Bernese Periacetabular Osteotomy in Patients with Hip Dysplasia Secondary to Cerebral Palsy and Developmental Dysplasia of the Hips
Article Information
Si Heng Sharon Tan*, James Hoipo Hui and Andrew Kean Seng Lim
Department of Orthopaedic Surgery, University Orthopaedic, Hand and Reconstructive Microsurgery Cluster, National University Health System (NUHS), Singapore
*Corresponding Author: Tan Si Heng, Sharon, Department of Orthopaedic Surgery, National University Health System, 1E Kent Ridge Road, NUHS Tower Block Level 11, Singapore.
Received: 09 September 2023; Accepted: 20 September 2023; Published: 06 October 2023
Citation: Si Heng Sharon Tan, James Hoipo Hui, Andrew Kean Seng Lim. Bernese Periacetabular Osteotomy in Patients with Hip Dysplasia Secondary to Cerebral Palsy and Developmental Dysplasia of the Hips. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 203-209.
Share at FacebookAbstract
Purpose: The current study aims to evaluate the outcomes of the Bernese periacetabular osteotomy when performed for children and adolescents with hip dysplasia secondary to cerebral palsy. The secondary aim of the study was to compare the outcomes of the Bernese periacetabular osteotomy when performed for hip dysplasia secondary to cerebral palsy as opposed to developmental dysplasia of the hips.
Methods: In the prospective case-control study, all patients under the age of 21 years who underwent the Bernese periacetabular osteotomy for hip dysplasia secondary to cerebral palsy or developmental dysplasia of the hips were included.
Results: Statistically significant improvements were noted for the acetabular index (p = 0.040), lateral central edge angle (p = 0.001), migration index (p < 0.001), extrusion index (p = 0.001) and Shenton line (p = 0.002) post-operatively as compared to pre-operatively. These improvements were similarly noted when subgroup analyses were performed for the patients with hip dysplasia secondary to cerebral palsy versus secondary to developmental dysplasia of the hips. Amongst the patients with hip dysplasia secondary to cerebral palsy, there was also improvement, if not maintenance, of the GMFCS levels in all patients postoperatively. All patients who were GMFCS level V also identified that there was less difficulty with perineal care post-operatively. All patients also reported pain relief post-operatively. When comparing between patients with hip dysplasia secondary to cerebral palsy versus patients with hip dysplasia secondary to developmental dysplasia of the hips, there were no statistically significant differences in the post-operative outcomes or change in pre-operative versus post-operative outcomes.
Conclusions: The Bernese periacetabular osteotomy is a viable surgical option for children and adolescents with closed triradiate cartilage and hip dysplasia. This applies to both patients with hip dysplasia secondary to cerebral palsy and hip dysplasia secondary to developmental dysplasia of the hips.
Keywords
Bernese periacetabular osteotomy; Ganz periacetabular osteotomy; Cerebral palsy; Neurogenic hip dysplasia; Developmental dysplasia of the hip; Hip dysplasia
Orthopaedic surgery articles Orthopaedic surgery Research articles Orthopaedic surgery review articles Orthopaedic surgery PubMed articles Orthopaedic surgery PubMed Central articles Orthopaedic surgery 2023 articles Orthopaedic surgery 2024 articles Orthopaedic surgery Scopus articles Orthopaedic surgery impact factor journals Orthopaedic surgery Scopus journals Orthopaedic surgery PubMed journals Orthopaedic surgery medical journals Orthopaedic surgery free journals Orthopaedic surgery best journals Orthopaedic surgery top journals Orthopaedic surgery free medical journals Orthopaedic surgery famous journals Orthopaedic surgery Google Scholar indexed journals Hip dysplasia articles Hip dysplasia Research articles Hip dysplasia review articles Hip dysplasia PubMed articles Hip dysplasia PubMed Central articles Hip dysplasia 2023 articles Hip dysplasia 2024 articles Hip dysplasia Scopus articles Hip dysplasia impact factor journals Hip dysplasia Scopus journals Hip dysplasia PubMed journals Hip dysplasia medical journals Hip dysplasia free journals Hip dysplasia best journals Hip dysplasia top journals Hip dysplasia free medical journals Hip dysplasia famous journals Hip dysplasia Google Scholar indexed journals Cerebral palsy articles Cerebral palsy Research articles Cerebral palsy review articles Cerebral palsy PubMed articles Cerebral palsy PubMed Central articles Cerebral palsy 2023 articles Cerebral palsy 2024 articles Cerebral palsy Scopus articles Cerebral palsy impact factor journals Cerebral palsy Scopus journals Cerebral palsy PubMed journals Cerebral palsy medical journals Cerebral palsy free journals Cerebral palsy best journals Cerebral palsy top journals Cerebral palsy free medical journals Cerebral palsy famous journals Cerebral palsy Google Scholar indexed journals Osteotomy articles Osteotomy Research articles Osteotomy review articles Osteotomy PubMed articles Osteotomy PubMed Central articles Osteotomy 2023 articles Osteotomy 2024 articles Osteotomy Scopus articles Osteotomy