Association of Serum Homocysteine Level with Unexplained Recurrent Pregnancy Loss: A Case-Control Study
Article Information
Dr. Masuda Sultana1, Prof. Dr. Nahreen Akhtar2, Dr. Mousumi Saha3, Dr. Nowshafreen Chowdhury4, Dr. Parul Akhter5, Prof. Dr. Firoza Begum6
1Junior Consultant (Obstetrics and Gynecology), Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
2Professor, Department of Feto-maternal Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
3Assistant professor (Obstetrics and Gynecology), On deputation- Department of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
4Assistant professor (Obstetrics and Gynecology), Mugda Medical College and Hospital, Dhaka, Bangladesh.
5Associate Professor (Obstetrics and Gynecology), Sir Salimullah Medical College and Mitford Hospital, Dhaka, Bangladesh.
6Professor & Founding Chairman, Department of Feto-maternal Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
*Corresponding Author: Dr. Masuda Sultana, Junior Consultant (Obstetrics and Gynecology), Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Received: 18 December 2023; Accepted: 22 December 2023; Published: 30 December 2023
Citation: Dr. Masuda Sultana, Prof. Dr. Nahreen Akhtar, Dr. Mousumi Saha, Dr. Nowshafreen Chowdhury, Dr. Parul Akhter, Prof. Dr. Firoza Begum. Association of Serum Homocysteine Level with Unexplained Recurrent Pregnancy Loss: A Case-Control Study. Obstetrics and Gynecology Research. 6 (2023): 349-353.
Share at FacebookAbstract
Background:
Recurrent pregnancy loss (RPL) is a very stressful and painful experience for the couple. Recurrent pregnancy loss without apparent causative factor which may be identified in about 50% of cases known as unexplained recurrent pregnancy loss (RPL). Hyperhomocysteinaemia is considered a major risk factor for this problem which is related either to a hereditary defect within the methionine-homocysteine pathway or it might be acquired as a result of deficiencies of vitamin B12 and B9.
Aim of the study:
The aim of the study was to evaluate the association of serum homocysteine level with unexplained recurrent pregnancy loss.
Methods:
This case-control study was conducted in the outpatient department of Feto-maternal Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh during the period from May 2020 to April 2021. According to inclusion and exclusion criteria, 34 patients with unexplained recurrent pregnancy loss (RPL) and 34 age and BMI-matched control were selected from OPD during the one-year study period. A 3ml blood sample was collected from the antecubital vein of all 68 participants in a plain test tube and was sent to the Biochemistry Department of BSMMU to assess the serum homocysteine level using direct chemiluminescent technology by the Atellica TM IM analyzer. The results were noted in the questionnaire and the data were analyzed by using SPSS software.
Results:
In this study, serum homocysteine levels of the 68 participants of both the case and control groups were measured and analyzed. We found hyperhomocysteinemia among 5.9% of patients in the case group as the abnormal homocysteine level. The mean homocysteine level of case group patients was 8.15±8.11 (μmol/L) which was found as 6.23±1.47 (μmol/L) in the control group. But statistically, we did not find any significant difference between the groups regarding the homocysteine level; the p-value was found as 0.787.
Conclusion:
Serum homocysteine level has no significant association with unexplained recurrent pregnancy loss. Even, no significant difference was found when serum homocysteine levels were compared with the control in 1st, 2nd and 3rd-trimester pregnancy loss.
