Anxiety and Depressive Symptoms Developed During COVID-19 and Their Impact on the Academic Performance of Egyptian College Students
Article Information
Omar El Sayed Rageh1*, Meret Tawfik Awad Allah2, Mennatullah Mohammed Abd el Nasser Abozekry2, Dr. Salwa Hassan Atlam3
14th Year Medical Student, Faculty of Medicine, Tanta University, Tanta city, Gharbia governate, Egypt
25th Year Medical Student, Faculty of Medicine, Tanta University, Tanta city, Gharbia governate, Egypt
3Assistant Professor of Community Medicine and Public Health, Faculty of Medicine, Tanta University, Tanta city, Gharbia governate, Egypt
*Corresponding Author: Omar El Sayed Rageh, 4th Year Medical Student, Faculty of Medicine, Tanta University, Tanta city, Gharbia governate, Egypt
Received: 07 November 2022; Accepted: 16 November 2022; Published: 18 November 2022
Citation:
Rageh OES, Allah MTA, Abozekry MMAN, Atlam SH. Anxiety and Depressive Symptoms Developed During COVID-19 and Their Impact on the Academic Performance of Egyptian College Students. Journal of Psychiatry and Psychiatric Disorders 6 (2022): 268-275.
Share at FacebookAbstract
Introduction: The COVID-19 pandemic has increased levels of anxiety and depression among the public; however, the impact on the faculty of medicine students in Egypt with respect to academic achievement has not been well-documented.
Objective: Assessment of the prevalence of depression and anxiety among medical college students in Egypt during COVID-19 pandemic and impact thereof on their academic achievement.
Participants: 396 college students participated in this study and filled the questionnaire representing Egypt governates.
Methodology: An online survey was conducted via Google Forms addressing undergraduate students of all medical fields belonging to all Egyptian universities. A previously validated questionnaire sheet containing standardized scale for anxiety and depression, named Hospital Anxiety and Depression Scale (HADS) form is used in this study.
Results and Conclusion: Among the 396 participants, 28.5% experience symptoms of anxiety, and 35.6% are considered to have developed anxiety disorder. With respect to depressive symptoms, 21.2% are borderline and 38.1% experience actual depressive symptoms. However, there has been no significant association between these mental health issues and academic achievement. Families with sufficient savings and income as well as male students have fallen among the protective factors. High prevalence of depressive symptoms and anxiety among medical students during COVID 19 pandemic is alarming. Evidently, there is no significant impact on students’ academic performance; nevertheless, further studies are required to detect the long-term impact of this pandemic on student performance.
Keywords
Anxiety; Depression; COVID-19; Medical students; Mental health; Academic performance
Anxiety articles; Depression articles; COVID-19 articles; Medical students articles; Mental health articles; Academic performance articles
Anxiety articles Anxiety Research articles Anxiety review articles Anxiety PubMed articles Anxiety PubMed Central articles Anxiety 2023 articles Anxiety 2024 articles Anxiety Scopus articles Anxiety impact factor journals Anxiety Scopus journals Anxiety PubMed journals Anxiety medical journals Anxiety free journals Anxiety best journals Anxiety top journals Anxiety free medical journals Anxiety famous journals Anxiety Google Scholar indexed journals Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Medical student articles Medical student Research articles Medical student review articles Medical student PubMed articles Medical student PubMed Central articles Medical student 2023 articles Medical student 2024 articles Medical student Scopus articles Medical student impact factor journals Medical student Scopus journals Medical student PubMed journals Medical student medical journals Medical student free journals Medical student best journals Medical student top journals Medical student free medical journals Medical student famous journals Medical student Google Scholar indexed journals Mental health articles Mental health Research articles Mental health review articles Mental health PubMed articles Mental health PubMed Central articles Mental health 2023 articles Mental health 2024 articles Mental health Scopus articles Mental health impact factor journals Mental health Scopus journals Mental health PubMed journals Mental health medical journals Mental health free journals Mental health best journals Mental health top journals Mental health free medical journals Mental health famous journals Mental health Google Scholar indexed journals Academic performance articles Academic performance Research articles Academic performance review articles Academic performance PubMed articles Academic performance PubMed Central articles Academic performance 2023 articles Academic performance 2024 articles Academic performance Scopus articles