Association of Assisted Reproductive Technology with the Risk of Congenital Heart Defects: A 5-Year Retrospective Study – Experience from a Tertiary Maternity Hospital in Bucharest
Article Information
Ioana Rosca1,2, Alina Turenschi8, Alexandra Raris-Denisa5, Daniela-Eugenia Popescu6,7*, Cristina Stoica4, Andreea Carp-Veliscu1,4, Ana-Maria-Cristina Jura9, Andreea Teodora Constantin1,3
1University of Medicine and Pharmacy “Carol Davila”, Bucharest
2Clinical Hospital of Obstetrics and Gynecology “Prof. Dr. P. Sârbu”, Neonatology Department, Bucharest
3National Institute for Mother and Child Health “Alessandrescu-Rusescu”, Pediatrics Department, Bucharest
4Clinical Hospital of Obstetrics and Gynecology “Prof. Dr. P. Sârbu”, Obstetrics and Gynecology Department, Bucharest
5Emergency Clinical Hospital for Children "Marie Curie" Bucharest
6Department of Obstetrics-Gynecology and Neonatology, “Victor Babes” University of Medicine and Pharmacy, Timisoara
7Department of Neonatology, Premiere Hospital, Regina Maria Health Network, Timisoara
8Pediatric Hospital Ploiesti
9"Louis Turcanu" Emergency Clinical Hospital for Children, Timisoara
*Corresponding Author: Daniela-Eugenia Popescu, Department of Obstetrics-Gynecology and Neonatology, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania.
Received: 24 November 2023; Accepted: 01 December 2023; Published: 06 December 2023
Citation: Ioana Rosca, Alina Turenschi, Alexandra Raris-Denisa, Daniela-Eugenia Popescu, Cristina Stoica, Andreea Carp-Veliscu, Ana-Maria-Cristina Jura, Andreea Teodora Constantin. Association of Assisted Reproductive Technology with the Risk of Congenital Heart Defects: A 5-Year Retrospective Study – Experience from a Tertiary Maternity Hospital in Bucharest. Obstetrics and Gynecology Research. 6 (2023): 281-294.
Share at FacebookAbstract
Congenital heart disease (CHD) represents a group of abnormalities present at birth, and a relevant cause of perinatal mortality. Infertility is a recurrent condition in medical practice, affecting almost 7% of couples. Causes are multiple and complex, including genetic and environmental factors [1]. Assisted Reproductive Technology (ART) treatment for infertility uses in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI) and oocyte donation (OD). Studies assessing the CHD risk in IVF/ ICSI pregnancies, showed a higher probability as opposed to spontaneous conceptions [2]. The study’s aim was to evaluate CHD prevalence in ART pregnancies over 5 years (January 2016-December 2020) and highlight the need of cardiac screening. We conducted a cross-sectional study at the Clinical Hospital of Obstetrics and Gynecology "Prof. Dr. Panait Sârbu", with a compartment dedicated to infertility. 349 ART newborns and 18,170 spontaneous conceptions were included in the analysis. The prevalence of congenital heart malformations in ART pregnancies was 3,15% and in spontaneous pregnancies only 0,51% (p<0,001). The most common CHDs were ventricular septal defect and coarctation of the aorta. We reported 11 cases, but the most challenging was an extremely preterm infant with patent ductus arteriosus (PDA), unresponsive to pharmacological therapy, requiring surgical ligation. PDA is frequent in preterms, and required for survival in some CHDs. Our paper shows that neonates conceived through ART have an increased risk of developing CHD compared to spontaneous conceptions. If CHD suspicion occurs, monitoring must happen in a unit capable of managing high-risk cases such as intrauterine growth restriction (IUGR) or prematurity.
Keywords
Congenital heart defects; assisted reproductive technology; Neonatal echocardiography; Persistent ductus arteriosus; Infertility
Congenital heart defects articles Congenital heart defects Research articles Congenital heart defects review articles Congenital heart defects PubMed articles Congenital heart defects PubMed Central articles Congenital heart defects 2023 articles Congenital heart defects 2024 articles Congenital heart defects Scopus articles Congenital heart defects impact factor journals Congenital heart defects Scopus journals Congenital heart defects PubMed journals Congenital heart defects medical journals Congenital heart defects free journals Congenital heart defects best journals Congenital heart defects top journals Congenital heart defects free medical journals Congenital heart defects famous journals Congenital heart defects Google Scholar indexed journals assisted reproductive technology articles assisted reproductive technology Research articles assisted reproductive technology review articles assisted reproductive technology PubMed articles assisted reproductive technology PubMed Central articles assisted reproductive technology 2023 articles assisted reproductive technology 2024 articles assisted reproductive technology Scopus articles assisted reproductive technology impact factor journals assisted reproductive technology Scopus journals assisted reproductive technology PubMed journals assisted reproductive technology medical journals assisted reproductive technology free journals assisted reproductive technology best journals assisted reproductive technology top journals assisted reproductive technology free medical journals assisted reproductive technology famous journals assisted reproductive technology Google Scholar indexed journals Neonatal echocardiography articles Neonatal echocardiography Research articles Neonatal echocardiography review articles Neonatal echocardiography PubMed articles Neonatal echocardiography PubMed Central articles Neonatal echocardiography 2023 articles Neonatal echocardiography 2024 articles Neonatal echocardiography Scopus articles Neonatal echocardiography impact factor journals Neonatal echocardiography Scopus journals Neonatal echocardiography PubMed journals Neonatal echocardiography medical journals Neonatal echocardiography free journals Neonatal echocardiography best journals Neonatal echocardiography top journals Neonatal echocardiography free medical journals Neonatal echocardiography famous journals Neonatal echocardiography Google Scholar indexed journals Persistent