Keywords
Recurrent pregnancy loss (RPL); Homocysteine; Hyperhomocysteinemia; Thrombophilia
Recurrent pregnancy loss (RPL) articles Recurrent pregnancy loss (RPL) Research articles Recurrent pregnancy loss (RPL) review articles Recurrent pregnancy loss (RPL) PubMed articles Recurrent pregnancy loss (RPL) PubMed Central articles Recurrent pregnancy loss (RPL) 2023 articles Recurrent pregnancy loss (RPL) 2024 articles Recurrent pregnancy loss (RPL) Scopus articles Recurrent pregnancy loss (RPL) impact factor journals Recurrent pregnancy loss (RPL) Scopus journals Recurrent pregnancy loss (RPL) PubMed journals Recurrent pregnancy loss (RPL) medical journals Recurrent pregnancy loss (RPL) free journals Recurrent pregnancy loss (RPL) best journals Recurrent pregnancy loss (RPL) top journals Recurrent pregnancy loss (RPL) free medical journals Recurrent pregnancy loss (RPL) famous journals Recurrent pregnancy loss (RPL) Google Scholar indexed journals Homocysteine articles Homocysteine Research articles Homocysteine review articles Homocysteine PubMed articles Homocysteine PubMed Central articles Homocysteine 2023 articles Homocysteine 2024 articles Homocysteine Scopus articles Homocysteine impact factor journals Homocysteine Scopus journals Homocysteine PubMed journals Homocysteine medical journals Homocysteine free journals Homocysteine best journals Homocysteine top journals Homocysteine free medical journals Homocysteine famous journals Homocysteine Google Scholar indexed journals Hyperhomocysteinemia articles Hyperhomocysteinemia Research articles Hyperhomocysteinemia review articles Hyperhomocysteinemia PubMed articles Hyperhomocysteinemia PubMed Central articles Hyperhomocysteinemia 2023 articles Hyperhomocysteinemia 2024 articles Hyperhomocysteinemia Scopus articles Hyperhomocysteinemia impact factor journals Hyperhomocysteinemia Scopus journals Hyperhomocysteinemia PubMed journals Hyperhomocysteinemia medical journals Hyperhomocysteinemia free journals Hyperhomocysteinemia best journals Hyperhomocysteinemia top journals Hyperhomocysteinemia free medical journals Hyperhomocysteinemia famous journals Hyperhomocysteinemia Google Scholar indexed journals Thrombophilia articles Thrombophilia Research articles Thrombophilia review articles Thrombophilia PubMed articles Thrombophilia PubMed Central articles Thrombophilia 2023 articles Thrombophilia 2024 articles Thrombophilia Scopus articles Thrombophilia impact factor journals Thrombophilia Scopus journals Thrombophilia PubMed journals Thrombophilia medical journals Thrombophilia free journals Thrombophilia best journals Thrombophilia top journals Thrombophilia free medical journals Thrombophilia famous journals Thrombophilia Google Scholar indexed journals Obstetrics articles Obstetrics Research articles Obstetrics review articles Obstetrics PubMed articles Obstetrics PubMed Central articles Obstetrics 2023 articles Obstetrics 2024 articles Obstetrics Scopus articles Obstetrics impact factor journals Obstetrics Scopus journals Obstetrics PubMed journals Obstetrics medical journals Obstetrics free journals Obstetrics best journals Obstetrics top journals Obstetrics free medical journals Obstetrics famous journals Obstetrics Google Scholar indexed journals Gynecology articles Gynecology Research articles Gynecology review articles Gynecology PubMed articles Gynecology PubMed Central articles Gynecology 2023 articles Gynecology 2024 articles Gynecology Scopus articles Gynecology impact factor journals Gynecology Scopus journals Gynecology PubMed journals Gynecology medical journals Gynecology free journals Gynecology best journals Gynecology top journals Gynecology free medical journals Gynecology famous journals Gynecology Google Scholar indexed journals vitamin B12 articles vitamin B12 Research articles vitamin B12 review articles vitamin B12 PubMed articles vitamin B12 PubMed Central articles vitamin B12 2023 articles vitamin B12 2024 articles vitamin B12 Scopus articles vitamin B12 impact factor journals vitamin B12 Scopus journals vitamin B12 PubMed journals vitamin B12 medical journals vitamin B12 free journals vitamin B12 best journals vitamin B12 top journals vitamin B12 free medical journals vitamin B12 famous journals vitamin B12 Google Scholar indexed journals hyperhomocysteinemia articles hyperhomocysteinemia Research articles hyperhomocysteinemia review articles hyperhomocysteinemia PubMed articles hyperhomocysteinemia PubMed Central articles hyperhomocysteinemia 2023 articles hyperhomocysteinemia 2024 articles hyperhomocysteinemia Scopus articles hyperhomocysteinemia impact factor journals hyperhomocysteinemia Scopus journals hyperhomocysteinemia PubMed journals hyperhomocysteinemia medical journals hyperhomocysteinemia free journals hyperhomocysteinemia best journals hyperhomocysteinemia top journals hyperhomocysteinemia free medical journals hyperhomocysteinemia famous journals hyperhomocysteinemia Google Scholar indexed journals thyroid disorders articles thyroid disorders Research articles thyroid disorders review articles thyroid disorders PubMed articles thyroid disorders PubMed Central articles thyroid disorders 2023 articles thyroid disorders 2024 articles thyroid disorders Scopus articles thyroid disorders impact factor journals thyroid disorders Scopus journals thyroid disorders PubMed journals thyroid disorders medical journals thyroid disorders free journals thyroid disorders best journals thyroid disorders top journals thyroid disorders free medical journals thyroid disorders famous journals thyroid disorders Google Scholar indexed journals renal disease articles renal disease Research articles renal disease review articles renal disease PubMed articles renal disease PubMed Central articles renal disease 2023 articles renal disease 2024 articles renal disease Scopus articles renal disease impact factor journals renal disease Scopus journals renal disease PubMed journals renal disease medical journals renal disease free journals renal disease best journals renal disease top journals renal disease free medical journals renal disease famous journals renal disease Google Scholar indexed journals
