equal on presentation [4], discrepancies can be a clinical sign of AAD [5,6]. Abnormal pulse pressure, or the difference between systolic and diastolic blood pressure unilaterally, is also described as a clinically relevant predictor of AAD [1]. It is unclear if the above findings are more common in patients who have AAD diagnosed on CT Angiography (CTA) vs. those who test negative for dissection on CTA.
Few studies have examined the presence of these findings in the context of the radiologic diagnosis of AAD. AAD is a difficult diagnosis to make clinically as the typical symptoms occur more frequently in other, more common disorders such as myocardial infarction. Ultimately, the diagnosis of AAD is made or confirmed with CTA of the entire aorta. This CT examination is relatively resource intensive in that it involves both a non-contrast examination of the chest, abdomen, and pelvis, followed by an arterial phase contrast-enhanced examination of the same regions. While the examination of the aorta can be completed quickly, the entirety of the chest, abdomen, and pelvis must be examined in two phases. Given that a lot of organ systems are examined, there are often incidental findings requiring additional work up and there is also the risk of false-positive diagnosis which can further contribute to patient anxiety and iatrogenic harms [7].
In a time of rising healthcare costs, the judicious use of diagnostic imaging should be considered an important part of healthcare sustainability. Gaining a better understanding of the physical examination findings in patients diagnosed with AAD may help lead to better clinical decision making and more appropriate use of imaging.
2. Methods
2.1 Participant Selection
This study was a retrospective quantitative analysis and chart review of patients who have undergone CTA for possible AAD in Newfoundland and Labrador from 2012-2019 (inclusive). This study was approved by the provincial Health Research Ethics Board (HREB) of Newfoundland and Labrador (approval number 20210572). mPower (Nuance Communications, UK) was used to search through a local radiology report database, including reports from 2012-2019 inclusive. Search terms including “aortic dissection”, “dissection” were used to identify CTA exams and thus participants for inclusion. CTAs performed which ruled in AAD (Presenting-Positive, PP) were included as study participants. CTAs performed which ruled out AAD (Presenting Negative, PN) were included as potential controls.
Participants were excluded if the positive CTA was performed outside of the date range, outside of our catchment population for screening purposes and non-acute indications such as family history, follow ups or because of surgical complications.
Once the final subset of presenting positive patients was identified, patient records and PACS (Picture Archiving Communications System) were used to collect pre-determined additional variables for each.
Data collected from the above medical records included health record numbers, CT scanner used, blood pressures and pulse pressures at presentation, symptoms at presentation, final diagnosis, incidental findings and date of death (if any). Stanford Type A and B AAD were defined as using the Stanford criteria, such that Stanford type A AAD (STA) refers to any nontraumatic dissection involving the ascending aorta while Stanford Type B AAD (STB) excludes the ascending aorta, presenting within 14 days of symptom onset [8]. Blood pressure differential was defined as the difference between the right arm and left arm systolic blood pressures. Pulse pressure was defined as the difference between the systolic and diastolic blood pressures unilaterally.
The final subset of participants was sex-matched, age-matched (+/- 2 years), and technology-matched (CT scanner used) with presenting-negative controls. Five CT scanners were identified and utilized over the inclusion period, 2 GE lightspeed VCT, 2 Toshiba Aquilion and a Phillips ICT. Presenting-positive participants were matched with presenting-negative participants who had had their imaging completed on the same CT scanner, as to avoid any undue influence of difference in imaging software and technology. Similar variables of interest were collected for the final control participants.
2.2 Data analysis
All analyses were performed using SPSS version 27.0 (IBM, Inc., Chicago, Illinois, USA). Descriptive statistics were performed for all variables. Continuous variables were expressed as means (standard deviation) and categorical variables as number of participants (percentages). Patient demographics were compared between groups. Continuous variables were analyzed using Student’s t test for normally distributed data while a nonparametric test of medians was used to compare continuous variables with skewed distributions. Chi-squared analysis was utilized for comparing categorical variables or Fisher’s exact test where appropriate. For in-hospital mortality and mortality at 1, 3, and 6 months, adjusted odds ratios were constructed. The adjusted Odds Ratio (OR) is expressed as OR with its corresponding 95% confidence interval (95% CI). Missing data were not defaulted to negative, and denominators reflect only reported cases. All P values calculated were 2 sided, and the statistical significance was set at P <0.05.
3. Results
3.1 Patient Demographics
A total of 61 participants with AAD met all inclusion criteria (Figure 1). These participants were sex-matched, age-matched (+/- 2 years), and technology-matched (CT scanner used) with 61 participants in the control group. Each group comprised 39 males and 22 females. Overall average age was 65.4 years for all respondents. For those with AAD, average age was higher in STB respondents (66.6 years) as opposed to STA (63.9 years) although this difference was not significant (p=0.422) (Table 1).
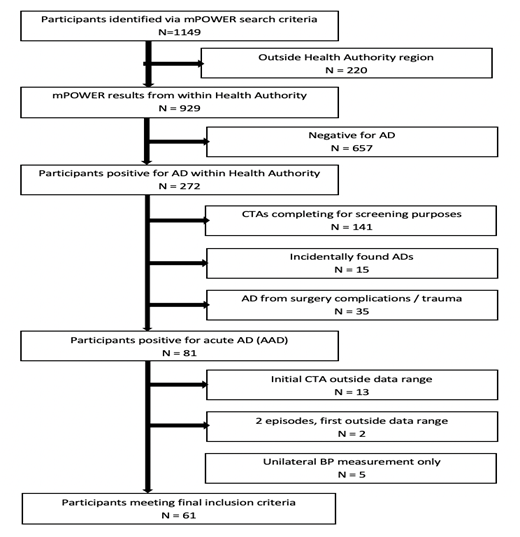
Figure 1: Participant inclusion.
Table 1: Demographics, mortality, clinical features and symptom frequency tabulations.