impact factor journals Osteotomy Scopus journals Osteotomy PubMed journals Osteotomy medical journals Osteotomy free journals Osteotomy best journals Osteotomy top journals Osteotomy free medical journals Osteotomy famous journals Osteotomy Google Scholar indexed journals Paediatric physical disability articles Paediatric physical disability Research articles Paediatric physical disability review articles Paediatric physical disability PubMed articles Paediatric physical disability PubMed Central articles Paediatric physical disability 2023 articles Paediatric physical disability 2024 articles Paediatric physical disability Scopus articles Paediatric physical disability impact factor journals Paediatric physical disability Scopus journals Paediatric physical disability PubMed journals Paediatric physical disability medical journals Paediatric physical disability free journals Paediatric physical disability best journals Paediatric physical disability top journals Paediatric physical disability free medical journals Paediatric physical disability famous journals Paediatric physical disability Google Scholar indexed journals Children articles Children Research articles Children review articles Children PubMed articles Children PubMed Central articles Children 2023 articles Children 2024 articles Children Scopus articles Children impact factor journals Children Scopus journals Children PubMed journals Children medical journals Children free journals Children best journals Children top journals Children free medical journals Children famous journals Children Google Scholar indexed journals Perineal care articles Perineal care Research articles Perineal care review articles Perineal care PubMed articles Perineal care PubMed Central articles Perineal care 2023 articles Perineal care 2024 articles Perineal care Scopus articles Perineal care impact factor journals Perineal care Scopus journals Perineal care PubMed journals Perineal care medical journals Perineal care free journals Perineal care best journals Perineal care top journals Perineal care free medical journals Perineal care famous journals Perineal care Google Scholar indexed journals Bernese periacetabular osteotomy articles Bernese periacetabular osteotomy Research articles Bernese periacetabular osteotomy review articles Bernese periacetabular osteotomy PubMed articles Bernese periacetabular osteotomy PubMed Central articles Bernese periacetabular osteotomy 2023 articles Bernese periacetabular osteotomy 2024 articles Bernese periacetabular osteotomy Scopus articles Bernese periacetabular osteotomy impact factor journals Bernese periacetabular osteotomy Scopus journals Bernese periacetabular osteotomy PubMed journals Bernese periacetabular osteotomy medical journals Bernese periacetabular osteotomy free journals Bernese periacetabular osteotomy best journals Bernese periacetabular osteotomy top journals Bernese periacetabular osteotomy free medical journals Bernese periacetabular osteotomy famous journals Bernese periacetabular osteotomy Google Scholar indexed journals Ambulatory difficulties articles Ambulatory difficulties Research articles Ambulatory difficulties review articles Ambulatory difficulties PubMed articles Ambulatory difficulties PubMed Central articles Ambulatory difficulties 2023 articles Ambulatory difficulties 2024 articles Ambulatory difficulties Scopus articles Ambulatory difficulties impact factor journals Ambulatory difficulties Scopus journals Ambulatory difficulties PubMed journals Ambulatory difficulties medical journals Ambulatory difficulties free journals Ambulatory difficulties best journals Ambulatory difficulties top journals Ambulatory difficulties free medical journals Ambulatory difficulties famous journals Ambulatory difficulties Google Scholar indexed journals Bilateral hips articles Bilateral hips Research articles Bilateral hips review articles Bilateral hips PubMed articles Bilateral hips PubMed Central articles Bilateral hips 2023 articles Bilateral hips 2024 articles Bilateral hips Scopus articles Bilateral hips impact factor journals Bilateral hips Scopus journals Bilateral hips PubMed journals Bilateral hips medical journals Bilateral hips free journals Bilateral hips best journals Bilateral hips top journals Bilateral hips free medical journals Bilateral hips famous journals Bilateral hips Google Scholar indexed journals Femoral head articles Femoral head Research articles Femoral head review articles Femoral head PubMed articles Femoral head PubMed Central articles Femoral head 2023 articles Femoral head 2024 articles Femoral head Scopus articles Femoral head impact factor journals Femoral head Scopus journals Femoral head PubMed journals Femoral head medical journals Femoral head free journals Femoral head best journals Femoral head top journals Femoral head free medical journals Femoral head famous journals Femoral head Google Scholar indexed journals Orthopaedic surgeons articles Orthopaedic surgeons Research articles Orthopaedic surgeons review articles Orthopaedic surgeons PubMed articles Orthopaedic surgeons PubMed Central articles Orthopaedic surgeons 2023 articles Orthopaedic