Article Details
Introduction
Recurrent pregnancy loss (RPL) is a major reproductive problem, affecting about 1-5% of couples and is frequently accompanied by considerable psychological and social burden for the couple [1]. Recurrent pregnancy loss without apparent causative factor which may be identified in about 50% of cases known as unexplained RPL. The risk of recurrence increases with maternal age and the number of successive losses. Despite intense anatomic, endocrinologic and immunologic screening efforts, up to 50% of RPL remain unexplained [2]. Hyperhomocysteinemia, defined as an elevated level of homocysteine, is described as a risk factor for venous thromboembolism and adverse pregnancy outcomes such as recurrent miscarriages, pre-eclampsia, neural tube defects, placental abruption, intrauterine growth restriction and fetal death [3]. Increased homocysteine has negative pathological effects on vascular endothelium, atherogenesis and the activity of coagulation factors VIII and V, ultimately leads to an increase in the level of thrombin and platelet aggregation and results in venous thrombosis [3]. Maternal hyperhomocysteinemia also interferes with embryonic development through defective chorionic villous vascularization [6]. The complications that are associated with the increased level of homocysteine include recurrent miscarriages, preeclampsia, abortion, neural tube defects, intrauterine growth retardation, fetal death and venous thrombosis [3]. Several other pathologies, not related to pregnancy, also associated with hyperhomocysteinemia are vascular diseases and several age-related pathologies like Alzheimer’s disease, Parkinson’s disease, stroke and osteoporosis etc [5]. The normal levels of homocysteine range between 5 and 15 µmol/L. Based on the levels of homocysteine, hyperhomocysteinemia has been classified as mild/moderate (15- 30µmol/L), intermediate (30-100µmol/L) and severe (>100µmol/L) [5]. Folic acid and vitamin B12 supplementations can be given for acquired hyperhomocysteinemia. Low-dose aspirin and LMW heparin can be used to treat hyperhomocysteinemia due to inherited causes (MTHFR C677T & A1298C mutations). These treatments have been successfully used in different studies in patients with RPL having hyperhomocysteinemia and/or MTHFR mutation [6-8]. The major objective of this current study was to evaluate the association of serum homocysteine level with unexplained recurrent pregnancy loss.
Methodology
This was a case-control study conducted in the outpatient department of Feto-maternal Medicine, Bangabandhu Sheikh Mujib Medical University Hospital (BSMMU), Dhaka, Bangladesh during the period from May 2020 to April 2021. According to inclusion and exclusion criteria, 34 patients with unexplained recurrent pregnancy loss (RPL) and 34 age and BMI-matched control were selected from OPD during the one-year study period. The study was approved by the ethical committee of the mentioned hospital. Properly written consent was taken from all the participants before data collection. The whole intervention was conducted following the principles of human research specified in the Helsinki Declaration [9] and executed in compliance with currently applicable regulations and the provisions of the General Data Protection Regulation (GDPR) [10]. A convenient sampling technique was applied, according to the availability of the patients as per inclusion and exclusion criteria. As per the inclusion criteria of this study, patients who attended Feto-maternal OPD for periconceptional counseling for RPL and who had a history of consecutive two or more failed clinical pregnancies were included as cases. On the other hand, age and BMI-matched women (patient’s attendants) who had at least one successful pregnancy with no history of spontaneous pregnancy loss from both out-patient and inpatient departments of Feto-maternal Medicine, BSMMU were included as control group participants. Women who are diagnosed to have a known cause for RPL, Parental chromosomal abnormalities except for gene mutation, Type-I and Type-II diabetes mellitus, thyroid disorders, chronic renal disease, chronic HTN, PCOS, anatomic defects of the uterus and autoimmune disorders and cases received folate and vit B12 supplementation within previous three months were excluded. A 3ml blood sample was collected from the antecubital vein of all 68 participants in a plain test tube and was sent to the Biochemistry Department of BSMMU to assess the serum homocysteine level using direct chemiluminescent technology by the Atellica TM IM analyzer. The results were noted in the questionnaire and data were analyzed by using SPSS software version 22.0.