3.2 Symptoms at presentation
3.2.1 Chest pain
The most common symptom was chest pain present in 57.4% of respondents, although there was no difference in frequency between AAD groups and controls (p=0.387), AAD types (p=0.811), or sex (p=0.458).
3.2.2 Abdominal pain
Abdominal pain was significantly more frequent in STB respondents as opposed to STA (p=0.001) and compared to controls overall (p=0.003), as well as between STB vs. STA males (p=0.024) and STB vs. STA females (p=0.011). Females with abdominal pain had increased likelihood of mortality at 0, 1, 3, and 6 months (OR=12.05, p=0.027) as compared to male counterparts.
3.2.3 Syncope
Syncope was more common in STA than STB (p=0.040) overall and compared to controls (p=0.032). Males had a higher frequency of syncope than female counterparts overall (p=0.036) and in the AAD group (p=0.028). Males presenting with syncope also had an increased likelihood of mortality at 0, 1, 3, and 6 months (p=0.008).
3.2.4 Back pain
There was no significant difference in frequency of back pain for AAD overall compared to controls (p=0.143). However, females with STB dissection had a significantly higher frequency of back pain when compared to males with STB (p=0.034) (Table 2 and 3). Females overall (OR=13.5, p=0.003) and females in the AAD group (OR=12.0, p=0.015) who had presented with back pain also had an increased likelihood of mortality at 0, 1, 3, and 6 months. (Table 4).
Table 2: Means tabulations.
Table 3: Mortality odds ratios – overall.
Table 4: Mortality odds ratios (Study group – only those with AAD).
3.3 Average systolic blood pressure
Average systolic blood pressure was significantly higher in the STB group (152.2mm) when compared to the STA group (131.5mm, p=0.018), but not significantly higher than controls (151.4mm, p=0.318).
While the highest frequency of STA respondents fell into the <100mm and 101-150mm category (p=0.795 and p=0.022, respectively), STB respondents were most likely to have SBP 151mm or above (p=0.006). Similarly, falling into a higher systolic blood pressure category (151 + mm) was consistently related to a higher likelihood of STB diagnosis for both males and females. Of these, females had a 9.17 times increased likelihood of a STB diagnosis (p=0.026), as opposed to males (OR=6.18, p=0.027) and AAD group overall (OR=6.43, p=0.001) (Table 4).
Female respondents consistently demonstrated a higher average SBP across all groups than male counterparts overall (p=0.045) and in the AAD group alone (p=0.017) and more frequently fell into the two highest SBP categories (p=0.037, p=0.010).
3.4 Average blood pressure differential
Blood pressure differential was highest in STA respondents 24.30mm although this difference was not significant (p=0.458). There was no significant difference in blood pressure differential ranges, mortality rate or AAD types. Males and females had similar blood pressure differential frequencies.
3.5 Average pulse pressure
Average PP was 65.7mm in the AAD group overall and 68.5mm in controls (p=0.548). Respondents with PP <40mm had lower mortality rates at 0, 1, and 3 months (p=0.025-0.039), although there was no significant difference in mortality rates at 6 months (p=1.07).
Of the AAD respondents, presenting PP in the 41-80mm range represented a decreased likelihood of a STB diagnosis (OR=0.252, p=0.015), while falling into the 81 + mm range represented an increased likelihood of STB (OR=9.722, p=0.002). This relationship was found to be consistent in males and females.
STB respondents overall had significantly higher PP (72.1mm) than STA (58.1mm, p=0.032), and were more likely to fall into the 81 + mm category vs. controls (p=0.040). STB respondents falling into the lowest PP category (<40mm) had decreased mortality rates at 0, 1, 3, and 6 months (p=0.018), a trend which was consistent in STB males as well (p=0.025). Females with STB had a higher frequency of respondents falling into the 41-80mm and 81+ mm categories when compared to matched controls (p=0.009, p=0.024). Of the AAD respondents, presenting PP in the 41-80mm range represented a decreased likelihood of a STB diagnosis (OR=0.252, p=0.015), while falling into the 81+mm range represented an increased likelihood of STB (OR=9.722, p=0.002). This relationship was found to be consistent in males and females.
3.6 Differences in mortality
Males had consistently higher mortality rates across all time periods for overall respondents and AAD respondents alone, although this relationship was not significant (p=0.735, p=0.474) (Table 3-6).