surgeons 2024 articles Orthopaedic surgeons Scopus articles Orthopaedic surgeons impact factor journals Orthopaedic surgeons Scopus journals Orthopaedic surgeons PubMed journals Orthopaedic surgeons medical journals Orthopaedic surgeons free journals Orthopaedic surgeons best journals Orthopaedic surgeons top journals Orthopaedic surgeons free medical journals Orthopaedic surgeons famous journals Orthopaedic surgeons Google Scholar indexed journals Lower limb articles Lower limb Research articles Lower limb review articles Lower limb PubMed articles Lower limb PubMed Central articles Lower limb 2023 articles Lower limb 2024 articles Lower limb Scopus articles Lower limb impact factor journals Lower limb Scopus journals Lower limb PubMed journals Lower limb medical journals Lower limb free journals Lower limb best journals Lower limb top journals Lower limb free medical journals Lower limb famous journals Lower limb Google Scholar indexed journals Pelvic osteotomies articles Pelvic osteotomies Research articles Pelvic osteotomies review articles Pelvic osteotomies PubMed articles Pelvic osteotomies PubMed Central articles Pelvic osteotomies 2023 articles Pelvic osteotomies 2024 articles Pelvic osteotomies Scopus articles Pelvic osteotomies impact factor journals Pelvic osteotomies Scopus journals Pelvic osteotomies PubMed journals Pelvic osteotomies medical journals Pelvic osteotomies free journals Pelvic osteotomies best journals Pelvic osteotomies top journals Pelvic osteotomies free medical journals Pelvic osteotomies famous journals Pelvic osteotomies Google Scholar indexed journals Triradiate cartilage articles Triradiate cartilage Research articles Triradiate cartilage review articles Triradiate cartilage PubMed articles Triradiate cartilage PubMed Central articles Triradiate cartilage 2023 articles Triradiate cartilage 2024 articles Triradiate cartilage Scopus articles Triradiate cartilage impact factor journals Triradiate cartilage Scopus journals Triradiate cartilage PubMed journals Triradiate cartilage medical journals Triradiate cartilage free journals Triradiate cartilage best journals Triradiate cartilage top journals Triradiate cartilage free medical journals Triradiate cartilage famous journals Triradiate cartilage Google Scholar indexed journals
Article Details
1. Introduction
Cerebral palsy is one of the most common causes of paediatric physical disability [1]. Amongst these, up to 90% of patients with cerebral palsy are affected with dysplastic hips, especially in children with Gross Motor Function Classification System (GMFCS) level V [2,3]. These can lead to pain, ambulatory difficulties, poor sitting balance and difficulty with perineal care [4,5].
The Bernese periacetabular osteotomy, otherwise commonly known as the Ganz periacetabular osteotomy, is one of the surgical strategies that has been repeatedly reported to be successful in the management of symptomatic hip dysplasia in adolescents and young adults [6-8]. However, literature regarding its outcomes in patients with hip dysplasia secondary to cerebral palsy has been limited [2,9].
The current study therefore aims to evaluate the outcomes of the Bernese periacetabular osteotomy when performed for children and adolescents with hip dysplasia secondary to cerebral palsy. The secondary aim of the study was to compare the outcomes of the Bernese periacetabular osteotomy when performed for hip dysplasia secondary to cerebral palsy as opposed to developmental dysplasia of the hips.
2. Material and Methods
In the prospective case-control study, all patients under the age of 21 years who underwent the Bernese periacetabular osteotomy for hip dysplasia secondary to cerebral palsy or developmental dysplasia of the hips over a 2-year period in a single institution were included. All patients who had hip dysplasia secondary to other conditions were excluded. The indication for the Bernese periacetabular osteotomy was symptomatic hip dysplasia in a patient with closed triradiate cartilage. Symptoms arising from the hip dysplasia include pain, ambulatory difficulties, sitting difficulties, pressure sores and difficulty with perineal care.
Pre-operatively, all patients were evaluated on an outpatient basis and identified to have symptomatic hip dysplasia secondary to cerebral palsy or developmental dysplasia of the hip. The patients were also assessed radiographically and confirmed to have closed triradiate cartilage. Radiographs including anteroposterior and false profile views of bilateral hips were also obtained to determine the coverage of the femoral head and for pre-operative planning. The radiographic parameters measured on the pre-operative radiographs include the acetabular index, lateral central edge angle, migration index, extrusion index and Shenton line [10-14]. The version of the acetabulum was also evaluated using the crossover sign and posterior wall sign [15,16]. Apart from the radiographic parameters, the GMFCS level was also obtained for patients with cerebral palsy pre-operatively, while the Harris hip score was obtained for patients with developmental dysplasia of the hip pre-operatively [3,17].