Result
In this study, it was found that the maximum (64.7%) patients in RPL (case) group and 67.7% in the normal (control) group were between 25 to 34 years of age. The mean age of the patients with RPL was (28.44±5.25), whereas the mean of the age of the control group was (29.15±4.72). There was no significant difference between these two groups in terms of age (P= 0.562). An Independent sample t-test was used to compare the mean BMI (Kg/m2) between case and control groups. The mean difference was not statistically significant (P = 0.208). So, it can be said that age and BMI of the case group (28.44±5.25 and 24.95±3.48) were matched with the control group (29.15±4.72 and 23.69±4.07). In comparison of homocysteine level, 32 (94.1%) patients were found to have normal (<15 μmol/L) level in RPL group and all 34 (100%) participants of control group have normal level of homocysteine. Only 2 (5.9%) have moderate or high (>15 μmol/L) homocysteine level in RPL group and zero percent on control group. The normality of S. homocysteine level data of all participants (case and control) was assessed by Kolmogorov-Smirnov test (p<0.05) and was found that the data were not normally distributed. So, Mann-Whitney U test was used to compare the mean S. homocysteine level between RPL group and control group and found that the difference was not statistically significant (P=0.787). So it can be said that mean S. homocysteine level of RPL patients (8.15±8.11) was not significantly different from control (6.23±1.47). In this study, it was also evident that there were no significant differences in S. homocysteine levels between patients who had pregnancy loss in 1st trimester, 2nd trimester, or combined 1st and 2nd trimester. Also, no significant difference was found when these were compared with the control.
|
Age group (In years) |
Case |
Control |
P value |
||
|
(n=34) |
(n=34) |
||||
|
n |
% |
n |
% |
||
|
18-24 yrs. |
7 |
20.6 |
5 |
14.7 |
|
|
25-34 yrs. |
22 |
64.7 |
23 |
67.7 |
|
|
35-40 yrs. |
5 |
14.7 |
6 |
17.6 |
|
|
Mean ± SD |
28.44 ± 5.25 |
29.15 ± 4.72 |
0.562 |
||
Table 1: Distribution of participants as per age. (N=68)
Table 1 showed that maximum (64.7%) patients in RPL group and 67.7% in control group were between 25 to 34 years of age. The mean age of the patients with RPL was (28.44±5.25), whereas the mean age of the control group was (29.15±4.72). There was no significant difference between these two groups in terms of age (P=0.562).
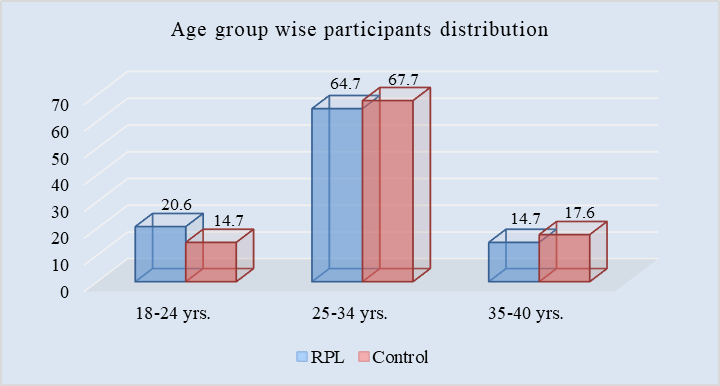
Figure I: Bar chart showed age group wise participants. (N=68)
|
BMI (Kg/m2) |
RPL |
Control |
P value |
||
|
(n=34) |
(n=34) |
||||
|
n |
% |
n |
% |
||
|
>18.5 |
0 |
0 |
1 |
2.9 |
0.208 |
|
18.5-24.9 |
18 |
52.9 |
21 |
61.8 |
|
|
25-29.9 |
12 |
35.3 |
9 |
26.5 |
|
|
≥30 |
4 |
11.8 |
3 |
8.8 |
|
|
Mean ± SD |
24.95 ± 3.48 |
23.69 ± 4.07 |
|||
|
Range |
20-32.4 |
18-31.2 |
|||
Table 2: Distribution of participants as per BMI. (N=68)
Independent sample t test was used to compare the mean BMI between RPL and control group in table 2. The mean difference was not statistically significant (P=0.208). So it can be said that BMI of RPL group (24.95±3.48) was matched with the control group (23.69±4.07). The range of BMI of RPL group 20-32.4 (Kg/m2) and control group 18-31.2 (Kg/m2).