|
Mortality Type A Only |
0m |
1m |
3m |
6m |
||||
|
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
|
Average PP |
||||||||
|
Overall |
||||||||
|
<40 |
0.37 (0.07-1.93) |
0.226 |
0.37 (0.07-1.93) |
0.226 |
0.37 (0.07-1.93) |
0.226 |
0.71 (0.15-3.26) |
0.655 |
|
41-80 |
1.55 (0.31-7.81) |
0.594 |
1.55 (0.31-7.81) |
0.594 |
1.20 (0.25-5.71) |
0.819 |
1.38 (0.33-5.68) |
0.654 |
|
81+ |
1.18 (1.04-1.32) |
0.31 |
1.18 (1.04-1.32) |
0.31 |
1.20 (1.06-1.27) |
0.273 |
1.18 (0.12-11.36) |
0.884 |
|
Males |
||||||||
|
<40 |
0.29 (0.02-5.10) |
0.358 |
0.29 (0.02-5.10) |
0.358 |
0.59 (0.05-7.41) |
0.682 |
1.28 (0.12-13.16) |
0.835 |
|
41-80 |
2.27 (0.13-40.00) |
0.565 |
2.27 (0.13-40.00) |
0.565 |
1.09 (0.09-13.33) |
0.946 |
1.53 (0.22-10.64) |
0.664 |
|
81+ |
1.06 (0.98-1.15) |
0.671 |
1.06 (0.98-1.15) |
0.671 |
1.09 (0.99-1.21) |
0.597 |
0.26 (0.02-3.53) |
0.281 |
|
Females |
||||||||
|
<40 |
0.37 (0.04-4.00) |
0.409 |
0.37 (0.04-4.00) |
0.409 |
0.37 (0.04-4.00) |
0.409 |
0.37 (0.04-4.00) |
0.409 |
|
41-80 |
1.00 (0.11-8.93) |
1 |
1.00 (0.11-8.93) |
1 |
1.00 (0.11-8.93) |
1 |
1.00 (0.11-8.93) |
1 |
|
81+ |
1.72 (1.06-2.76) |
0.171 |
1.72 (1.06-2.76) |
0.171 |
1.72 (1.06-2.76) |
0.171 |
1.72 (1.06-2.76) |
0.171 |
|
Average BP Differential |
||||||||
|
Overall |
||||||||
|
<10 |
2.91 (0.32-26.32) |
0.323 |
2.91 (0.32-26.32) |
0.323 |
3.50 (0.40-31.25) |
0.235 |
1.93 (0.37-10.31) |
0.432 |
|
44136 |
0.26 (0.05-1.39) |
0.098 |
0.26 (0.05-1.39) |
0.098 |
0.33 (0.07-1.68) |
0.17 |
0.27 (0.06-1.21) |
0.074 |
|
21+ |
1.74 (0.19-16.13) |
0.622 |
1.74 (0.19-16.13) |
0.622 |
0.79 (0.14-4.52) |
0.79 |
1.11 (0.20-6.10) |
0.903 |
|
Males |
||||||||
|
<10 |
0.46 (0.03-8.00) |
0.588 |
0.46 (0.03-8.00) |
0.588 |
0.96 (0.08-11.63) |
0.974 |
0.69 (0.10-4.72) |
0.702 |
|
44136 |
0.15 (0.01-2.83) |
0.155 |
0.15 (0.01-2.83) |
0.155 |
0.31 (0.02-4.12) |
0.355 |
0.19 (0.02-1.53) |
0.094 |
|
21+ |
1.07 (0.97-1.17) |
0.434 |
1.07 (0.97-1.17) |
0.434 |
0.55 (0.04-6.90) |
0.64 |
1.18 (0.12-12.20) |
0.886 |
|
Females |
||||||||
|
<10 |
1.72 (1.06-2.76) |
0.119 |
1.72 (1.06-2.76) |
0.119 |
1.72 (1.06-2.76) |
0.119 |
1.72 (1.06-2.76) |
0.119 |
|
44136 |
0.56 (0.06-5.21) |
0.611 |
0.56 (0.06-5.21) |
0.611 |
0.56 (0.06-5.21) |
0.611 |
0.56 (0.06-5.21) |
0.611 |
|
21+ |
0.89 (0.06-12.82) |
0.931 |
0.89 (0.06-12.82) |
0.931 |
0.89 (0.06-12.82) |
0.931 |
0.89 (0.06-12.82) |
0.931 |
|
Average Systolic BP |
||||||||
|
Overall |
||||||||
|
<100 |
0.55 (0.05-5.71) |
0.609 |
0.55 (0.05-5.71) |
0.609 |
0.65 (0.06-6.71) |
0.717 |
0.88 (0.09-8.89) |
0.912 |
|
101-150 |
0.56 (0.10-3.18) |
0.509 |
0.56 (0.10-3.18) |
0.509 |
0.45 (0.08-2.47) |
0.349 |
0.59 (0.13-2.56) |
0.475 |
|
151+ |
3.00 (0.33-27.03) |
0.308 |
3.00 (0.33-27.03) |
0.308 |
3.61 (0.41-32.30) |
0.223 |
2.00 (0.38-10.64) |
0.409 |
|
Males |
||||||||
|
<100 |
1.06 (0.98-1.15) |
0.624 |
1.06 (0.98-1.15) |
0.624 |
1.09 (0.99-1.21) |
0.542 |
1.17 (1.02 -1.34) |
0.418 |
|
101-150 |
0.92 (0.82-1.03) |
0.277 |
0.92 (0.82-1.03) |
0.277 |
0.88 (0.76-1.02) |
0.177 |
0.40 (0.04-4.02) |
0.427 |
|
151+ |
1.07 (0.97-1.19) |
0.394 |
1.07 (0.97-1.19) |
0.394 |
1.11 (0.99-1.26) |
0.29 |
1.44 (0.14-14.71) |
0.757 |
|
Females |
||||||||
|
<100 |
0.267 (0.12-0.62) |
0.126 |
0.267 (0.12-0.62) |
0.126 |
0.267 (0.12-0.62) |
0.126 |
0.267 (0.12-0.62) |
0.126 |
|
101-150 |
0.56 (0.06-4.76) |
0.59 |