After the above pre-operative evaluation and after obtaining informed consent, all patients then underwent the Bernese periacetabular osteotomy by one of the senior orthopaedic surgeons. The patients were positioned supine on a radiolucent operative table. The entire lower limb is cleaned and draped to permit manipulation during the surgery. An anterior approach of the hip, otherwise known as the Smith-Petersen approach, is used. An iliac apophysis split is then performed with subperiosteal dissection to the sciatic notch, as well as over the superior pubic ramus and ischium. Pelvic osteotomies are then sequentially performed under intraoperative imaging guidance with anteroposterior and 45 degrees iliac oblique views (Figure 1). The first osteotomy performed is that of the anterior ischial cut, performed using the Ganz osteotome. Following which, the superior pubic ramus cut is performed using the Ganz osteotome. Subsequently, the iliac wing is then osteotomised with an oscillating saw. Lastly, the posterior column is cut with a Ganz osteotome to meet the first ischial cut. With the above osteotomies, the periacetabular fragment is then freed and repositioned to obtain improved acetabular coverage (Figure 2). The fragment is then held with temporary Kirschner wires (Figure 3). Definitive fixation is made subsequently when cortical screws (Figure 4). The final position of the periacetabular fragment is then confirmed with intraoperative imaging to be satisfactory prior to layered closure and dressings.
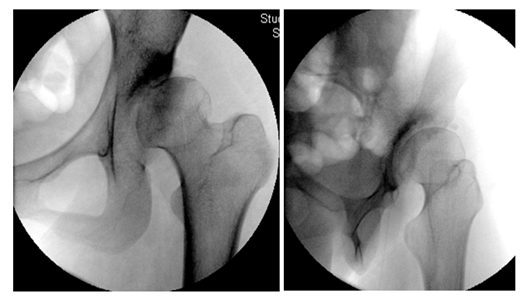
Figure 1: Demonstrates the anteroposterior and 45 degrees iliac oblique intraoperative imaging views used to guide the pelvic osteotomies.
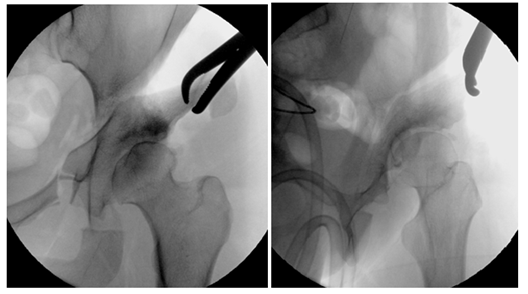
Figure 2: Demonstrates the anteroposterior and 45 degrees iliac oblique intraoperative imaging views after the pelvic osteotomies, allowing the periacetabular fragment to be freed and repositioned to obtain improved acetabular coverage.
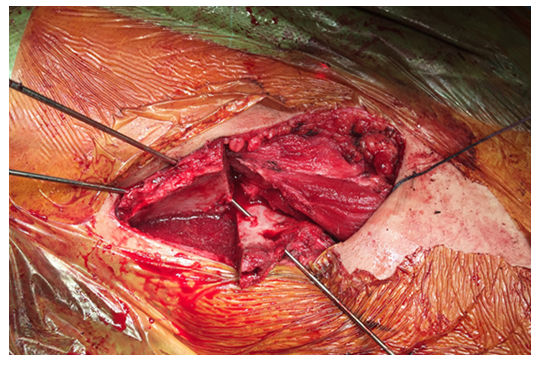
Figure 3: Demonstrates the freed and repositioned fragment held temporarily with Kirschner wires to obtain improved acetabular coverage.
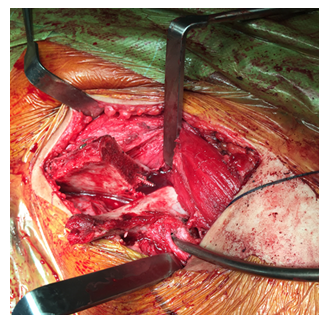
Figure 4: Demonstrates the freed and repositioned fragment fixed definitively with cortical screws to obtain improved acetabular coverage.
Post-operatively, the patient is allowed partial weight bearing from the first post-operative day as tolerated based on their pre-operative functional status for a total of six weeks. The patients are typically discharged within the first post-operative week and are scheduled for regular outpatient follow-up visits post-operatively. Repeat radiographs are performed at the six-week interval and weight-bearing was advanced gradually as tolerated.
All patients included in the study had a minimum of two-year follow-up duration prior to the conclusion of the study. At the last follow-up visit, the GMFCS level was assessed for patients with cerebral palsy and the Harris hip score was evaluated for patients with developmental dysplasia of the hips. The radiographs were also evaluated post-operatively for similar radiographic parameters, including the acetabular index, lateral central edge angle, migration index, extrusion index, crossover sign, posterior wall sign and the Shenton line. Measurements of the radiographic parameters were performed blind, without knowledge and cross-referencing to the pre-operative radiographs.
The study was performed in accordance with the ethical standards of the institutional research committee.
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) 23.0 was used for statistical analysis. Paired student’s T-test and McNemar’s exact test was performed to compare the pre-operative and post-operative outcomes for continuous and categorical variables respectively. Student’s T-test and Fisher’s exact test was performed to compare between the outcomes of patients with hip dysplasia secondary to cerebral palsy and with hip dysplasia secondary to developmental dysplasia of the hips. A p-value of <0.05 was considered statistically significant.