|
S. homocysteine Level |
RPL |
Control |
||
|
(n=34) |
(n=34) |
|||
|
n |
% |
n |
% |
|
|
<15 μmol/L |
32 |
94.1 |
34 |
100 |
|
>15 μmol/L |
2 |
5.9 |
0 |
0 |
Table 3: Comparison of serum homocysteine level between the groups. (N=68)
Table 3 showed that only 2 (5.9%) of the patients in RPL group and none of the participants from control group have hyperhomocystienemia. The majority 32 (94.1%) patients in RPL group and all 34 (100%) participants of control group have normal homocysteine level.
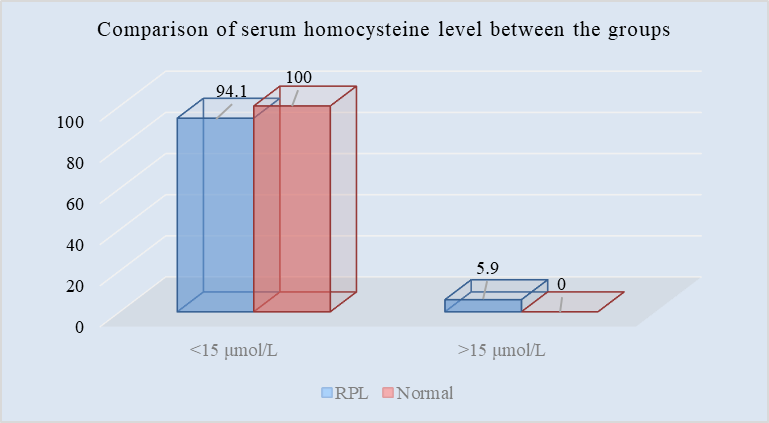
Figure II: Bar chart showed comparison of mean serum homocysteine level between the groups (N=68)
|
Tests of Normality |
|||
|
Kolmogorov-Smirnova |
|||
|
Statistic |
df |
Sig. |
|
|
S. homocysteine level |
0.307 |
87 |
0 |
*Here, 0.000 is not an absolute zero.
Table 4: Normality test of continuous variable. (N=68)
|
Parameter |
RPL |
Normal |
P value |
|
Mean ± SD |
Mean ± SD |
||
|
S. homocysteine level |
8.15 ± 8.11 |
6.23 ± 1.47 |
0.787 |
Table 5: Mean Serum Homocysteine Level in study population. (N=68)
In table 5, Mann-Whitney U test was used to compare the mean S. homocysteine level between RPL and control group. After checking the normality of S. homocysteine level data of all patient with Kolmogorov-Smirnov test (p<0.05), it was found that the data set was not normally distributed. The difference was not statistically significant (P=0.787). So it can be said that S. homocysteine level of RPL patients (8.15±8.11) was not significantly different from control (6.23±1.47).
|
Biochemical parameters |
RPL (n=34) |
Control (n=34) |
P value |
||
|
1st |
2nd |
(1st + 2nd) Trimester combined loss |
|||
|
Trimester loss |
Trimester loss |
Mean ±SD |
|||
|
Mean ±SD |
Mean ±SD |
||||
|
S. homocysteine Level |
8.37 ± 8.47 |
7.81 ±4.55 |
8.16±8.11 |
6.23±1.47 |
0.539 |
Table 6: Serum Homocysteine Level between two groups according to trimester. (N=68)
Table 6 showed that there are no significant differences in S. homocysteine level between patients who had pregnancy loss in 1st Trimester, 2nd Trimester or combined 1st and 2nd trimester. Also, no significant difference was found when these compared with the control.