0.56 (0.06-4.76) |
0.59 |
0.56 (0.06-4.76) |
0.59 |
0.56 (0.06-4.76) |
0.59 |
|
151+ |
4.81 (0.40-58.82) |
0.197 |
4.81 (0.40-58.82) |
0.197 |
4.81 (0.40-58.82) |
0.197 |
4.81 (0.40-58.82) |
0.197 |
|
Chest Pain |
||||||||
|
Overall |
3.62 (0.61-21.74) |
0.139 |
3.62 (0.61-21.74) |
0.139 |
2.62 (0.48-14.29) |
0.252 |
4.00 (0.80-20.00) |
0.079 |
|
Males |
3.83 (0.21-71.43) |
0.338 |
3.83 (0.21-71.43) |
0.338 |
1.83 (0.14-23.81) |
0.639 |
4.41 (0.45-38.46) |
0.16 |
|
Females |
3.00 (0.24-37.04) |
0.386 |
3.00 (0.24-37.04) |
0.386 |
3.00 (0.24-37.04) |
0.386 |
3.00 (0.24-37.04) |
0.386 |
|
SOB |
||||||||
|
Overall |
1.33 (0.19-9.17) |
0.77 |
1.33 (0.19-9.17) |
0.77 |
0.95 (0.15-6.06) |
0.961 |
1.57 (0.29-8.40) |
0.593 |
|
Males |
0.94 (0.83-1.06) |
0.42 |
0.94 (0.83-1.06) |
0.42 |
0.87 (0.73-1.05) |
0.245 |
0.78 (0.06-9.90) |
0.846 |
|
Females |
6.99 (0.40-12.50) |
0.157 |
6.99 (0.40-12.50) |
0.157 |
6.99 (0.40-12.50) |
0.157 |
6.99 (0.40-12.50) |
0.157 |
|
Abdominal Pain |
||||||||
|
Overall |
5.00 (0.42-58.82) |
0.182 |
5.00 (0.42-58.82) |
0.182 |
5.00 (0.42-58.82) |
0.182 |
3.00 (0.28-31.25) |
0.35 |
|
Males |
0.89 (0.71-1.12) |
0.621 |
0.89 (0.71-1.12) |
0.621 |
0.89 (0.71-1.12) |
0.621 |
0.78 (0.55-1.10) |
0.461 |
|
Females |
3.00 (0.606-14.86) |
0.136 |
3.00 (0.61-14.86) |
0.136 |
3.00 (0.61-14.86) |
0.136 |
3.00 (0.61-14.86) |
0.136 |
|
Nausea |
||||||||
|
Overall |
0.76 (0.07-8.70) |
0.826 |
0.76 (0.07-8.70) |
0.826 |
0.76 (0.07-8.70) |
0.826 |
0.54 (0.05-5.71) |
0.601 |
|
Males |
0.93 (0.80-1.07) |
0.633 |
0.93 (0.80-1.07) |
0.633 |
0.93 (0.80-1.07) |
0.633 |
0.86 (0.69-1.06) |
0.486 |
|
Females |
0.37 (0.02-6.33) |
0.49 |
0.37 (0.02-6.33) |
0.49 |
0.37 (0.02-6.33) |
0.49 |
0.37 (0.02-6.33) |
0.49 |
|
Vomiting |
||||||||
|
Overall |
1.33 (0.20-9.09) |
0.768 |
1.33 (0.20-9.09) |
0.768 |
0.78 (0.13-4.55) |
0.78 |
1.06 (0.19-5.92) |
0.946 |
|
Males |
0.87 (0.67-1.14) |
0.274 |
0.87 (0.67-1.14) |
0.274 |
0.75 (0.50-1.12) |
0.11 |
0.37 (0.03-5.18) |
0.453 |
|
Females |
1.33 (0.06-31.25) |
0.858 |
1.33 (0.06-31.25) |
0.858 |
1.33 (0.06-31.25) |
0.858 |
1.33 (0.06-31.25) |
0.858 |
|
Weakness |
||||||||
|
Overall |
0.80 (0.59-1.09) |
0.621 |
0.80 (0.59-1.09) |
0.621 |
0.80 (0.59-1.09) |
0.621 |
0.80 (0.59-1.09) |
0.621 |
|
Males |
0.89 (0.71-1.12) |
0.715 |
0.89 (0.71-1.12) |
0.715 |
0.89 (0.71-1.12) |
0.715 |
0.89 (0.71-1.12) |
0.715 |
|
Females |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
|
Syncope |
||||||||
|
Overall |
0.90 (0.73-1.11) |
0.74 |
0.90 (0.73-1.11) |
0.74 |
0.90 (0.73-1.11) |
0.74 |
0.90 (0.73-1.11) |
0.74 |
|
Males |
1.06 (0.98-1.16) |
0.504 |
1.06 (0.98-1.16) |
0.504 |
1.10 (0.99-1.23) |
0.407 |
1.18 (1.0 -1.36) |
0.271 |
|
Females |
0.67 (0.30-1.49) |
0.505 |
0.67 (0.30-1.49) |
0.505 |
0.67 (0.30-1.49) |
0.505 |
0.67 (0.30-1.49) |
0.505 |
|
Back Pain |
||||||||
|
Overall |
14.08 (0.62-33.3) |
0.042 |
14.08 (0.62-33.3) |
0.042 |
9.01 (0.44-20.00) |
0.098 |
6.49 (0.34-12.50) |
0.167 |
|
Males |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
|
Females |
4.50 (1.33-15.28) |
0.107 |
4.50 (1.33-15.28) |
0.107 |
4.50 (1.33-15.28) |
0.107 |
4.50 (1.33-15.28) |
0.107 |
|
Sex |
||||||||
|
Males / Females |
8.62 (1.47-50.00) |
0.007 |
8.62 (1.47-50.00) |
0.007 |
5.62 (1.15-27.03) |
0.022 |
3.18 (0.77-12.99) |
0.098 |
Table 5: Mortality odds ratios – stanford type A only.
