Association between Probable Generalized Anxiety Disorder with The Planning or Acceptance of The Pregnancy From The Beginning in Women Undergoing Prenatal Care
Article Information
Álvaro Monterrosa-Castroa, Jairo Fernández-Barriosb, Geraldine Romero-Martínezc,
Shairine Romero-Martínezd
a Physician. Gynecology. Senior researcher. Associate Professor. Grupo de Investigación Salud de la Mujer. Facultad de Medicina. Universidad de Cartagena. Colombia.
b Physician. Grupo de Investigación Salud de la Mujer. Facultad de Medicina. Universidad de Cartagena. Colombia.
c Physician. Grupo de Investigación Salud de la Mujer. Facultad de Medicina. Universidad de Cartagena. Colombia.
d Physician. Grupo de Investigación Salud de la Mujer. Facultad de Medicina. Universidad de Cartagena. Colombia.
*Corresponding Author: Dr. Álvaro Monterrosa Castro, Physician, Gynecology, Senior researcher, Associate Professor. Grupo de Investigación Salud de la Mujer. Facultad de Medicina. Universidad de Cartagena. Colombia.
Received: 13 February 2023; Accepted: 16 February 2023; Published: 22 February 2023
Citation:
Monterrosa-Castro A, Fernández-Barrios J, Romero-Martínez G, Romero-Martínez S. Association between probable generalized anxiety disorder with the planning or acceptance of the pregnancy from the beginning in women undergoing prenatal care. Obstetrics and Gynecology Research. 6 (2023): 79-83.
Share at FacebookAbstract
Objective:
To identify the frequency of Probable Generalized Anxiety Disorder (PGAD) and estimate its association with pregnancy planning or with its acceptance from the beginning.
Methods:
Cross-sectional study. Pregnant women who attended prenatal consultation, >12 weeks of gestation and without acute morbidity were included. They were asked about pregnancy planning and acceptance from the beginning. They answered the Generalized Anxiety Disorder Questionnaire to identify PGAD. Anonymous and voluntary participation.
Results:
702 pregnant women were assessed. Age 28.0±5.7y, gestational age 24.5±10.3w. Preconception consultation 22.8%; planned pregnancy 58.7%, accepted from the beginning 94.3% and PGAD 21.3%. Unplanned pregnancy was more frequent in pregnant women with PGAD than among those without PGAD, 53.4% vs. 38.1% The same was true for the pregnancy not accepted from the beginning, 11.4% vs. 6.3% Pregnancy planned and accepted from the beginning, they were associated with PGAD. OR:0.34[CI95%:0.17-0.67] and OR:0.53[CI95%:0.36-0.77].
Discussion:
PGAD was identified in one fifth of the pregnant women. Pregnancy planned and accepted from the beginning, were associated with 66% and 47% lower chance of PGAD. Unplanned or unaccepted pregnancy from the beginning can have a negative impact on mental health. It is suggested to explore mental health and planning/acceptance of the pregnancy, during prenatal control.
Keywords
Pregnancy; Pregnancy Unplanned; Mental Health; Mental Health Associations; Anxiety; Mental Health Services
Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals Pregnancy Unplanned articles Pregnancy Unplanned Research articles Pregnancy Unplanned review articles Pregnancy Unplanned PubMed articles Pregnancy Unplanned PubMed Central articles Pregnancy Unplanned 2023 articles Pregnancy Unplanned 2024 articles Pregnancy Unplanned Scopus articles Pregnancy Unplanned impact factor journals Pregnancy Unplanned Scopus journals Pregnancy Unplanned PubMed journals Pregnancy Unplanned medical journals Pregnancy Unplanned free journals Pregnancy Unplanned best journals Pregnancy Unplanned top journals Pregnancy Unplanned free medical journals Pregnancy Unplanned famous journals Pregnancy Unplanned Google Scholar indexed journals Mental Health articles Mental Health Research articles Mental Health review articles Mental Health PubMed articles Mental Health PubMed Central articles Mental Health 2023 articles Mental Health 2024 articles Mental Health Scopus articles Mental Health impact factor journals Mental Health Scopus journals Mental Health PubMed journals Mental Health medical journals Mental Health free journals Mental Health best journals Mental Health top journals Mental Health free medical journals Mental Health famous journals Mental Health Google Scholar indexed journals Mental Health Association articles Mental Health Association Research articles Mental Health Association review articles Mental Health Association PubMed articles Mental Health Association PubMed Central articles Mental Health Association 2023 articles Mental Health Association 2024 articles Mental Health Association Scopus articles Mental Health Association impact factor journals Mental Health Association Scopus journals Mental Health Association PubMed journals Mental Health Association medical journals Mental Health Association free journals Mental Health Association best journals Mental Health Association top journals Mental Health Association free medical journals Mental Health Association famous journals Mental Health Association Google