ductus arteriosus articles Persistent ductus arteriosus Research articles Persistent ductus arteriosus review articles Persistent ductus arteriosus PubMed articles Persistent ductus arteriosus PubMed Central articles Persistent ductus arteriosus 2023 articles Persistent ductus arteriosus 2024 articles Persistent ductus arteriosus Scopus articles Persistent ductus arteriosus impact factor journals Persistent ductus arteriosus Scopus journals Persistent ductus arteriosus PubMed journals Persistent ductus arteriosus medical journals Persistent ductus arteriosus free journals Persistent ductus arteriosus best journals Persistent ductus arteriosus top journals Persistent ductus arteriosus free medical journals Persistent ductus arteriosus famous journals Persistent ductus arteriosus Google Scholar indexed journals Infertility articles Infertility Research articles Infertility review articles Infertility PubMed articles Infertility PubMed Central articles Infertility 2023 articles Infertility 2024 articles Infertility Scopus articles Infertility impact factor journals Infertility Scopus journals Infertility PubMed journals Infertility medical journals Infertility free journals Infertility best journals Infertility top journals Infertility free medical journals Infertility famous journals Infertility Google Scholar indexed journals in vitro fertilization articles in vitro fertilization Research articles in vitro fertilization review articles in vitro fertilization PubMed articles in vitro fertilization PubMed Central articles in vitro fertilization 2023 articles in vitro fertilization 2024 articles in vitro fertilization Scopus articles in vitro fertilization impact factor journals in vitro fertilization Scopus journals in vitro fertilization PubMed journals in vitro fertilization medical journals in vitro fertilization free journals in vitro fertilization best journals in vitro fertilization top journals in vitro fertilization free medical journals in vitro fertilization famous journals in vitro fertilization Google Scholar indexed journals hypertension articles hypertension Research articles hypertension review articles hypertension PubMed articles hypertension PubMed Central articles hypertension 2023 articles hypertension 2024 articles hypertension Scopus articles hypertension impact factor journals hypertension Scopus journals hypertension PubMed journals hypertension medical journals hypertension free journals hypertension best journals hypertension top journals hypertension free medical journals hypertension famous journals hypertension Google Scholar indexed journals gestational diabetes articles gestational diabetes Research articles gestational diabetes review articles gestational diabetes PubMed articles gestational diabetes PubMed Central articles gestational diabetes 2023 articles gestational diabetes 2024 articles gestational diabetes Scopus articles gestational diabetes impact factor journals gestational diabetes Scopus journals gestational diabetes PubMed journals gestational diabetes medical journals gestational diabetes free journals gestational diabetes best journals gestational diabetes top journals gestational diabetes free medical journals gestational diabetes famous journals gestational diabetes Google Scholar indexed journals prematurity articles prematurity Research articles prematurity review articles prematurity PubMed articles prematurity PubMed Central articles prematurity 2023 articles prematurity 2024 articles prematurity Scopus articles prematurity impact factor journals prematurity Scopus journals prematurity PubMed journals prematurity medical journals prematurity free journals prematurity best journals prematurity top journals prematurity free medical journals prematurity famous journals prematurity Google Scholar indexed journals IUGR articles IUGR Research articles IUGR review articles IUGR PubMed articles IUGR PubMed Central articles IUGR 2023 articles IUGR 2024 articles IUGR Scopus articles IUGR impact factor journals IUGR Scopus journals IUGR PubMed journals IUGR medical journals IUGR free journals IUGR best journals IUGR top journals IUGR free medical journals IUGR famous journals IUGR Google Scholar indexed journals
Article Details
Introduction
According to different researchers, the word "infertility" has been used to designate a diverse range of patients. Adverse perinatal outcomes may also be influenced by certain maternal traits linked to infertility. Age, parity, and socioeconomic status are only some of the key factors that differentiate women who use assisted reproduction from fertile ones. These have an important impact on pregnancy outcomes. The most significant negative predictive factor concerning pregnancy was identified as being advanced maternal age, which increased in the last 25-30 years [3]. Few studies have taken into consideration the impact of additional possible cofactors such as parity, smoking status, alcohol intake, infertility duration, and pre-existing maternal illness, even if certain authors have made an effort to account for recognized confounders. Recent research indicates that the duration and origin of infertility are significant indicators of perinatal outcomes [4-6] and future research should take these aspects into account.
Although in vitro fertilization (IVF) was initially used in England in 1978, the first successful ART birth in Romania occurred on the 6th of February, 1996, a long time later. The number of clinics providing assisted reproductive services has increased in our country in the last years. However, the number of clinics that have been performing ART and the number of ART newborns each year are unclear due to the lack of precise statistics on ART [7-9]. Since 2011, the Romanian Government introduced a national sponsorship program for infertile couples, providing financial aid to cover a part of the ART procedure and, by 2022, this initiative was maintained with a subsidy of roughly 3000 euros. [9,10]. “Prof. Dr. Panait Sârbu” Hospital is one of the few public hospitals in Romania where ART is practiced, while most of them are carried out in private institutions.