|
0m |
1m |
3m |
6m |
|||||
|
Mortality Type B only |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
Average PP |
||||||||
|
Overall |
||||||||
|
<40 |
0.11 (0.01-0.92) |
0.018 |
0.11 (0.01-0.92) |
0.018 |
0.11 (0.01-0.92) |
0.018 |
0.13 (0.02-1.07) |
0.018 |
|
41-80 |
2.29 (0.50-10.53) |
0.277 |
2.29 (0.50-10.53) |
0.277 |
2.29 (0.50-10.53) |
0.277 |
1.67 (0.40-6.90) |
0.477 |
|
81+ |
1.17 (0.23-4.85) |
0.952 |
1.17 (0.23-4.85) |
0.952 |
1.17 (0.23-4.85) |
0.952 |
1.29 (0.29-5.71) |
0.733 |
|
Males |
||||||||
|
<40 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
|
41-80 |
1.62 (0.31-8.47) |
0.566 |
1.62 (0.31-8.47) |
0.566 |
1.62 (0.31-8.47) |
0.566 |
1.62 (0.31-8.47) |
0.566 |
|
81+ |
1.81 (0.30-10.75) |
0.514 |
1.81 (0.30-10.75) |
0.514 |
1.81 (0.30-10.75) |
0.514 |
1.81 (0.30-10.75) |
0.514 |
|
Females |
|
|
|
|
|
|
|
|
|
<40 |
1.04 (0.96-1.12) |
0.842 |
1.04 (0.96-1.12) |
0.842 |
1.04 (0.96-1.12) |
0.842 |
1.08 (0.97-1.21) |
0.773 |
|
41-80 |
1.10 (0.91-1.33) |
0.219 |
1.10 (0.91-1.33) |
0.219 |
1.10 (0.91-1.33) |
0.219 |
1.50 (0.08-27.03) |
0.782 |
|
81+ |
0.90 (0.73-1.11) |
0.184 |
0.90 (0.73-1.11) |
0.184 |
0.90 (0.73-1.11) |
0.184 |
0.56 (0.03-10.10) |
0.693 |
|
Average BP Differential |
||||||||
|
Overall |
||||||||
|
<10 |
2.67 (0.30-23.26) |
0.36 |
2.67 (0.30-23.26) |
0.36 |
2.67 (0.30-23.26) |
0.36 |
3.13 (0.36-27.03) |
0.28 |
|
44136 |
1.05 (0.19-5.75) |
0.958 |
1.05 (0.19-5.75) |
0.958 |
1.05 (0.19-5.75) |
0.958 |
1.25 (0.23-6.71) |
0.794 |
|
21+ |
3.15 (0.36-27.78) |
0.278 |
3.15 (0.36-27.78) |
0.278 |
3.15 (0.36-27.78) |
0.278 |
3.69 (0.43-32.26) |
0.208 |
|
Males |
||||||||
|
<10 |
1.32 (1.07-1.62) |
0.103 |
1.32 (1.07-1.62) |
0.103 |
1.32 (1.07-1.62) |
0.103 |
1.32 (1.07-1.62) |
0.103 |
|
44136 |
1.19 (0.20-7.25) |
0.85 |
1.19 (0.20-7.25) |
0.85 |
1.19 (0.20-7.25) |
0.85 |
1.19 (0.20-7.25) |
0.85 |
|
21+ |
2.86 (0.30-27.03) |
0.344 |
2.86 (0.30-27.03) |
0.344 |
2.86 (0.30-27.03) |
0.344 |
2.86 (0.30-27.03) |
0.344 |
|
Females |
||||||||
|
<10 |
0.87 (0.67-1.14) |
0.107 |
0.87 (0.67-1.14) |
0.107 |
0.87 (0.67-1.14) |
0.107 |
0.37 (0.02-6.71) |
0.486 |
|
44136 |
1.04 (0.96-1.14) |
0.635 |
1.04 (0.96-1.14) |
0.635 |
1.04 (0.96-1.14) |
0.635 |
1.10 (0.97-1.24) |
0.494 |
|
21+ |
1.05 (0.95-1.16) |
0.52 |
1.05 (0.95-1.16) |
0.52 |
1.05 (0.95-1.16) |
0.52 |
1.11 (0.96-1.29) |
0.353 |
|
Average Systolic BP |
||||||||
|
Overall |
||||||||
|
<100 |
0.05 (0.00-0.68) |
0.003 |
0.05 (0.00-0.68) |
0.003 |
0.05 (0.00-0.68) |
0.003 |
0.06 (0.01-0.80) |
0.007 |
|
101-150 |
1.75 (0.32-9.43) |
0.512 |
1.75 (0.32-9.43) |
0.512 |
1.75 (0.32-9.43) |
0.512 |
1.11 (0.25-4.93) |
0.89 |
|
151+ |
1.59 (0.36-7.04) |
0.538 |
1.59 (0.36-7.04) |
0.538 |
1.59 (0.36-7.04) |
0.538 |
2.08 (0.50-8.62) |
0.305 |
|
Males |
||||||||
|
<100 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
0.08 (0.01-1.10) |
0.025 |
|
101-150 |
1.38 (0.23-8.26) |
0.728 |
1.38 (0.23-8.26) |
0.728 |
1.38 (0.23-8.26) |
0.728 |
1.38 (0.23-8.26) |
0.728 |
|
151+ |
2.11 (0.40-11.11) |
0.372 |
2.11 (0.40-11.11) |
0.372 |
2.11 (0.40-11.11) |
0.372 |
2.11 (0.40-11.11) |
0.372 |
|
Females |
||||||||
|
<100 |
1.04 (0.96-1.12) |
0.845 |
1.04 (0.96-1.12) |
0.845 |
1.04 (0.96-1.12) |
0.845 |
1.08 (0.97-1.20) |
0.778 |
|
101-150 |
1.06 (0.94-1.20) |
0.434 |
1.06 (0.94-1.20) |
0.434 |
1.06 (0.94-1.20) |
0.434 |
0.56 (0.03-10.10) |
0.693 |
|
151+ |
0.94 (0.84-1.06) |
0.434 |
0.94 (0.84-1.06) |
0.434 |
0.94 (0.84-1.06) |
0.434 |
1.78 (0.10-32.26) |
0.693 |
|
Chest Pain |
||||||||
|
Overall |
1.31 (0.21-8.00) |
0.771 |
1.31 (0.21-8.00) |
0.771 |
1.31 (0.21-8.00) |
0.771 |
2.12 (0.41-10.87) |
0.359 |
|
Males |
0.75 (0.07-8.06) |
0.812 |
0.75 (0.07-8.06) |
0.812 |
0.75 (0.07-8.06) |
0.812 |
0.75 (0.07-8.06) |
0.812 |
|
Females |
1.14 (0.88-1.49) |
0.149 |
1.14 (0.88-1.49) |
0.149 |
1.14 (0.88-1.49) |
0.149 |
1.33 (0.89-1.99) |
0.037 |
|
SOB |
||||||||
|
Overall |
2.08 (0.26-16.39) |
0.481 |
2.08 (0.26-16.39) |
0.481 |
2.08 (0.26-16.39) |
0.481 |
2.08 (0.26-16.39) |
0.481 |
|