Scholar indexed journals Anxiety articles Anxiety Research articles Anxiety review articles Anxiety PubMed articles Anxiety PubMed Central articles Anxiety 2023 articles Anxiety 2024 articles Anxiety Scopus articles Anxiety impact factor journals Anxiety Scopus journals Anxiety PubMed journals Anxiety medical journals Anxiety free journals Anxiety best journals Anxiety top journals Anxiety free medical journals Anxiety famous journals Anxiety Google Scholar indexed journals Mental Health Services articles Mental Health Services Research articles Mental Health Services review articles Mental Health Services PubMed articles Mental Health Services PubMed Central articles Mental Health Services 2023 articles Mental Health Services 2024 articles Mental Health Services Scopus articles Mental Health Services impact factor journals Mental Health Services Scopus journals Mental Health Services PubMed journals Mental Health Services medical journals Mental Health Services free journals Mental Health Services best journals Mental Health Services top journals Mental Health Services free medical journals Mental Health Services famous journals Mental Health Services Google Scholar indexed journals hormonal changes articles hormonal changes Research articles hormonal changes review articles hormonal changes PubMed articles hormonal changes PubMed Central articles hormonal changes 2023 articles hormonal changes 2024 articles hormonal changes Scopus articles hormonal changes impact factor journals hormonal changes Scopus journals hormonal changes PubMed journals hormonal changes medical journals hormonal changes free journals hormonal changes best journals hormonal changes top journals hormonal changes free medical journals hormonal changes famous journals hormonal changes Google Scholar indexed journals metabolic changes articles metabolic changes Research articles metabolic changes review articles metabolic changes PubMed articles metabolic changes PubMed Central articles metabolic changes 2023 articles metabolic changes 2024 articles metabolic changes Scopus articles metabolic changes impact factor journals metabolic changes Scopus journals metabolic changes PubMed journals metabolic changes medical journals metabolic changes free journals metabolic changes best journals metabolic changes top journals metabolic changes free medical journals metabolic changes famous journals metabolic changes Google Scholar indexed journals adverse perinatal implications articles adverse perinatal implications Research articles adverse perinatal implications review articles adverse perinatal implications PubMed articles adverse perinatal implications PubMed Central articles adverse perinatal implications 2023 articles adverse perinatal implications 2024 articles adverse perinatal implications Scopus articles adverse perinatal implications impact factor journals adverse perinatal implications Scopus journals adverse perinatal implications PubMed journals adverse perinatal implications medical journals adverse perinatal implications free journals adverse perinatal implications best journals adverse perinatal implications top journals adverse perinatal implications free medical journals adverse perinatal implications famous journals adverse perinatal implications Google Scholar indexed journals gestational intentions articles gestational intentions Research articles gestational intentions review articles gestational intentions PubMed articles gestational intentions PubMed Central articles gestational intentions 2023 articles gestational intentions 2024 articles gestational intentions Scopus articles gestational intentions impact factor journals gestational intentions Scopus journals gestational intentions PubMed journals gestational intentions medical journals gestational intentions free journals gestational intentions best journals gestational intentions top journals gestational intentions free medical journals gestational intentions famous journals gestational intentions Google Scholar indexed journals
Article Details
INTRODUCTION
Pregnancy involves hormonal and metabolic changes that are articulated with social aspects and influence mental health. Prenatal assessment should be multidisciplinary and combine obstetric aspects with mental health evaluation. This offers an opportunity to provide coping tools and identify mothers with mental disorders, to prevent adverse perinatal implications, especially preterm delivery and low birth weight [1,2,3,4]. In addition, it allows the timely referral of pregnant women who require psychiatric consultation [2].
It is of recent interest to explore the association between pregnancy intentionality and mental health. Two gestational intentions have been proposed: planning of the pregnancy and acceptance of the pregnancy from the beginning. They are used: unwanted, untimely or accidental pregnancies, without establishing differences [5]. These situations may be the cause or consequence of inadequate mental health [4].