The exact underlying mechanisms associating assisted reproductive technologies (ARTs) and congenital heart disease (CHD) are not fully understood. However, some researchers believe that the increased risk may be due to factors such as the use of fertility drugs and the manipulation of embryos during the ART procedures [11]. There are some studies assessing the risk of CHD in pregnancies conceived after ART, indicating a slightly higher risk in this group compared to spontaneous conceptions [12,13]. ART is also associated with a higher probability of complications such as hypertension, gestational diabetes, prematurity, IUGR and other perinatal difficulties [14].
Congenital heart disease can range from mild to severe and can affect the heart's structure, function, or both. Some examples of CHDs include atrial septal defects, ventricular septal defects, tetralogy of Fallot, and transposition of the great arteries [11]. In most cases, the etiology remains unknown. Chromosomal anomalies and genetic mutations are responsible for less than 15% of CHD. Therefore, it is essential to evaluate new potential risk factors in order to improve the CHD detection rate, and, if possible, the outcome as well [13].
Objectives
The aim of the study was to assess whether congenital heart defects (CHDs) occur more often in pregnancies conceived through ART compared to spontaneous ones.
Our goal is to highlight the result of interdisciplinary collaboration between Neonatology, Obstetrics, Pediatric Cardiology, and Pediatric Cardiac Surgery using a more rapid case identification and efficient management, emphasized by a favorable long-term patient prognosis.
Material and Method
We conducted a cross-sectional observational study, over a 5-year timeframe (between January 2016 and December 2020), investigating neonates with cardiovascular malformations obtained through in vitro fertilization, admitted to our clinic, the Clinical Hospital of Obstetrics and Gynecology “Prof. Dr. Panait Sârbu”, in Bucharest, Romania. The study cohort included 104 patients diagnosed with congenital heart disease during this timeframe. Eleven of them were conceived via in vitro fertilization. Inclusion criteria consisted of: newborns with cardiovascular malformations, obtained using IVF. Exclusion criteria were incomplete data, or neonates resulted from natural conception. Data was collected from the hospital's electronic register using simple random sampling to reduce bias. Information gathering was done using Microsoft Excel and was analyzed with IBM SPSS version 26. Prematurity refers to a gestational age below 37 weeks, with subcategories of late preterm (32-37 weeks of gestation), very preterm (28-32 weeks), and extremely preterm (<28 weeks)[15].
We assembled data from naturally conceived newborns and those obtained through ART, such as: antenatal diagnosis, place of birth (our hospital or other maternities), gestational age, gender, extracardiac anomalies (multiple malformations) or chromosomal anomaly, IUGR (intrauterine growth restriction), Apgar score, complications, the need for computer tomography angiogram (CT angiogram), orotracheal intubation, the demand for immediate surgery after birth and death (exitus).
If prenatal CHD was suspected, fetal echocardiography was carried out, and the pregnant woman was promptly referred to a specialist. If the diagnosis was made postnatally, based on clinical and paraclinical signs, the newborn was evaluated by a Pediatric Cardiology specialist. All newborns underwent neonatal cardiological pulse oximetry screening.
Every CHD patient included in the study was referred for Pediatric Cardiology examination and echocardiography, which were carried out by physicians with advanced training and expertise in identifying cardiac malformations. The consulted Pediatric Cardiologists are skilled, experienced in this field, and have competences in cardiac scanning.
The ultrasound machine used during the study period was Vivid E95 (GE Vingmed Ultrasound AS, Norway), equipped with multifrequency convex transducers.
The prevalence of CHDs in our group with neonates conceived using ART was calculated as follows: prevalence of CHDs (3,15%) = Total number of CHDs diagnosed during the period of the study in ART neonates/Total number of neonates obtained through ART. The Fisher's Exact Test was used to compare the prevalence of CHD between spontaneous and AR obtained newborns.
Results
During the five-year study period (from 2016 to 2020), 18,519 newborns were admitted to our clinic. Of them, 349 were obtained using ART technology (Figure 1). 11 of the ART conceived newborns were diagnosed with congenital heart defects (CHD), some based on fetal morphologies and others after neonatal screening performed in the maternity ward.
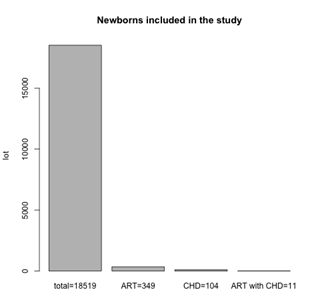
Figure 1: Newborns included in the study
The prevalence of congenital heart malformations in ART pregnancies was 11/349 (3,15%) and total CHD events in spontaneous population were 93/18170 (0,51%), (104-11)/ (18.519-349) =93/18.170=0.0051). The risk of CHD was significantly increased in the ART group compared to the spontaneous conception group (Table 1).
|
Neonates |
Naturally conceived neonates |
Assisted reproductive technology neonates |
p* |
|
Total 18519 |
18170 |
349 |
<0,001 |
|
CHD 104 (0,56%) |
93 (0,51%) |
11 (3,15%) |
|
*Fisher's Exact Test
Table 1: Prevalence of CHD in study group
According to Fisher's Exact Test the difference between the prevalence of CHD in natural pregnancy vs IVF (0,51% vs 3,15%) is statistically significant (p<0,001).