3. Results
A total of eleven patients were included in the study. These included six patients with hip dysplasia secondary to cerebral palsy and five patients with hip dysplasia secondary to developmental dysplasia of the hips. All patients had Bernese periacetabular osteotomy performed. The patients with cerebral palsy also had varus derotational femoral osteotomy performed. One of the patients with cerebral palsy had contralateral surgery performed, but only left hip had completed two years of follow-up at the conclusion of the study, and therefore only the outcomes of the left hip were included in the study.
The average age of the patients was 15.0 years (SD 3.8). There was no statistically significant difference in the age of the patients between the two groups, with the average age of the patients with hip dysplasia secondary to cerebral palsy being 14.2 years (SD 2.1) while the average age of the patients with hip dysplasia secondary to developmental dysplasia of the hips was 16.0 years (SD 5.2) (p = 0.496).
When comparing pre-operative and post-operative outcomes, there was statistically significant improvements in all the parameters evaluated (Table 1). These included decrease in the acetabular index (p = 0.040), increase in the lateral central edge angle (p = 0.001), decrease in the migration index (p < 0.001), decrease in the extrusion index (p = 0.001) and restoration of the Shenton line (p = 0.002) (Table 1). These statistical significances were maintained in most of the parameters when subgroup analyses were performed for the patients with hip dysplasia secondary to cerebral palsy versus secondary to developmental dysplasia of the hips (Table 1).
|
Overall |
Pre-Operative |
Post-Operative |
P-value |
||
|
Mean /Frequency |
SD /Percentage |
Mean /Frequency |
SD /Percentage |
||
|
Acetabular Angle (Degrees) |
53.3 |
6.4 |
46.5 |
12.4 |
0.04 |
|
Lateral Central Edge Angle (Degrees) |
-12.7 |
23.7 |
31.5 |
17.6 |
0.001 |
|
Migration Index (Percentage) |
85.9 |
22.9 |
16 |
20.6 |
<0.001 |
|
Extrusion Index (Percentage) |
67.8 |
26.6 |
20.6 |
28.3 |
0.001 |
|
Shenton Line (In Continuity/Not In Continuity) |
0 / 11 |
0.0 / 100.0 |
11 / 0 |
100.0 / 0.0 |
0.002 |
|
Hip Dysplasia Secondary to Cerebral Palsy |
|||||
|
Acetabular Angle (Degrees) |
55.2 |
7.8 |
47.9 |
15.4 |
0.098 |
|
Lateral Central Edge Angle (Degrees) |
-22.3 |
26.5 |
28.1 |
22.8 |
0.037 |
|
Migration Index (Percentage) |
98.3 |
3.1 |
18.6 |
23.8 |
0.001 |
|
Extrusion Index (Percentage) |
86.5 |
15.8 |
29.6 |
35.4 |
0.027 |
|
Shenton Line (In Continuity/Not In Continuity) |
0 / 6 |
0.0 / 100.0 |
6 / 0 |
100.0 / 0.0 |
0.031 |
|
GMFCS (Level) |
4 |
1.3 |
3.8 |
1.3 |
0.363 |
|
Hip Dysplasia Secondary to Developmental Dysplasia of the Hips |
|||||
|
Acetabular Angle (Degrees) |
51.1 |
3.6 |
44.9 |
8.9 |
0.291 |
|
Lateral Central Edge Angle (Degrees) |
-1.2 |
15.1 |
25.6 |
9.2 |
0.001 |
|
Migration Index (Percentage) |
71.1 |
28.1 |
12.9 |
18.3 |
0.004 |
|
Extrusion Index (Percentage) |
45.3 |
17.2 |
9.8 |
12.8 |
0.012 |
|
Shenton Line (In Continuity/Not In Continuity) |
0 / 5 |
0.0 / 100.0 |
5 / 0 |
100.0 / 0.0 |
0.031 |
|
Harris Hip Score |
77.3 |
13.6 |
92.4 |
3.1 |
0.131 |
Table 1: details the pre-operative versus post-operative outcomes for the overall group as well as the individual groups with patients with hip dysplasia secondary to cerebral palsy and patients with hip dysplasia secondary to developmental dysplasia of the hips.
In the group with patients with hip dysplasia secondary to cerebral palsy, there were similar statistically significant improvements in the lateral central edge angle (p = 0.037), migration index (p = 0.001), extrusion index (p = 0.027) and Shenton line (p = 0.031) post-operatively (Table 1). Improvements were noted for the acetabular index (p = 0.098) and GMFCS (p = 0.363) though not statistically significant (Table 1). Pre-operatively, there were three patients with GMFCS level V, one patient with GMFCS level IV, one patient with GMFCS level III and one patient with GMFCS level II. The patient with GMFCS level IV improved to level III post-operatively, while the other two patients with GMFCS level III and II managed to maintain their GMFCS levels. All three of the patients who were GMFCS level V also identified that there was less difficulty with perineal care post-operatively. All patients reported pain relief post-operatively.