Among the mental health disorders are Generalized Anxiety Disorder (GAD), characterized by excessive and uncontrollable worry. It is a problem with a lifetime prevalence of 3.7%, frequent in high-income countries, in pregnancy and postpartum [3,6]. Buist et al [2] found a 9.5% prevalence of GAD at some point in pregnancy, highest in the first trimester, and associated with pre-pregnancy anxiety, low educational level, low social support, and a history of child abuse.
Although French National Perinatal Survey [4] indicated a relationship between poor psychological health or depressive symptoms, with the acceptance and planning of the pregnancy, the latter have been little addressed with GAD. The objective was to identify the frequency of Probable Generalized Anxiety Disorder (PGAD) and estimate its association with pregnancy planning or with its acceptance from the beginning, in pregnant women receiving prenatal care.
Methodology
Cross-sectional study endorsed by the University of Cartagena and approved by the ethics committee. The Helsinki Declaration and the Belmont Report were considered. The participants acted anonymously and voluntarily, after signing an informed consent form.
Participants
Pregnant women who attended in 2022 at >12 weeks of gestation were included. Those who did not wish to participate, those with literacy limitations, fetal malformation, multiple pregnancy, genital bleeding or cervical cerclage, reproductive treatment and those receiving medication other than prenatal vitamins were excluded. The participants were invited to fill out a form that asked: obstetric data, schooling, occupation, cohabitation and opinion on the programming and acceptance of the pregnancy from the beginning. In addition, the Generalized Anxiety Disorder Questionnaire (GAD-7) was used to identify PGAD. Each question is answered: not at all (zero points), less than half of the days (one), more than half the days (two) almost every day (three). The optimal cutoff is 10 points, sensitivity 89.0%, specificity 82.0% and α Cronbach 0.92 [7]. In Spanish pregnant women α Cronbach 0.89 was estimated [8].
Sample size and statistical analysis
The sample size was calculated with the EPIDAT software. In the last decade, the selected clinic had attended 9600 prenatal/annual consultations. It was estimated to include 621 pregnant women, heterogeneity 50%, confidence level 95% and margin of error 5%. Ninety pregnant women were added to compensate for incorrectly completed forms. The analysis was performed with EPI-INFO-7. Quantitative data were expressed as X±DS and qualitative data as n (%). Differences for quantitative data were estimated with Anova or Mann-Whitney/Wilcoxon and qualitative data with Chi2. Two adjusted logistic regression models were performed. One, PGAD with acceptance of pregnancy from the beginning. The other, PGAD with pregnancy planning. The covariables were maternal age, residence, schooling, occupation, sexual partner, religiosity and obstetric history. p<0.05 was statistically significant.
Results
A total of 702 pregnant women were included in 2022, mean age 28 years. PGAD was found in 150 (21.3%). The sociodemographic and obstetric characteristics are presented in Table 1.
|
Sociodemographic and obstetric characteristics |
||||
|
|
All n = 702 |
Without PGAD n = 552 (78.6%) |
With PGAD n = 150 (21.4%) |
p |
|
Age, y, X±DS |
28.0±5.7 |
28.3±5.8 |
27.1±5.3 |
0.03? |
|
Age at first menstruation, y, X±DS |
12.5±1.7 |
12.6±1.7 |
12.3±1.8 |
0.21? |
|
Gestational age, w, X±DS |
24.5±10.3 |
24.4±10.4 |
24.7±10.4 |
0.73? |
|
First pregnancy, n, X±DS |