The characteristics of the study group are presented in Table2. Three of the newborns included in the study were diagnosed with CHD antenatally, requiring confirmation of the diagnosis using postnatal specialist consult. Due to immaturity and fetal distress, more than half of the newborns (premature babies, and those with IUGR) were referred for cardiological examination. It is important to emphasize that no child from the IVF lot presented multiple malformation syndromes or chromosomal anomalies. All of them were born in our maternity; they were not transferred from another unit. Most of them were male (7), and 4 were female. Multiple cases (36,36%) had IUGR, 4 were preterm babies (late and extremely preterm) and 3 were born at term, having normal weight. 72,7% of the 11 newborns with CHD had an Apgar score >8, and only 9,09% had moderate to severe perinatal hypoxia with an Apgar score <5.
|
Variables |
Newborn babies obtained through ART (n=11) |
Naturally conceived newborn babies (n=104) |
|
Suspected CHD (antenatal diagnosis) |
3 |
23 |
|
Birth - our maternity |
11 |
88 |
|
Birth - other maternities |
0 |
5 |
|
Males |
7 |
53 |
|
Females |
4 |
40 |
|
Extracardiac anomaly (multiple malformations) or chromosomal anomaly |
0 |
13 |
|
Term neonates & normal weight |
3 |
8 |
|
Late preterm |
2 |
25 |
|
LBW |
1 |
8 |
|
ELBW |
1 |
3 |
|
IUGR |
4 |
13 |
|
Apgar score 8-10 |
8 |
64 |
|
Apgar score 6-7 |
2 |
18 |
|
Apgar score <5 |
1 |
11 |
|
Complications - mild-moderate PPHN |
3 |
19 |
|
Complications - severe PPHN |
1 |
4 |
|
Other complications |
0 |
3 |
|
CT angiogram |
1 |
10 |
|
Orotracheal intubation |
2 |
29 |
|
Surgery immediately after birth - in our country - another hospital |
3 |
10 |
|
Surgery immediately after birth - another country (San Donato, Lyon) |
0 |
14 |
|
Surgery immediately after birth - in our unit |
1 |
0 |
|
Death |
1 |
7 |
Abbreviation: CHD, congenital heart disease, IUGR intrauterine growth restriction, LBW low birth weight VLBW very low birth weight, ELBW extremely low birth weight, PPHN persistent pulmonary hypertension of the newborn, computed tomography (CT) angiogram
Table 2: Characteristics of the study group
27,2% of the 11 neonates were transferred to a cardiology surgical correction center in Bucharest and one of them was managed in our neonatal intensive care unit. Despite the complexity of CHD and the association of the majority of them with prematurity and IUGR, the preoperative survival rate was 90,9%. Only one death occurred.
A third of the patients in the study experienced complications, such as pulmonary hypertension, 2 of which required orotracheal intubation and mechanical ventilation. One computed tomography angiography was performed during the study, for the CHD group obtained using in vitro fertilization.
The most common CHD encountered was ventricular septal defect (VSD) (Figure 2a, b) and coarctation of the aorta (Figure 3a, b), followed by moderate pulmonary artery stenosis (Figure 4a, b, c), patent ductus arteriosus (Figure 5a, b), tetralogy of Fallot (Figure 6a, b) and severe aortic valve stenosis (Figure 7a, b), seen in Table 3.
|
Congenital heart disease in neonates |
n =11 |
|
Ventricular Septal Defect |
4 |
|
Coarctation of the Aorta |
3 |
|
Moderate Pulmonary Stenosis |
1 |
|
Patent Ductus Arteriosus |
1 |
|
Tetralogy of Fallot |
1 |
|
Sever Aortic Valve Stenosis |
1 |
Table 3: Congenital heart disease diagnosed in the study group (n=11 neonates)
Parasternal short axis: large perimebranous ventricular septal defect. RA, right atrium; LA, left atrium; LVOT, left ventricle outflow tract; RVOT, right ventricle outflow tract; VSD, ventricular septal defect.
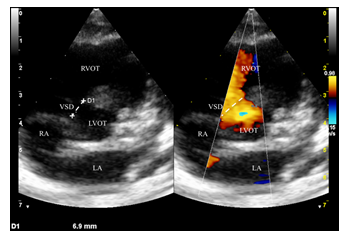
Figure 2a: Ventricular septal defect
Apical 5 chamber: subaortic ventricular septal defect. RV, right ventricle; LV, left ventricle; IVS, interventricular septum; VSD, ventricular septal defect; LA, left atrium; Ao, aorta.
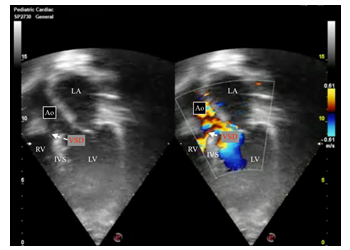
Figure 2b: Ventricular septal defect
Suprasternal long axis view showing discrete preductal coarctation. There is a calibre discrepancy between the ascending aorta (Asc Ao) and transverse arch. AoD, descending aorta; Asc Ao, ascending aorta; RPA, right pulmonary artery.
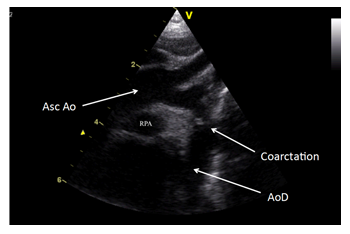
Figure 3a: Coarctation of the aorta
Subcostal Abdominal Aorta Doppler signal flow: severe coarctation of the aorta with reduced pulse width.