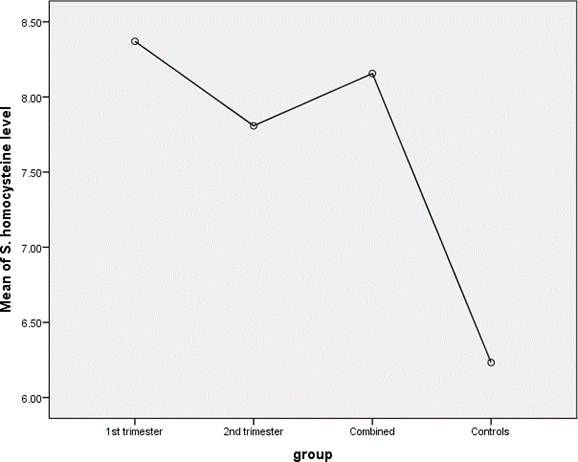
Figure III: Line diagram showed serum homocysteine level according to trimester between two groups. (N=68)
Discussion
This study aimed to evaluate the association of serum homocysteine level with unexplained recurrent pregnancy loss. Hyperhomocysteinemia is considered one of the major parts of thrombotic risk factors and many studies have investigated their potential association with RPL with inconclusive and controversial results. In this study, the mean age was 28.44±5.25 years in the case group and 29.15±4.72 years in the control group. The difference is not statistically significant (P=0.562) between the two groups. In another study, Xu et al. (2019) [11] found the mean age was 31.82 and 31.16 years for RPL and controls respectively (P=0.109). There were no statistically significant differences between the case and control groups in terms of age in both of the studies, which were similar to the current study. In our study, the mean BMI of RPL patients was 24.95 ± 3.48 Kg/m2 and that of control was 23.69 ± 4.07 Kg/m2 (P=0.208). So, the BMI of the RPL group was not significantly different from that of the controls which reflects perfect matching of BMI between the two groups. Creus et al. (2013) [12] also found a statistically non-significant difference in BMI between the case and control groups, which were 23.9±3.4 Kg/m2 and 24.7±3.9 Kg/m2 respectively. In Yousefian et al., (2014) [13] BMI of RPL patients and controls were found to be 24.2±2.5 and 25.4±2.7 Kg/m2 respectively (p=0.23) which was also not significant. Hyperhomocysteinemia was present in 5.9% (2 patients) of the study population among the RPL group, whereas no one had this in the control group. So, the current study found that it may be a cause of unexplained RPL in a few patients. Among the two patients, one had intermediate hyperhomocysteinemia (S. Hcy level was 50 μmol/l). Mukhopadhyay et al., (2017) [8] found hyperhomocysteinemia in 32% of RPL patients in their prospective study, they defined hyperhomocysteinemia when S. Hcy level≥12 μmol/l. The study conducted by Puri et al. (2013) [14] found that hyperhomocysteinemia (considered level ≥13 μmol/l) was present among 65.06% of the cases as compared to only 20.94% of the controls and the difference was statistically significant with a P-value < 0.0001. The odds ratio also revealed a 7.02-fold increased risk of RPL (OR=7.02; CI=3.8558-12.8094, P < 0.0001) depicting hyperhomocysteinemia as an independent risk factor for RPL. It was observed in this study that the mean homocysteine level of RPL patients was 8.15±8.11 μmol/l was not significantly different from the control group (6.23±1.47 μmol/l) with a P-value 0.878. S. homocysteine level was also divided according to different trimester loss and compared with the control which was also found not significant (P-value=0.539). Creus et al., (2013) [12] also found in their study that the mean homocysteine level in the case group was not significantly different from the control (7.7±2.3 vs. 8.1±3.3 μmol/l). In Zarfeshan Fard et al., (2019) [3], the mean homocysteine level was also not different significantly between the case group and control (6.58±1.84 vs. 5.50±0.81 μmol/l). The study of Govindaiah et al., (2009) [15] found that hyperhomocysteinemia increased the risk of RPL and the mean homocysteine level in the case group was higher significantly than the control (mean: 11.6±5.0 versus 8.6±4.2 μmol/l, OR=4.48). The review article titled “A Novel Review of Homocysteine and pregnancy complications” by Dai et al., (2021) [16] reviewed 7 articles that analyzed the association of serum homocysteine and RPL and found that 5 articles supported and 2 articles rejected the association between homocysteine levels and RPL. The association between serum homocysteine level and RPL susceptibility has been widely researched, with contradictory results.