Academic performance impact factor journals Academic performance Scopus journals Academic performance PubMed journals Academic performance medical journals Academic performance free journals Academic performance best journals Academic performance top journals Academic performance free medical journals Academic performance famous journals Academic performance Google Scholar indexed journals Hospital Anxiety and Depression Scale articles Hospital Anxiety and Depression Scale Research articles Hospital Anxiety and Depression Scale review articles Hospital Anxiety and Depression Scale PubMed articles Hospital Anxiety and Depression Scale PubMed Central articles Hospital Anxiety and Depression Scale 2023 articles Hospital Anxiety and Depression Scale 2024 articles Hospital Anxiety and Depression Scale Scopus articles Hospital Anxiety and Depression Scale impact factor journals Hospital Anxiety and Depression Scale Scopus journals Hospital Anxiety and Depression Scale PubMed journals Hospital Anxiety and Depression Scale medical journals Hospital Anxiety and Depression Scale free journals Hospital Anxiety and Depression Scale best journals Hospital Anxiety and Depression Scale top journals Hospital Anxiety and Depression Scale free medical journals Hospital Anxiety and Depression Scale famous journals Hospital Anxiety and Depression Scale Google Scholar indexed journals mental illness articles mental illness Research articles mental illness review articles mental illness PubMed articles mental illness PubMed Central articles mental illness 2023 articles mental illness 2024 articles mental illness Scopus articles mental illness impact factor journals mental illness Scopus journals mental illness PubMed journals mental illness medical journals mental illness free journals mental illness best journals mental illness top journals mental illness free medical journals mental illness famous journals mental illness Google Scholar indexed journals negative thoughts articles negative thoughts Research articles negative thoughts review articles negative thoughts PubMed articles negative thoughts PubMed Central articles negative thoughts 2023 articles negative thoughts 2024 articles negative thoughts Scopus articles negative thoughts impact factor journals negative thoughts Scopus journals negative thoughts PubMed journals negative thoughts medical journals negative thoughts free journals negative thoughts best journals negative thoughts top journals negative thoughts free medical journals negative thoughts famous journals negative thoughts Google Scholar indexed journals mental exhaustion articles mental exhaustion Research articles mental exhaustion review articles mental exhaustion PubMed articles mental exhaustion PubMed Central articles mental exhaustion 2023 articles mental exhaustion 2024 articles mental exhaustion Scopus articles mental exhaustion impact factor journals mental exhaustion Scopus journals mental exhaustion PubMed journals mental exhaustion medical journals mental exhaustion free journals mental exhaustion best journals mental exhaustion top journals mental exhaustion free medical journals mental exhaustion famous journals mental exhaustion Google Scholar indexed journalsArticle Details
1. Introduction
With The COVID-19 healthcare crisis has emerged in an unimaginable magnitude and momentum [1]. On 26 March 2020, over 3 billion people had been partially or completely locked down and had been required to comply with social distancing guidelines which led to deterioration of people’s mental stability [2]. Studies have also showed a noticeable prevalence of mental illness among health care workers dealing with COVID-19 [3].
Moreover, students’ lives and societies had been on lock down, erasing social and peer support networks that are considered protective of their mental health. Therefore, these students will face difficulties in moving on with their lives not to mention keeping up with the requirements of the healthcare degrees. Thus, a sizable number of students experience mental disorders, showing further symptoms of anxiety and / or depression [4].
Depressive disorders are illnesses that affect humans emotionally, physically and intellectually [5]. Even though a depressive mood might not be detectable, students may show signs of physical symptoms including without limitation fatigue, pain, and / or sleep disorder. A person diagnosed with chronic anxiety and / or depression is more likely to experience relapse [6].
Moreover, a study has shown that a sizable number of students experiences symptoms of anxiety and stress upon returning to clinics or schools. Generally, even in the absence of a public health crisis, medical college students show high prevalence of anxiety. A previous meta-analysis reported that the estimated global rate of anxiety among medical students is 28%, and another cross-sectional study indicated high prevalence of anxiety symptoms ranging between 31% and 46% [7].