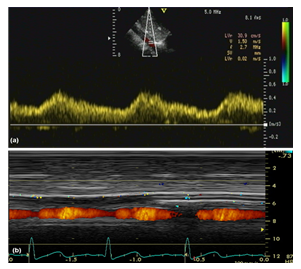
Figure 3b: Coarctation of the aorta
Parasternal short axis: turbulence flow starting at the pulmonary valve region (pulmonary valve stenosis). AoV, aortic valve; RV, right ventricle; RVOT, right ventricle outflow tract; PV, pulmonary valve
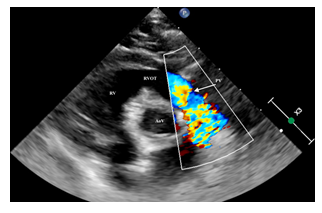
Figure 4a: Pulmonary valve stenosis
Parasternal short axis: pulmonary valve stenosis in a newborn. AoV, aortic valve; RV, right ventricle; RVOT, right ventricle outflow tract; PV, pulmonary valve; RPA, right pulmonary artery; LPA, left pulmonary artery; RA, right atrium.
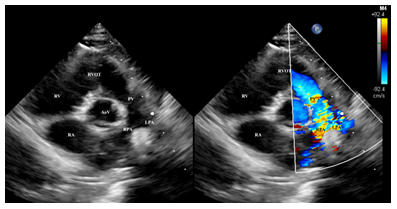
Figure 4b: Pulmonary valve stenosis
Parasternal short axis anterior showing a continuous doppler of the pulmonary valve gradient (moderate pulmonary stenosis). PV, pulmonary valve.
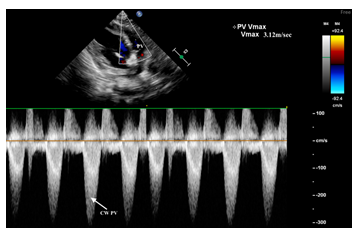
Figure 4c: Pulmonary valve stenosis
High left parasternal view – “ductal view” showing a large arterial duct. RPA, right pulmonary artery; LPA, left pulmonary artery; PDA, patent ductus arteriosus; Dao, descending aorta.
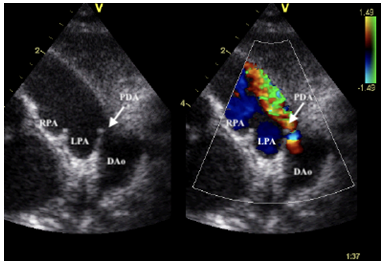
Figure 5a: Patent ductus arteriosus
Subcostal oblique view showing an arterial duct. RPA, right pulmonary artery; LPA, left pulmonary artery; PDA, patent ductus arteriosus; MPA, main pulmonary artery
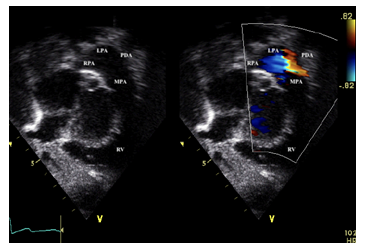
Figure 5b: Patent ductus arteriosus
Parasternal short axis showing a large perimembranous ventricular septal defect (VSD) with anterior deviation of the outlet septum (OS) and, increased turbulence in the right ventricle outflow tract (RVOT). LA, left atrium; LAA, left atrial appendage; RA, right atrium; AoV, aortic valve; VSD, ventricle septal defect; OS, outlet septum; RVOT, right ventricle outflow tract
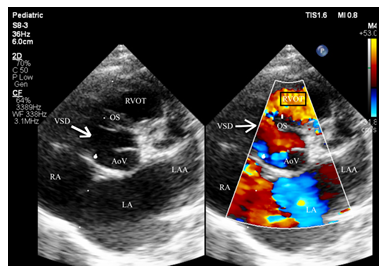
Figure 6a: Tetralogy of Fallot
Subcostal right anterior oblique view showing the infundibular obstruction of the right ventricle outflow tract with v max 4.82m/sec (severe obstruction) of a newborn with tetralogy of Fallot.
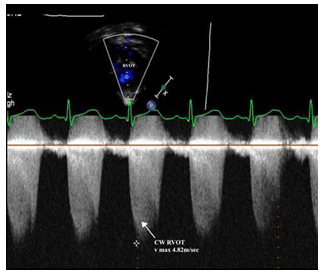
Figure 6b: Tetralogy of Fallot
Parasternal long axis- Reduced opening of aortic valve in systole due to aortic valve stenosis. LA, left atrium; LV, left ventricle; AoV, aortic valve; IVS, interventricular septum; Asc Ao, ascending aorta; RV, right ventricle.
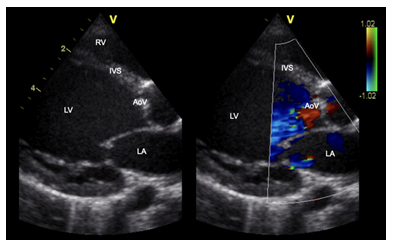
Figure 7a: Severe aortic valve stenosis
Apical 5 Chamber showing turbulent flow starting from aortic valve region (Nyquis high) representing severe aortic valve stenosis. RV, right ventricle; LV, left ventricle; AoV, aortic valve
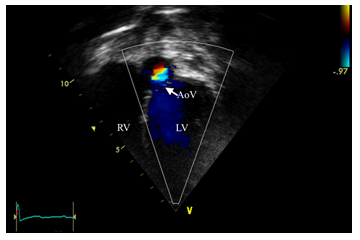
Figure 7b: Severe aortic valve stenosis
Discussion
Detection of congenital heart disease is strongly related to the corresponding methodology/protocol employed in hospitals for screening/diagnosing CHD, as stated in a recent paper published in 2023[16].