Males |
8.47 (0.61-12.50) |
0.075 |
8.47 (0.61-12.50) |
0.075 |
8.47 (0.61-12.50) |
0.075 |
8.47 (0.61-12.50) |
0.075 |
|
Females |
0.91 (0.75-1.10) |
0.353 |
0.91 (0.75-1.10) |
0.353 |
0.91 (0.75-1.10) |
0.353 |
0.91 (0.75-1.10) |
0.353 |
|
Abdominal Pain |
||||||||
|
Overall |
2.21 (0.34-14.49) |
0.4 |
2.21 (0.34-14.49) |
0.4 |
2.21 (0.34-14.49) |
0.4 |
2.21 (0.34-14.49) |
0.4 |
|
Males |
1.42 (0.11-17.54) |
0.785 |
1.42 (0.11-17.54) |
0.785 |
1.42 (0.11-17.54) |
0.785 |
1.42 (0.11-17.54) |
0.785 |
|
Females |
1.25 (0.81-1.94) |
0.086 |
1.25 (0.81-1.94) |
0.086 |
1.25 (0.81-1.94) |
0.086 |
1.25 (0.81-1.94) |
0.086 |
|
Nausea |
||||||||
|
Overall |
0.64 (0.06-6.85) |
0.708 |
0.64 (0.06-6.85) |
0.708 |
0.64 (0.06-6.85) |
0.708 |
0.64 (0.06-6.85) |
0.708 |
|
Males |
0.50 (0.04-6.02) |
0.581 |
0.50 (0.04-6.02) |
0.581 |
0.50 (0.04-6.02) |
0.581 |
0.50 (0.04-6.02) |
0.581 |
|
Females |
0.92 (0.79-1.08) |
0.523 |
0.92 (0.79-1.08) |
0.523 |
0.92 (0.79-1.08) |
0.523 |
0.92 (0.79-1.08) |
0.523 |
|
Vomiting |
||||||||
|
Overall |
0.50 (0.06-4.24) |
0.52 |
0.50 (0.06-4.24) |
0.52 |
0.50 (0.06-4.24) |
0.52 |
0.50 (0.06-4.24) |
0.52 |
|
Males |
0.20 (0.02-2.39) |
0.182 |
0.20 (0.02-2.39) |
0.182 |
0.20 (0.02-2.39) |
0.182 |
0.20 (0.02-2.39) |
0.182 |
|
Females |
0.86 (0.73-1.05) |
0.335 |
0.86 (0.73-1.05) |
0.335 |
0.86 (0.73-1.05) |
0.335 |
0.86 (0.73-1.05) |
0.335 |
|
Weakness |
||||||||
|
Overall |
0.87 (0.73-1.05) |
0.517 |
0.87 (0.73-1.05) |
0.517 |
0.87 (0.73-1.05) |
0.517 |
0.81 (0.64-1.03) |
0.414 |
|
Males |
1.02 (0.17-6.29) |
0.981 |
1.02 (0.17-6.29) |
0.981 |
1.02 (0.17-6.29) |
0.981 |
1.02 (0.17-6.29) |
0.981 |
|
Females |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
0.33 (0.03-3.51) |
0.35 |
|
Syncope |
||||||||
|
Overall |
2.00 (0.10-41.67) |
0.649 |
2.00 (0.10-41.67) |
0.649 |
2.00 (0.10-41.67) |
0.649 |
2.00 (0.10-41.67) |
0.649 |
|
Males |
7.00 (1.14-42.97) |
0.064 |
7.00 (1.14-42.97) |
0.064 |
7.00 (1.14-42.97) |
0.064 |
7.00 (1.14-42.97) |
0.064 |
|
Females |
0.67 (0.30-1.48) |
0.212 |
0.67 (0.30-1.48) |
0.212 |
0.67 (0.30-1.48) |
0.212 |
0.67 (0.30-1.48) |
0.212 |
|
Back Pain |
||||||||
|
Overall |
2.57 (0.20-32.36) |
0.451 |
2.57 (0.20-32.36) |
0.451 |
2.57 (0.20-32.36) |
0.451 |
1.67 (0.15-18.52) |
0.674 |
|
Males |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
1.50 (0.11-20.41) |
0.759 |
|
Females |
0.95 (0.85-1.05) |
0.483 |
0.95 (0.85-1.05) |
0.483 |
0.95 (0.85-1.05) |
0.483 |
0.89 (0.77-1.04) |
0.312 |
|
Sex |
||||||||
|
Males / Females |
0.16 (0.02-1.42) |
0.068 |
0.16 (0.02-1.42) |
0.068 |
0.16 (0.02-1.42) |
0.068 |
0.34 (0.07-1.78) |
0.187 |
Table 6: Mortality odds ratios – Stanford type B only.
|
Incidental Findings |
Immediate follow up recommended |
Non-immediate follow-up recommended |
Less urgent or no follow-up recommended |
|
Pulmonary |
|||
|
Embolus |
1 |
||
|
Nodules |
1 |
6 |
7 |
|
Pleural Effusion |
3 |
2 |
|
|
Vascular |
|||
|
Celiac artery stenosis |
1 |
||
|
Coronary artery calcification |
3 |
||
|
Subclavian artery occlusion |
1 |
||
|
Thrombosis |
1 |
||
|
Renal |
|||
|
Cyst |
2 |
1 |
|
|
Ischemia |
1 |
||
|
Nephrolithiasis |
1 |
||
|
Renal cell carcinoma |
1 |
||
|
Gastrointestinal |
|||
|
Ischemia |
2 |
||
|
Cardiac |
|||
|
Mitral valve calcification |
1 |
||
|
Musculoskeletal |
|||
|
Degenerative changes |
1 |
||
|
Rib fractures |
1 |
||
|
Vertebral fractures |
1 |
||
|
Breast |
|||
|
Lesion |
1 |
||
|
Gallbladder |
|||
|
Cholecystitis |
4 |
||
|
Cholelithiasis |
1 |
1 |
5 |
|
Liver |
|||
|
Cyst |
3 |
2 |
|
|
Mediastinum |
|||
|
Enlarged lymph nodes |
1 |
||
|
Prostate |
|||
|
Enlargement |
3 |
1 |
|
|
Hernia |
|||
|
Hiatal |
1 |
||
|
Periumbilical |
1 |
||
|
Appendix |
|||
|
Appendicitis |
1 |
||
Table 7: Incidental findings
Of STA respondents, males had significantly increased likelihood of mortality across 0, 1, 3 months (OR=5.62-8.62, p=0.007-0.022) than females. Of STB respondents, males consistently had a decreased likelihood of mortality at 0, 1, and 3 months (OR=0.16, p=0.068).