272 (38.7) |
216 (39.1) |
56 (37.3) |
0.69§ |
|
One or more vaginal deliveries, n, X±DS |
183 (26.0) |
138 (25.0) |
45 (30.0) |
0.22§ |
|
One or more cesarean sections, n, X±DS |
214 (30.5) |
171 (31.0) |
43 (28.7) |
0.58§ |
|
One or more miscarriages, n, X±DS |
169 (24.1) |
130 (23.6) |
39 (26.0) |
0.53§ |
|
One or more preterm deliveries, n, X±DS |
39 (5.6) |
30 (5.4) |
9 (6.0) |
0.79§ |
|
One or more stillbirths, n, X±DS |
14 (2.0) |
8 (1.4) |
6 (4.0) |
0.05§ |
|
Adolescent pregnant women, n (%) |
40 (5.7) |
29 (5.3) |
11 (7.3) |
0.33§ |
|
Preconception consultation, n (%) |
160 (22.8) |
131 (23.7) |
29 (19.3) |
0.26§ |
|
Pregnancy accepted from the beginning, n (%) |
662 (94.3) |
529 (95.8) |
133 (88.7) |
<0.001§ |
|
Planned pregnancy, n (%) |
412 (58.7) |
342 (62.0) |
70 (46.7) |
<0.001§ |
|
Residence in urban areas, n (%) |
651 (92.8) |
514 (93.1) |
137 (91.3) |
0.45§ |
|
Occupation outside the home, n (%) |
491 (70.0) |
389 (70.5) |
102 (68.0) |
0.55§ |
|
With stable sexual partner, n (%) |
654 (93.2) |
518 (93.8) |
136 (90.7) |
0.17§ |
|
Practicing any religion, n (%) |
654 (93.2) |
518 (93.8) |
136 (90.7) |
0.17§ |
|
Level of higher education, n (%) |
497 (70.8) |
400 (72.5) |
97 (64.7) |
0.06§ |
|
* Kruskal-Wallis H. ? ANOVA. § Chi2. |
||||
Table 1: Sociodemographic and obstetric characteristics
PGAD symptoms reported on “more than half of the days”, and “almost every day” were more frequent among pregnant women with PGAD (p<0.001). Figure 1.
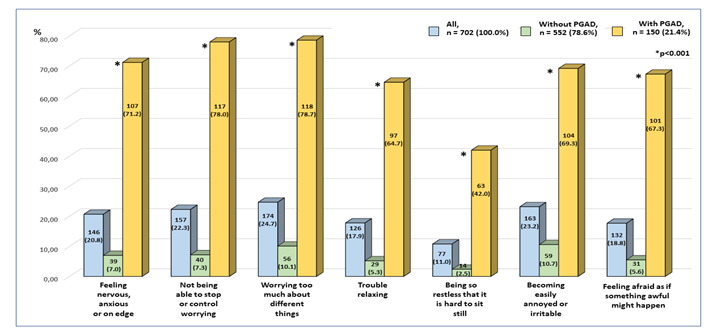
Figure 1: Items of the Generalized Anxiety Diseases Questionnaire [GAD-7]. Absolute and percentage frequency of the sum of the response options: “more than half the days” and “almost every day”. Distribution according to Probable Generalized Anxiety Disorder [PGAD].
Pregnancies were not accepted from the beginning by 5.7% of the pregnant women, more frequently among those with PGAD than among those without PGAD, 11.4% vs. 6.3%, respectively. Unplanned pregnancies were 41.4%, also more frequent in mothers with PGAD, 53.4% vs. 38.1%. Accepted pregnancy from the beginning and pregnancy planning were associated with lower chance of PGAD, OR:0.34[CI95%:0.17-0.67] and OR:0.53[CI95%:0.36-0.77], respectively (p<0.001).
Discussion
We found that one in five pregnant women had PGAD, which should be of concern, since mental health alterations in maternal have adverse perinatal, neonatal and infant effects [1,3]. Children born to women with PGAD during pregnancy have twice lower levels of BDNF (Brain Derived Fetal Circulating Neurotrophic Factor) in cord blood, which may negatively influence neurodevelopment [9].
We have estimated that the pregnancy accepted from its beginning and the planned pregnancy were associated with less PGAD. Women with an unplanned pregnancy had more psychiatric symptoms during the gestational period and one postnatal year, compared with women with a planned pregnancy [10]. Both results are consistent with other studies that indicate that unplanned or unaccepted pregnancies have deleterious effects on mental health during pregnancy, the puerperium, the postpartum years, and in women's adult life. Herd et al. [5] found an association between unwanted pregnancy ending in live birth with worse mental health outcomes for women later in life. They point out that mothers of unwanted youngsters were more likely to be depressed and unhappy than women whose children were the result of planned pregnancies. They recommend providing support to women who choose to continue with unplanned or unwanted pregnancies, due to the consequences for their mental health.