In our study, the prevalence of congenital heart malformations in ART pregnancies was 11/349 (3,15%) and total CHD events were 104/18519 (0,56%). The risk of CHD was increased significantly in the ART group compared to the spontaneous conception group (p<0,001). These results are consistent with data from current literature, which is a topic that many researchers are interested in. [13].
We are one of the first Romanian 3rd level Maternity Hospitals to have an ART compartment. In our hospital, ART pregnancies can be followed to term and if complications occur (such as CHD, prematurity or with any other pathology) they do not require transfer to other hospital units. A third (36,3%) of our study group was represented by IUGR newborns, which is an indicator for intrauterine stress. According to specialized literature, infants with IUGR are at risk for perinatal difficulties and often require specific care during the first few days of life. Therefore, if possible, delivery should take place in a center with a Neonatal Intensive Care Unit (NICU) or special care nursery. The delivery team should be prepared to manage fetal distress, perinatal depression, meconium aspiration, hypoxia, hypoglycemia, and heat loss [17-20]. In our study, two significant pathologies requiring rigorous management could be observed: IUGR and CHD. Compared to appropriate for gestational age (AGA) babies, IUGR infants have a higher incidence of neonatal morbidity and mortality [17]. Only one of the neonates from our study group did not survive, due to a complex CHD, not because of IUGR. The etiology of IUGR can be fetal, placental and maternal, one of the fetal causes being congenital malformation [18,20,21]. Owing to the fact that a maternal cause led to infertility or that the couple required ART, this contributes to an interrelationship between ART, IUGR and CHD.
Intrauterine growth restriction means a fetus does not grow at the expected rate during pregnancy. The condition can lead to a wide range of neonatal health issues, including low birth weight, respiratory problems, and developmental delays.
Several studies suggested that ART may be associated with an increased risk of IUGR in pregnancies obtained using this procedure. A 2017 systematic review and meta-analysis, published in the journal Fertility and Sterility, analyzed data from 16 studies and found that the risk of IUGR was higher in pregnancies conceived through ART compared to spontaneous conception [22].
The exact underlying mechanisms between the ART and IUGR association are not fully understood. However, some researchers believe that the increased risk may be due to certain factors such as the use of fertility drugs and the manipulation of embryos during the ART procedures. Fertility drugs used during ART can stimulate the ovaries to produce more eggs, which can lead, as a consequence, to multiple pregnancies and an increased risk of IUGR. In addition, the manipulation of embryos during ART, such as the use of ICSI, may also raise the possibility of IUGR. Further research is needed to completely comprehend the exact process of this association and to identify strategies to minimize the risk of IUGR in pregnancies conceived using ART. Couples considering ART should discuss the potential risks and benefits of the procedure with their healthcare providers [23,24].
Coarctation of the aorta was found in 27,2% of cases in our study group. According to literature, the incidence of aortic coarctation represents 5-8-10% of CHD (congenital heart diseases) with a male predominance (2/1). It is estimated that 60-80% of the newborns with isolated coarctation of the aorta are discharged as healthy, later developing hemodynamic complications, installed suddenly or gradually with the closure of the arterial duct. For this reason, it is essential to perform cardiology screening on all newborns prior to discharge, which includes measuring arterial pressure in each of the four limbs and pre- and post-ductal pulse oximetry [25-31]. The patients with coarctation of the aorta from our study were transferred to the cardiovascular surgery service for specialized treatment. Survival is better among patients who undergo successful corrective treatment at a young age [26, 32]. Isolated coarctation of the aorta can be attributed to multifactorial inheritance, but a few families in which the transmission is autosomal dominant have been reported; in such families, the recurrence risk is 50% [28, 32]. Clinical studies suggest that genetic and environmental factors play an important role during pregnancy in the occurrence of this defect [26]. A 2018 study published in the Journal of the American College of Cardiology found that children born through ARTs had a higher risk of CHD compared to children naturally conceived [5, 33].
The family health history, especially the maternal one, together with certain pathological elements during pregnancy, suspicion of congenital heart disease on fetal echocardiography, inadequate fetal development, and/or problems at birth or postnatally, represent additional risk factors for congenital heart anomalies, and these newborns require postnatal evaluation[29].
None of the studied neonates from our IVF lot presented with diagnosed genetic syndromes or malformations. It could be explained by the fact that these pregnancies are more investigated than the general population. Lately, the number of newborns with genetic and multiple malformations syndromes has decreased due to better access to Family Doctors, Obstetricians, Geneticists, Pediatric Cardiologists (fetal echocardiography), and maternal-fetal medicine (morphology in the first and second trimester) especially in the case of pregnancies obtained through ART. Pediatric Cardiology has developed a lot in our country during recent years, increasing the number of available places for this specialty in the residency exam [26].