3.7 Incidental findings
A total of 46 respondents had incidental findings with a total of 63 findings (Table 7).
4. Discussion
4.1 Symptoms at Presentation
Most participants presented with chest pain in the ED from all groups, consistent with trends from previous research [9,10]. Although chest pain has been used in EDs globally as an indicator of AAD, our results demonstrate no difference in frequency of chest pain symptoms between the AAD group overall and age- and sex-matched controls, as well as specific AAD types and respective control participants. Our findings demonstrate an increased frequency of syncope, and later mortality, reported in those with STA dissection, consistent with previous reports [10,11]. STB respondents more commonly presented with back and abdominal pain, aligning with other studies [11,12].
While the frequency of syncope was significantly higher for those with STA dissection, the frequency of abdominal pain at presentation was significantly higher for those with STB dissection as opposed to STA, and matched controls. Overall, males presenting with syncope had an increased likelihood of mortality, while females presenting with abdominal pain had an increased likelihood of mortality, at all measured time points.
The current findings demonstrate the unique nature of AAD. Given the potential to mimic other syndromes, chest pain may not be the most reliable symptom to triage patients in the ED. Other symptoms, such as syncope and abdominal pain, in conjunction with the presenting sex of the patient, may have the potential to better analyze the likelihood of AAD and adverse outcomes.
4.2 Average Systolic Blood Pressure (SBP)
STB respondents overall presented with the highest average SBP, more frequently falling above 150mm Hg than those with STA dissection and matched controls (p=0.018, p=0.026).
Female respondents consistently demonstrated higher average SBP than male counterparts. Females presenting with average SBP above 150 mm Hg had a 9.17 times increased likelihood of a STB dissection above all AADs (p=0.026), while males had a 6.18 times increased risk (p=0.027). These findings are consistent with Erbel [13], suggesting hypotension may be a more valuable predictor for STA dissection, while hypertension for STB.
Mortality rates were also increased for those in the highest average SBP ranges, for both males and females, demonstrating a trend of increasing mortality with increasing SBP.
The current findings reflect well-established trends in previous research [14,15]. Mortality and adverse outcomes increase with increasing SBP, as does the likelihood of STB dissection. High SBP at baseline may be a valuable initial indicator of AAD and adverse outcomes, allowing for improved triage and risk stratification [15].
4.3 Average Blood Pressure Differential
The current findings reflect no significant relationship between blood pressure differential for AAD overall, and for specific type of AAD, over matched controls. There was also no significant difference related to gender or mortality rates across all measured time points.
Current literature, however, has suggested that these differentials above 10 mm Hg, or 20 mm Hg, to be clinically relevant predictors of AAD [11,16,17], several limitations exist. While Kuan et al. [16] was the first to assess blood pressure differentials with AAD as confirmed on Computed Tomography Angiography (CTA), the focus was a case report of a 35-year old female. Diercks et al. [11] found differentials above 20 mm Hg to be significant, however these were analyzed in participants presenting with acute tearing or ripping pain on presentation and the presence of a widened mediastinum on chest x-ray. These findings are like that of Von Kodolitsch et al. [2] and Klompas [1] which used chest x-ray to confirm findings, however Klompas [1] also combined pulse differentials with blood pressure differentials, which makes it difficult to determine which variable is driving the findings and whether they may be better used independently [5]. Singer and Hollander [17] and Orme et al. [4] established “normal” differential ranges, outside which AAD may be more likely. Despite 53% of participants having differentials >10 mm Hg and 19% with >20 mm Hg in the sample, none were diagnosed with AAD [17], questioning the specificity and reliability of this measurement in acute settings [5,6].
Um et al. [5] found a difference above 20 mm Hg to be associated with AAD. While this study was the first to use age- and sex-matched controls, technology was not controlled for and the diagnosis of AAD was confirmed with various imaging modalities. It is currently accepted that CTA is currently the best diagnostic tool for AAD, with a sensitivity of near 100% and a specificity of 98%.8 Other imaging modalities, such as those used here (chest x-ray, computed tomography, and transthoracic echocardiography) may not be as sensitive, specific, or reliable to accurately diagnose AAD.
It is unclear if the above findings are more common in patients with AAD confirmed on CTA compared to those who test negative on CTA [8]. To date, this is the first study analyzing blood pressure differentials in the context of CTA-confirmed AAD with matched controls. Our findings suggest no association between blood pressure differentials on presentation and type of dissection or mortality rates.
4.4 Average Pulse Pressure
The current results demonstrate lower mortality rates overall for those with narrower pulse pressures (p=0.025-0.039).
STA respondents had overall lower mean pulse pressures than STB respondents (p=0.032), consistent with previous studies [18] Of the STA respondents only, it has been previously shown that those under 40 mm Hg pulse pressure had increased mortality as compared to the higher reference ranges [18]. Our results contrast these findings, suggesting low-range pulse pressures had a decreased incidence of mortality at 0, 1, and 3 months (p=0.025) with no significant difference at 6-months post-AD (p=0.107). Mid-range pulse pressures (41-80mm) had an increasing likelihood of mortality, for type A and B AAD, although this trend is not significant (STA p=0.594, STB p=0.277).