Education, socioeconomics, social support, accompaniment and well-being are factors that condition the decision to plan or accept the pregnancy, and even contribute to mental health. It is recommended to encourage preconception counseling, it was only completed by 22.7% of the pregnant women studied, and to explore mental health and provide tools to consolidate the ability to plan the pregnancy and accept it from the beginning. It is concluded that PGAD was identified in a fifth of those evaluated. The pregnancy accepted from the beginning and the planned pregnancy were associated with 66% and 47% lower chance of PGAD.
Acknowledgements
To the pregnant women who agreed to participate and filled out the forms anonymously and without receiving stipends. To Mrs. Mabel Vergara Borja, for the work of supervision and coordination of the field work. To the nursing and administrative staff of the Santa Cruz de Bocagrande Clinic, Cartagena, Colombia.
Ethics approval and consent to participate:
All experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki). The University of Cartagena endorsed this project, and the ethics committee of the Santa Cruz de Bocagrande Clinic, Cartagena, Colombia, approved it according to act 04-2018. The participants acted anonymously and voluntarily, without payment, and could leave the form incomplete if pertinent. Informed consent was obtained from all subjects and/or their legal guardian(s).
Disclosures
None to declared.
Funding
The Pregnancy Mental Study project [Mental Health in Pregnant Women with low obstetric risk who attend a prenatal control program], was the winner in the 2nd call for research projects of alliances with companies and the University of Cartagena, Colombia. It was advanced with logistical and financial support from the Research Vice-Rectory of the University of Cartagena and Clinica Santa Cruz de Bocagrande, Cartagena, Colombia. Resolution 01788-2020. The directors of the institutions did not participate in the design, field work, analysis and writing of the final reports, which were advanced by the authors.
Authors' contributions
M-C A (conceptualization, data curation, statistical analysis review, initial draft review, writing, revision and editing). F-B J, R-M G, R-M S (statistical analysis, writing original drafts, review and editing). All authors approved this manuscript.
Availability of data and materials
The data sets generated and/or analyzed during the study are available to interested persons, by request and by writing to the corresponding author.
REFERENCES
- Ghahremani T, Magann EF, Phillips A, Ray-Griffith SL, Coker JL, Stowe ZN. Women's Mental Health Services and Pregnancy: A Review. Obstet Gynecol Surv. 2022 Feb;77(2):122-129
- Buist A, Gotman N, Yonkers KA. Generalized anxiety disorder: course and risk factors in pregnancy. J Affect Disord. 2011 Jun;131(1-3):277-283.
- Inness BE, McCabe RE, Green SM. Problematic behaviours associated with generalized anxiety disorder during pregnancy and the postpartum period: A thematic analysis. Psychol Psychother. 2022 Dec;95(4):921-938.
- Moreau C, Bonnet C, Beuzelin M, Blondel B. Pregnancy planning and acceptance and maternal psychological distress during pregnancy: results from the National Perinatal Survey, France, 2016. BMC Pregnancy Childbirth. 2022 Feb 28;22(1):162.
- Herd P, Higgins J, Sicinski K, Merkurieva I. The Implications of Unintended Pregnancies for Mental Health in Later Life. Am J Public Health. 2016 Mar;106(3):421-429.
- Monterrosa-Blanco A, Cassiani-Miranda CA, Scoppetta O, Monterrosa-Castro A. Generalized anxiety disorder scale (GAD-7) has adequate psychometric properties in Colombian general practitioners during COVID-19 pandemic. Gen Hosp Psychiatry. 2021 May-Jun;70:147-148.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092-1097.
- García-Campayo J, Zamorano E, Ruiz MA, Pardo A, Pérez-Páramo M, López-Gómez V, Freire O, Rejas J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes. 2010 Jan 20;8:8.
- Uguz F, Sonmez EO, Sahingoz M, Gokmen Z, Basaran M, Gezginc K, Sonmez G, Kaya N, Erdem SS, Cicekler H, Tasyurek E. Maternal generalized anxiety disorder during pregnancy and fetal brain development: a comparative study on cord blood brain-derived neurotrophic factor levels. J Psychosom Res. 2013 Oct;75(4):346-350.
- Muskens L, Boekhorst MGBM, Kop WJ, van den Heuvel MI, Pop VJM, Beerthuizen A. La asociación del embarazo no planificado con la depresión perinatal: un estudio de cohorte longitudinal. Arch Womens Ment Health. 2022 Junio;25(3):611-620.