The incidence of symptomatic PDA is as high as 70% in infants with a birth weight <1000g. Infants with a symptomatic PDA have a higher risk of Bronchopulmonary Dysplasia (BPD), but early closure does not decrease this risk [17]. Our reported case with ELBW and PDA presented BPD as a complication of multiple causes (extreme prematurity, infection, PDA, mechanical ventilation). He required surgical ligation of PDA by an Italian-Romanian cardiovascular surgery team, which took place in our maternity unit, thus avoiding the stress of transfer. Initially, the neonatologist tried to close the arterial duct with medication, without a favorable response. There are still many open questions in the therapy of premature babies with PDA, which makes therapeutic approaches differ between centers. Some units approach a gradual therapy, which starts with a conservative treatment, followed, in the case of a hemodynamically significant ductus arteriosus (DA), by medical/surgical therapeutic interventions to close the DA. This approach seems to have most supporters. Some studies in the literature show that both therapeutic extremes - the least aggressive and the excessively aggressive ones - have lower therapeutic results and more important side effects. Other centers prefer early targeted drug therapy in premature babies with hemodynamically significant DA [26,34-36]. Although indomethacin and ibuprofen have been shown to be effective in producing ductal closure, the long-term benefits on the incidence and severity of BPD, necrotizing enterocolitis (NEC), or survival have yet to be established [29, 36-39]. Seventy percent of United States (US) Neonatologists believe that enteral feedings should be stopped in the presence of a PDA. In contrast, non-US Neonatologists have exactly the opposite opinion: 70% believe that enteral feedings should continue in the presence of a PDA [29,40]. The premature baby in our group had an upward weight curve. Growth was not affected despite the restriction of fluids recommended in the treatment of PDA, but enteral nutrition was maintained, initially trophic feedings with slowly increase of the amount of milk later on.
Good collaboration between Neonatologists and Pediatric Cardiologists, together with a thorough clinical examination, resulted in a reduction of morbidity and mortality due to CHD in our maternity unit.
Eight (72,7%) of the 11 newborns had an Apgar score >8, in spite of the fact that 72,7% of them were born preterm and had IUGR, which meant an increased risk of moderate to severe perinatal hypoxia. The frequency of perinatal asphyxia is inversely related to gestational age and birth weight; a higher incidence is observed in newborns with intrauterine growth restriction [16]. In our study, the vast majority of neonates had an Apgar score above 8, which indicates good obstetrical and neonatal management. Fetal distress and severe perinatal hypoxemia, which maintain high levels of pulmonary vascular resistance, lead to a longer persistence of transient systolic murmur of tricuspid regurgitation. This represents an innocent murmur that disappears after 1-2 days but may persist if there is a much-increased pulmonary vascular resistance[28,41].
In recent years, the frozen embryo transfer (FET) technique has gained popularity in assisted reproductive technology (ART) due to its various advantages over fresh embryo transfer (fresh-ET). One notable advantage of FET is a lower incidence of prematurity and being born small for gestational age (SGA), which are often associated with adverse health outcomes [42].
Our study has several limitations that should be considered when interpreting the results. We lacked data on the total number of embryos used in each embryo transfer, day of the embryos, type of assisted reproductive technology used. These limitations may affect the generalizability of our findings and warrant further investigation for future studies.
Due to good collaboration between Obstetricians, Neonatologists, and Pediatric Cardiologists, fetuses conceived using IVF received better management. All patients included in this study were born in our clinic (none of them was transferred), which shows a better understanding of the special monitoring needed for these pregnancies in our hospital.
Conclusions
In our study, the risk of CHD was significantly increased in the ART group compared to the spontaneous conception group. Further research is needed to fully understand the exact underlying mechanisms associating assisted reproductive technologies (ARTs) and congenital heart disease (CHD) and to identify strategies to minimize the risk of congenital cardiac malformations in children born through ART. Couples considering ART need to discuss the potential risks and benefits of the procedure with their healthcare providers.
ART pregnancies must be monitored in a 3rd level maternity hospital due to their risk of developing fetal IUGR or other perinatal complications exemplified in our study. Even though these pregnancies should be very well investigated, only 27.2%, less than half, of the CHDs in our study were diagnosed antenatally. In current practice guidelines, there is no consensus stating if conception by ART methods is an indication for performing a fetal echocardiography.
Funding
No funding was received for this study.
Conflict of interest
The authors declare no conflict of interest.
References
- Zorrilla M, Yatsenko AN. The Genetics of Infertility: Current Status of the Field. Curr Genet Med Rep 1 (2013): 247-260.
- Galdini A, Fesslova VME, Gaeta G, et al. Prevalence of Congenital Heart Defects in Pregnancies Conceived by Assisted Reproductive Technology: A Cohort Study. J Clin Med 10 (2021): 5363.
- Carson SA, Kallen AN. Diagnosis and Management of Infertility: A ReviewJAMA 326 (2021): 65-76.
- Henriksen TB, B. D. Time to pregnancy and preterm delivery. Obstet Gynecol 89 (1997): 594–599.
- Basso O, B.D. Infertility and preterm delivery, birthweight, and Caesarean section: a study within the Danish National Birth Cohort. Hum Reprod, 18 (2003): 2478–2484.
- Sutcliffe AG, L.M. Outcome of assisted reproduction. Lancet 370 (2007): 351–359.
- Tocariu R, Stan D, Mitroi RF. Incidence of complications among in vitro fertilization pregnancies 16 (2023): 399-405
- Eskew AM, Jungheim ES. A History of Developments to Improve in vitroFertilization. Mo Med 114 (2017): 156-159.
- Nahman MR. Romanian IVF: a brief history through the 'lens' of labour, migration and global egg donation markets. Reprod Biomed Soc Online 2 (2016): 79-87.
- Guvernul României. Government Emergency Ordinance 121/221 [2021]. Available from: https://mfamilie.gov.ro/docs/20220623Proiect-stema-hgfiv-iunie2022.pdf
- Bouillon, C. K.-R. Risk of congenital heart disease in children conceived by assisted reproductive technologies. Journal of the American College of Cardiology 72 (2018): 1126-1127.
- Tararbit K, Houyel L, Bonnet D, et al. Risk of congenital heart defects associated with assisted reproductive technologies: apopulation-based evaluation. Eur Heart J 32 (2011): 500-508.