Limitation of the Study
The study population was only recruited from one selected hospital in Dhaka city. So, the results of the study may not reflect the exact scenario of the country. The present study was conducted over a very short period and the study was conducted on a relatively small sample size, which was also a limitation.
Conclusion and Recommendation
As per the findings of this current study, we can conclude that serum homocysteine level has not any significant association with unexplained recurrent pregnancy loss. Even, not any significant difference is found when serum homocysteine levels are compared with the control in 1st, 2nd and 3rd-trimester pregnancy loss. All the findings of this current study may be helpful in further similar studies.
References
- Tian Chen, H., Yang, X, Lu, M. "Methylenetetrahydrofolate reductase gene polymorphisms and recurrent pregnancy loss in China: a systematic review and meta-analysis". Archives of gynecology and obstetrics 293 (2016): 283-290.
- Rai, V. "Methylenetetrahydrofolate reductase C677T polymorphism and recurrent pregnancy loss risk in Asian population: a meta-analysis". Indian Journal of Clinical Biochemistry 31 (2016): 402-413.
- Zarfeshan Fard, Y., Kooshkaki, O., Kordi Tammandani, D, et al. "Investigation of the association between C677T polymorphism of the MTHFR gene and plasma homocysteine level in recurrent fetal miscarriage". Journal of Obstetrics and Gynaecology Research 45 (2019): 1442-1447.
- Kutteh, W. H, Triplett, D. A. "Thrombophilias and Recurrent Pregnancy Loss". Semin Reprod Med, 24 (2006): 054-066.
- Kumar, A., Palfrey, H. A., Pathak, R., et al. "The metabolism and significance of homocysteine in nutrition and health". Nutrition & metabolism 14 (2017): 78.
- Brenner, B., Hoffman, R., Carp, H., et al. "Efficacy and safety of two doses of enoxaparin in women with thrombophilia and recurrent pregnancy loss: the LIVE-ENOX study". Journal of Thrombosis and Haemostasis 3 (2005): 227-229.
- Chakraborty, P., Banerjee, S., Saha, P., et al. "Aspirin and low-molecular weight heparin combination therapy effectively prevents recurrent miscarriage in hyperhomocysteinemic women". PloS one, 8 (2013): e74155.
- Mukhopadhyay, I., Pruthviraj, V., Rao, P, Biswas, M. "Hyperhomocysteinemia in recurrent pregnancy loss and the effect of folic acid and vitamin B12 on homocysteine levels: a prospective analysis". Int J Reprod Contracept Obstet Gynecol, 6 (2017): 2258-2261.
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization 79 (2001): 373 - 374.
- Voigt, Paul, Axel von dem Bussche. "Enforcement and fines under the GDPR." The EU General Data Protection Regulation (GDPR). Springer, Cham (2017): 201-217.
- Xu, Y., Ban, Y., Ran, L., et al. "Relationship between unexplained recurrent pregnancy loss and 5, 10-methylene tetrahydrofolate reductase polymorphysms". Fertility and Sterility 111 (2019): 597-602.
- Creus, M., Deulofeu, R., Peñarrubia, J., et al. "Plasma homocysteine and vitamin B12 serum levels, red blood cell folate concentrations, C677T methylene tetrahydrofolate reductase gene mutation and risk of recurrent miscarriage: a case-control study in Spain". Clinical chemistry and laboratory medicine 51 (2013): 693-699.
- Yousefian, E., Kardi, M. T, Allahveisi, A. "Methylenetetrahydrofolate reductase C677T and A1298C polymorphism in Iranian women with idiopathic recurrent pregnancy losses". Iranian Red Crescent Medical Journal 16 (2014): e16763.
- Puri, M., Kaur, L., Walia, G. K., et al. "MTHFR C677T polymorphism, folate, vitamin B12 and homocysteine in recurrent pregnancy losses: a case-control study among North Indian women". Journal of perinatal medicine, 41 (2013): 549-554.
- Govindaiah, V., Naushad, S.M., Prabhakara, K., et al. "Association of parental hyperhomocysteinemia and C677T Methylene tetrahydrofolate reductase (MTHFR) polymorphism with recurrent pregnancy loss". Clinical biochemistry, 42 (2009): 380-386.
- Dai, C., Fei, Y., Li, J., et al. "A Novel Review of Homocysteine and Pregnancy Complications". BioMed Research International, 111 (2021): 590-603.