The current research suggests that there is a significant difference in average pulse pressure between AAD types. The range of pulse pressure at presentation, in conjunction with type of dissection, may be a useful tool as a predictor of future adverse outcomes.
4.5 Gender Differences in Mortality
This is the first study to examine the value of average systolic blood pressure, blood pressure differentials, and pulse pressures together, between both males and females using matched controls. While Um et al. [5] used sex-matched controls, findings were not analyzed based on this grouping. Given the physiological variation between males and females, as well as the current findings demonstrating both symptomatic and AAD-type differences for sex, the influence of blood pressure differentials as stated in Um et al. [5] may not be generalizable.
Our current results demonstrate a unique, previously unidentified trend, and several gender-specific factors are identified. Of those with STA, males had higher mortality rates than females across all time points, while for STB respondents, females demonstrated increased mortality rates.
Males presenting with syncope had significantly increased rates of mortality across all groups as compared to females presenting with syncope (p=0.008). However, females presenting with back pain and/or abdominal pain had significantly increased mortality across all time points.
Our results suggest potential differences in symptomatic presentation could be invaluable in initial assessment and triage. While previous research suggests chest pain may be the most predictive presentation, our findings suggest no difference between AAD groups and controls, or males and females. However, the above findings point to the likelihood of a unique gender-specific presentation of AAD. It is pertinent to consider the possibility of other predictive symptoms, such as syncope and abdominal pain, in the initial ED assessment and the variation of AAD presentations between males and females.
This study has several limitations. As a retrospective study with chart review, the number of respondents was limited by the availability of health records. There was only database access to health records from 2012 onwards. Similarly, our catchment area encompasses a relatively small population size as compared to larger urban centers across Canada, further limiting our sample size.
This study assessed acute presentations of AAD and symptoms in the emergency department. Predisposing factors, such as Marfan’s syndrome, history of hypertension, or previous cardiac history were not controlled for, as much of this information was not available on present ED records.
5. Conclusion
Acute Aortic Dissection (AAD) is a serious, potentially fatal, diagnosis which is the result of a tear in the intimal lining of the aorta. AAD is a difficult diagnosis to make clinically as the typical symptoms occur more frequently in other, more common disorders such as myocardial infarction. This was the first study to compare average systolic blood pressure, blood pressure differentials, and pulse pressures together in conjunction with age-, sex-, and technology-matched controls as predictors of AAD and adverse outcomes. This was also the first to break these findings down further by AAD type and gender. Our findings demonstrate previously unidentified symptom and gender-specific factors. A better understanding of the physical examination findings in patients diagnosed with aortic dissection may help lead to better clinical decision making, improved patient outcomes, and decreased healthcare costs.
References
- Klompas M. Does this patient have an acute thoracic aortic dissection? JAMA 287 (2002).
- von Kodolitsch Y, Schwartz AG, Nienaber CA. Clinical prediction of acute aortic dissection. Arch Intern Med 160 (2000).
- Nazerian P, Giachino F, Vanni S, et al. Diagnostic performance of the aortic dissection detection risk score in patients with suspected acute aortic dissection. Eur Heart J Acute Cardiovasc Care. 3 (2014).
- Orme S, Ralph SG, Birchall A, et al. The normal range for inter-arm differences in blood pressure. Age Ageing 28 (1999).
- Um SW, Ohle R, Perry JJ. Bilateral blood pressure differential as a clinical marker for acute aortic dissection in the emergency department. Emergency Medicine Journal 35 (2018).
- Su YJ, Lai YC, Chen CC, et al. Inter-arm and inter-leg systolic blood pressure differences in aortic dissection. Int J Gerontol 1 (2007).
- Prabhakar AM, Le TQ, Abujudeh HH, et al. Incidental findings and recommendations are common on ED CT angiography to evaluate for aortic dissection. American Journal of Emergency Medicine 33 (2015).
- Baliga RR, Nienaber CA, Bossone E, et al. The role of imaging in aortic dissection and related syndromes. JACC Cardiovasc Imaging 7 (2014).
- Strayer RJ, Shearer PL, Hermann LK. Screening, evaluation, and early management of acute aortic dissection in the ED. Curr Cardiol Rev 8 (2012).
- Tsai TT, Trimarchi S, Nienaber CA. Acute Aortic Dissection: Perspectives from the International Registry of Acute Aortic Dissection (IRAD). European Journal of Vascular and Endovascular Surgery 37 (2009).
- Diercks DB, Promes SB, Schuur JD, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients with Suspected Acute Nontraumatic Thoracic Aortic Dissection. Ann Emerg Med 65 (2015).
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. J Am Med Assoc 283 (2000).
- Erbel R. Hypotensive Systolic Blood Pressure Predicts Severe Complications and In-Hospital Mortality in Acute Aortic Dissection. J Am Coll Cardiol 71 (2018).
- Lu N, Xu T, He Z, et al. Diastolic, but not systolic, blood pressure at admission is associated with aortic-related adverse events in type B dissection after thoracic endovascular aortic repair. Int J Cardiol 299 (2020).
- Bossone E, Gorla R, LaBounty TM, et al. Presenting Systolic Blood Pressure and Outcomes in Patients With Acute Aortic Dissection. J Am Coll Cardiol 71 (2018).
- Kuan PX, Tan PW, Jobli AT, et al. Discrepancy in blood pressure between the left and right arms - Importance of clinical diagnosis and role of radiological imaging. Medical Journal of Malaysia 71 (2016).
- Singer AJ, Hollander JE. Blood pressure. Assessment of interarm differences. Arch Intern Med 156 (1996).
- Hoff E, Eagle T, Pyeritz RE, et al. Pulse pressure and type A acute aortic dissection in-hospital outcomes (from the International Registry of Acute Aortic Dissection). American Journal of Cardiology 113 (2014).