When comparing between patients with hip dysplasia secondary to cerebral palsy versus patients with hip dysplasia secondary to developmental dysplasia of the hips, there were no statistically significant differences in the post-operative outcomes (Table 2). These include the post-operative acetabular index (p = 0.694), lateral central edge angle (p = 0.482), migration index (p = 0.663), extrusion index (p = 0.245) and Shenton line (p = 0.999) (Table 2).
|
Hip Dysplasia Secondary to Cerebral Palsy |
Hip Dysplasia Secondary to Developmental Dysplasia of the Hips |
P-value |
|||
|
Mean /Frequency |
SD /Percentage |
Mean /Frequency |
SD /Percentage |
||
|
Acetabular Angle (Degrees) |
47.9 |
15.4 |
44.9 |
8.9 |
0.694 |
|
Lateral Central Edge Angle (Degrees) |
28.1 |
22.8 |
25.6 |
9.2 |
0.482 |
|
Migration Index (Percentage) |
18.6 |
23.8 |
12.9 |
18.3 |
0.663 |
|
Extrusion Index (Percentage) |
29.6 |
35.4 |
9.8 |
12.8 |
0.245 |
|
Shenton Line (In Continuity/Not In Continuity) |
6 / 0 |
100.0 / 0.0 |
5 / 0 |
100.0 / 0.0 |
0.999 |
Table 2: details the comparison of the post-operative outcomes between patients with hip dysplasia secondary to cerebral palsy and patients with hip dysplasia secondary to developmental dysplasia of the hips.
Similarly, there were no statistically significant differences when comparing the change in pre-operative versus post-operative outcomes between patients with hip dysplasia secondary to cerebral palsy versus patients with hip dysplasia secondary to developmental dysplasia of the hips (Table 3). These include the change in acetabular index (p = 0.860), lateral central edge angle (p = 0.494), migration index (p = 0.158), extrusion index (p = 0.325) and Shenton line (p = 0.999) (Table 3).
|
Hip Dysplasia Secondary to Cerebral Palsy |
Hip Dysplasia Secondary to Developmental Dysplasia of the Hips |
P-value |
|||
|
Mean / Frequency |
SD / Percentage |
Mean / Frequency |
SD /Percentage |
||
|
Acetabular Angle (Degrees) |
7.3 |
8.8 |
6.2 |
11.4 |
0.86 |
|
Lateral Central Edge Angle (Degrees) |
50.4 |
43.7 |
36.9 |
10.1 |
0.494 |
|
Migration Index (Percentage) |
79.7 |
24.9 |
58.2 |
21.5 |
0.158 |
|
Extrusion Index (Percentage) |
56.9 |
45.2 |
35.5 |
18 |
0.325 |
|
Shenton Line (Change / No Change) |
6 / 0 |
100.0 / 0.0 |
5 / 0 |
100.0 / 0.0 |
0.999 |
Table 3: Details the comparison of the change in pre-operative versus post-operative outcomes between patients with hip dysplasia secondary to cerebral palsy and patients with hip dysplasia secondary to developmental dysplasia of the hips.
Three of the patients had complications post-operatively. All three patients had retroversion of the hip, which were also present pre-operatively, but inadequately corrected during the operation. One of the three patients required adjustment of screws for the retroversion, while the other two were managed non-surgically. Another one of the three patients also had superficial surgical site infection that resolved with antibiotics. Two of these three patients had hip dysplasia secondary to cerebral palsy while the other patient had hip dysplasia secondary to developmental dysplasia of the hips.
4. Discussion
The principal finding of the study is that the Bernese periacetabular osteotomy is a viable surgical option for children and adolescents with closed triradiate cartilage and hip dysplasia. This applies to both patients with hip dysplasia secondary to cerebral palsy and hip dysplasia secondary to developmental dysplasia of the hips. There are no significant differences in the outcomes post-operatively when the Bernese periacetabular osteotomy is used for hip dysplasia secondary to cerebral palsy or secondary to developmental dysplasia of the hips.
These good post-operative outcomes for patients with hip dysplasia secondary to cerebral palsy parallel the findings identified in two other publications [2,9]. MacDonald et al, in their study of patients with neurogenic acetabular dysplasia, included five patients with hip dysplasia secondary to cerebral palsy, and identified that the Bernese periacetabular osteotomy can be used successfully to manage neurogenic acetabular dysplasia with improvement in the acetabular index, centre-edge angle, extrusion index and pain9. However, they did not specifically perform subgroup analysis regarding the outcomes of the patients with cerebral palsy only [9]. Georgiadis et al focused on the outcomes of Bernese periacetabular osteotomy in patient with hip dysplasia secondary to cerebral palsy only [2]. Similarly, they found that the Bernese periacetabular osteotomy was successful in correcting the acetabular dysplasia for these patients [2]. Their study, however, was slightly different in that they focused mainly on the patients with GMFCS level I, II and III, in which hip dysplasia was rarer as compared to the GMFCS level IV and V patients [2].