- Giorgione, V., et al. Congenital heart defects in IVF/ICSI pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol, 51 (2018): 33-42.
- He M, Sun X, Wang C, et al. Analysis of the risk of complications duringpregnancy in pregnant women with assisted reproductive technology: aretrospective study using registry linkage from 2013 to 2018 in Shanghai, China. BMC Pregnancy Childbirth 22 (2022): 526.
- Quinn, J.-A, Munoz, F.M, Gonik, B, et al. Preterm Birth: Case Definition & Guidelines for Data Collection, Analysis, and Presentation of Immunisation Safety Data. Vaccine 34 (2016): 6047-6056.
- Quaresima P, et al. How to do a fetal cardiac scan. Arch Gynecol Obstet 307 (2023): 1269-1276.
- Eichenwald E. c, Hansen R.A, Martin C.R, et al. Cloherty and Stark’s Manual of Neonatal Care 8 (2021): 791-792.
- Brodsky D, Chritou H: Current concepts in intrauterine growth restriction. J Intensive Care Med 19 (2004): 307-319.
- Doctor BA, O′Riordan HL, et al: Perinatal correlates and neonatal outcomes of small for gestational age infants born at term gestation. Am J Obstet Gynecol 185 (2001): 652-659.
- Brodsky, MA Ouellette "Primary Care of the Premature Infant", WS 410 P952, (2008): 77-81.
- Martinez A, Simmons R: Abnormalities of fetal growth. In Taeusch HW, Ballard RA, Gleason CA, et al., editors: Avery′s diseases of the newborn, ed 8. Philadelphia, Elsevier Saunders (2005).
- Middelburg KJ, H.M. The association between in vitro fertilization and intrauterine growth restriction: a systematic review and meta-analysis. Fertil Steril, 108 (2017): e130-e131.
- Griesinger, E.M. Ovarian stimulation for IVF has no quantitative association with birthweight: a registry study. Hum Reprod 23 (2008): 2549-2554.
- Suleena Kansal Kalra, S.J. Ovarian Stimulation and Low Birth Weight in Infants Conceived Through In Vitro Fertilization. Obstet Gynecol 118 (2011): 863-871.
- Noori, S, Seri, I. Chapter 1 - Principles of Developmental Cardiovascular Physiology and Pathophysiology. In Hemodynamics and Cardiology (Third Edition); Seri, I, Kluckow, M, Eds. Elsevier: Philadelphia (2019): 3-27.
- Nicolescu A. Cinteza, E. Esentialul În Cardiologia Pediatrica; Amaltea (2022): 321-329.
- Boia, M, Costescu, O.-C, Cioboata, D, et al. Congenital Heart Disease – a Public Health Problem. Rom. J. Pediatr 69 (2020): 221-225.
- Stamatin.; A-L Avasiloaie, Urgente Neonatale; Tehnopress (2018).
- Charles S, Kleinman, Istvan Seri, Hemodynamics and Cardiology: Neonatology Questions and Controversies (Second Edition); W.B. Saunders: Philadelphia, (2012): 277-284.
- Petrescu I, Dumitrescu A, Iordache G, et al. Aortic coarctation-difficulties of fetal diagnosis. Case report and literature review. Ginecologia.ro. 2 (2017).
- Rosca I, Turenschi A, Nicolescu A, et al. Endocrine Disorders in a Newborn with Heterozygous Galactosemia, Down Syndrome and Complex Cardiac Malformation: Case Report, Jurnal Medicina mdpi.com, 59 (2023): 856.
- Brown ML, Burkhart HM, Connolly HM, et al. Coarctation of the aorta: Lifelong surveillance is mandatory following surgical repair. Journal of the American College of Cardiology 62 (2013): 1020-1025.
- Beekman RH, Robinow M. Coarctation of the aorta inherited as an autosomal dominant trait. Am J Cardiol 56 (1985): 818-819.
- Krishnappa S, Shah PS, Jain A, et al. Predictors of Early Extubation after Patent Ductus Arteriosus Ligation among Infants Born Extremely Preterm Dependent on Mechanical Ventilation. J Pediatr 214 (2019): 222-226.
- Isayama T, Kusuda S, Reichman B, et al. Neonatal Intensive Care Unit-Level Patent Ductus Arteriosus Treatment Rates and Outcomes in Infants Born Extremly Preterm. J Pediatr (2020).
- Clyman RI, Chorne N. Patent ductus arteriosus: evidence for and against treatment. J Pediatr 150 (2007): 216-219.
- Cooke L, Steer P, Woodgate P. Indomethacin for asymptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev (2003): CD003745
- Knight DB. The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Semin Neonatal. 2001;6:63-73
- Rosca I, Preda AG, Constantin AT, et al. Case report: Tackling the complexities of an extremely premature newborn with intrauterine growth restriction and congenital metabolic disorders through a multidisciplinary approach, frontiersin.org, Frontiers in Pediatrics 11 (2023).
- Jhaveri N, Soll RF, Clyman RI. Feeding practices and patent ductus arteriosus ligationpreferences-are they related? Am J Perinatol 27 (2009): 667-674.
- Turiy, Y. Evaluation of a Newborn with a Murmur. J. Pediatr. Heal. care Off. Publ. Natl. Assoc. Nurse Assoc. Pract 27 (2013): 226-229.
- Roque M, Haahr T, Geber S, Esteves SC, Humaidan P.Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update 25 (2019): 2-14.