The current study is therefore novel in several ways. Firstly, to the authors’ knowledge, the current study is the first study that studied the outcomes of the Bernese periacetabular osteotomy in patients with cerebral palsy regardless of the GMFCS level. The improvements in the post-operative outcomes of all of the patients with cerebral palsy proved that the Bernese periacetabular osteotomy has a role in the management of hip dysplasia in patients with cerebral palsy regardless of the GMFCS level. In fact, the Bernese periacetabular osteotomy was able to improve the gross motor function and GMFCS level of one of the patients with advanced GMFCS level, improving the GMFCS level from level IV to level III post-operatively. This reinforces the belief that breaking the vicious cycle of hip dysplasia and decreasing gross motor function level can indeed improve the functional capacity of the patients [3,5]. While two of the other patients with GMFCS level II and III had no improvements in their GMFCS levels post-operatively, there were able to maintain their GMFCS levels for at least two years post-operatively despite the known natural history of the deterioration of GMFCS with age [3]. Similarly, while the three patients with GMFCS level V expectedly did not have an improvement in their GMFCS levels post-operatively, all three patients identified less difficulty with perineal care post-operatively. All patients also experienced pain relief post-operatively. Indeed, as per the study by Cobanoglu et al, hip reconstructions for hip dysplasia secondary to cerebral palsy are able to result in improvement in outcomes post-operatively, though these might not be reflected in the improvement in GMFCS levels post-operatively [5].
Secondly, the current study is the only study available in the literature that has compared between the outcomes following the Bernese periacetabular osteotomy for patients with hip dysplasia secondary to cerebral palsy versus developmental dysplasia of the hips. Traditionally, the Bernese periacetabular osteotomy has most commonly been performed for developmental dysplasia of the hips [6-8]. Most of the studies reporting the success of the Bernese periacetabular osteotomy have therefore been understandably focused on hip dysplasia secondary to developmental dysplasia of the hips, with very limited literature regarding its outcomes in patient with neurogenic hip dysplasia secondary to cerebral palsy [2,9]. As most of the available literature on the Bernese periacetabular osteotomy is published based on developmental dysplasia of the hips, showing that there is no statistically significant difference in the outcomes regardless of the cause of the hip dysplasia in the current study then lends confidence that the results on the Bernese periacetabular osteotomy in the current literature can likely also be applied to patients with hip dysplasia secondary to cerebral palsy.
Thirdly, the current study is the only study in the available literature that has evaluated only patients under the age of 21. Consequently, to the authors’ knowledge, the current study also then represents the youngest age group of all the available studies that has evaluated the outcomes of the Bernese periacetabular osteotomy. This is important because outcomes following surgical management of hip dysplasia has been shown to be better when performed earlier in the course of the disease process, supporting the need for earlier intervention for these patients [3]. The good outcomes identified in the current study then supports the early use of the Bernese periacetabular osteotomy in children and adolescents with hip dysplasia once after the closure of the triradiate cartilage.
Another interesting finding of the study is that many of the patients with hip dysplasia secondary to cerebral palsy indeed require anteverting Bernese periacetabular osteotomy as advocated by Georgiadis et al2. Georgiadis et al discussed in their paper that the Bernese periacetabular osteotomy was originally designed for hip dysplasia secondary to developmental dysplasia of the hips, which are characterised mainly by anterolateral acetabular insufficiency [2]. However, owing to the pathomechanics of neurogenic hip dysplasia secondary to cerebral palsy, the location of acetabular insufficiency is frequently posterolateral and are often associated with retroversion, thereby necessitating specific attention to be paid to antevert the freed acetabular fragment during the surgical procedure2. This is in contrast to the traditional Bernese periacetabular osteotomy performed for developmental dysplasia of the hips [2]. This is possible due to the nature of the periacetabular osteotomy that allows complete mobilisation of the acetabulum from the bony pelvis to allow multi-directional reorientation [2]. Indeed, similar findings were noted in our cohort, with four out of six (66.7%) of the patients with hip dysplasia secondary to cerebral palsy having retroversion pre-operatively as compared to two out of five (40.0%) of the patients with hip dysplasia secondary to developmental dysplasia of the hips [2]. Three of these patients were also noted to have retroversion post-operatively due to insufficient correction intraoperatively, therefore highlighting the importance for extra attention to be paid to the hip version when performing the Bernese periacetabular osteotomy for hip dysplasia secondary to cerebral palsy.
Despite the above findings, this study faces limitations. The main and most important limitation of the study is that of a small sample size. This has limited the power of the statistical analysis, possibly explaining the lack of statistical significance identified in several of the parameters post-operatively. The small sample size is due to the low numbers of Bernese periacetabular osteotomy performed during early learning years in the institution. Despite so, significant learning points and results are obtained from this preliminary cohort which the authors believe can be beneficial to the rest of the Orthopaedic community, therefore the decision was made to publish these results despite the small sample size. Further studies with larger sample sizes will be conducted and published once there is adequate follow-up from these patients who are operated more recently. Secondly, the presence of concomitant varus derotational femoral osteotomy performed for patients with cerebral palsy could have introduced confounding bias. However, this is largely inevitable as patients with cerebral palsy often require concomitant procedures alongside periacetabular osteotomies. The study, however, allowed recognition that Bernese periacetabular osteotomy together with varus derotational femoral osteotomy can be a viable option for children and adolescents with closed triradiate cartilage and hip dysplasia secondary to cerebral palsy, and the outcomes are comparable to those who underwent Bernese periacetabular osteotomy for developmental dysplasia of the hips. Thirdly, while the study used Harris Hip Score and GMFCS to evaluate the pre-operative and post-operative outcomes of the patients, the authors acknowledge that more outcome scores could also have been used in the evaluation of the pre-operative and post-operative outcomes to further validate the results, and these would be included in further studies performed. Lastly, the current study has only evaluated the outcomes of the Bernese periacetabular osteotomies, and not for other osteotomies such as that of the Dega and San Diego osteotomies that can also be performed for patients with closed triradiate cartilage. The evaluation of only the Bernese periacetabular osteotomy could reduce the potential for confounding bias introduced by the evaluation of multiple osteotomies, and subsequent studies on the outcomes of other types of osteotomies could be performed [18].
Conflicts of interest:
The authors declare that there is no conflict of interest.
Funding:
The authors received no financial support for the research.
Research involving human participants and/or animals:
The study was performed in accordance with the Helsinki declaration.
Institutional Review Board/Ethics committee approval:
The study was performed in accordance with the ethical standards of the institutional research committee.
Informed consent:
Waiver of informed consent was approved by the institutional research committee.
References
- Oskoui M, Coutinho F, Dykeman J, et al. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55 (2013): 509-519.
- Georgiadis AG, Dutt V, Truong WH, et al. Anteverting Bernese periacetabular osteotomy in the treatment of neurogenic hip dysplasia in cerebral palsy. J Pediatr Orthop B 27 (2018): 473-478.
- Davids JR. Management of Neuromuscular Hip Dysplasia in Children with Cerebral Palsy: Lessons and Challenges. J Pediatr Orthop 1 (2018): S21-S27.
- Oto M, Sarikaya IA, Erdal OA, et al. Surgical reconstruction of hip subluxation and dislocation in children with cerebral palsy. Eklem Hastalik Cerrahisi 29 (2018): 8-12.
- Cobanoglu M, Cullu E, Omurlu I. The effect of hip reconstruction on gross motor function levels in children with cerebral palsy. Acta Orthop Traumatol Turc 52 (2018): 44-48.
- Ganz R, Klaue K, Vinh TS, et al. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res l (1988): 26-36.
- Siebenrock KA, Schöll E, Lottenbach M, et al. Bernese periacetabular osteotomy. Clin Orthop Relat Res 363 (1999): 9-20.
- Steppacher SD, Tannast M, Ganz R, et al. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res 466 (2008): 1633-1644.
- MacDonald SJ, Hersche O, Ganz R. Periacetabular osteotomy in the treatment of neurogenic acetabular dysplasia. J Bone Joint Surg Br 81 (1999): 975-978.
- Kuong EE, Gardner WT, Koljonen PA, et al. Normal radiographic parameters in paediatric pelvic radiographs from a Chinese population. J Pediatr Orthop B 26 (2017): 336-339.
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: With special referance to the complication of osteoarthritis. Acta Chir Scand Suppl 83 (1939): 1-135.
- Reimers J. The Stability of the Hip in Children: A Radiological Study of the Results of Muscle Surgery in Cerebral Palsy. Acta Orthopaedica Scandinavica 51 (1980): 1-100.
- Tannast M, Hanke MS, Zheng G, et al. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res 473 (2015): 1234-1246.
- Rhee PC, Woodcock JA, Clohisy JC, et al. Academic Network for Conservational Hip Outcomes Research Group. The Shenton line in the diagnosis of acetabular dysplasia in the skeletally mature patient. J Bone Joint Surg Am 93 (2011): 35-39.
- Jamali AA, Mladenov K, Meyer DC, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: High validity of the “cross-over-sign. Journal of Orthopaedic Research 25 (2007): 758-765.
- Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 81 (1999): 281-288.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51 (1969): 737-755.
- Murar J, Dias LS, Swaroop VT. San Diego pelvic osteotomy in patients with closed triradiate cartilage. J Child Orthop 12 (2018): 461-471.