In respect of depression, a study in Kuwait was conducted to assess mental illness status among healthcare professionals and undergraduate medical students. The study reported that 66.6% experience mild to severe signs of depression [8]. Another study conducted in Mexico among undergraduate and graduate students suggested that they have negative thoughts, mental exhaustion, and energy depletion [9]. Accordingly, this study aims to assess the prevalence of depression and anxiety during the COVID-19 pandemic and the impact thereof on academic performances of Egyptian college students.
2. Methodology
2.1 Study Design and Setting
It is a cross sectional, self-administered questionnaire-based study.
2.2 Study sample and participants
The least sample size needed for cross sectional studies using Epi info software with 95% confidence level and 5% confidence limits is 384. All undergraduate students from collages: Medicine, Dentistry, Pharmacy, Physical Therapy, Nursery, and Science might have participated in the study. An online Google form questionnaire was available from 25 Oct 2021 through 11 Nov 2021 and published among student social media groups in 12 of Egyptian governmental and private universities. Students from Tanta, Alexandria, Horus, Cairo, and Assuit Universities responded. 276 students completed the questionnaire. Moreover, a printed-out questionnaire was used for face-to-face interviewing with other students who did not participate online. The total number of participants amounted to 397. After exclusion of one incomplete questionnaire, the total number of participants was 396.
2.3 Exclusion criteria
Students diagnosed and taking treatments for any mental disorders are excluded from this study.
3. Study Tool to assess the Psychological Impact on the College Students and their Academic Performance
A validated questionnaire from a previous cross-sectional study that had been conducted in Jordan (HADS) as of July 2020 [10]. In addition, certain questions related to sociodemographic data had been validated by 5 experts in the field of Community Medicine and had been added at the beginning of the survey. Thus, the questionnaire consists of 3 main parts:
3.1 Part 1
The sociodemographic data of a participant (16 items) including: age, gender, University, college, academic year, father’s education and occupation, mother’s education and occupation, residence, family income, academic achievement last year (2020 – 2021) and the year before COVID – 19 (2019 – 2020), whether or not they had been infected, whether or not they had had the vaccine as well as the reason for not having the vaccine, and the sources of information.
3.2 Part 2
HADS scale for anxiety is composed of 7 questions which were answered as (always-often-sometimes-rarely) including: feeling tense or wound up, having panic attacks, anxiety, having stomach butterflies, and restlessness.
3.3 Part 3
HADS scale of Depressive signs is composed of 7 questions on whether he / she still enjoys things, can laugh and see the funny side, feels cheerful, slowed down, has lost interest in how they dress, looks forward to enjoyment and still enjoys a good book, radio, or TV program.
3.4 Scoring of the HADS scale
Scoring for each item of anxiety and depression ranges from zero to three. A subscale score of >8 denotes anxiety or depression. Scores From 0 to 7 means normal. Scores from 8 to10 specifies borderline cases and above 11 means being diagnosed with clinical anxiety or depression.
3.5 Statistical Analysis
Data was analyzed using IBM SPSS program, version 26. Qualitative data was reported in numbers and as a percentage. For comparison between variables, chi square test was used. Regression analysis was carried out to detect signs of anxiety and depression. The level of indication was chosen to be > 0.05.
4. Results
4.1 Demographic features
50.8% of the participants have over 21 years old. Females accounted for 67.7%. ~2 thirds (61.9%) live in urban areas. Most students (87,4%) study in governmental universities, and ~3 quarters (78%) of students study at the Faculty of Medicine. Approximately half of the participants (42.2%) are 5th year medical students. Students whose fathers received higher education and work in governmental institutions are found in 73.7% and 58.1% of the cases respectively. Therefore, 66.4% of students have highly educated mothers of whom 53.5% have paid jobs. There is sufficient family income in 47.2% of participants and sufficient saving in 45.5% of participants. The academic achievement before the COVID – 19 was excellent in 53.5% of the cases, very good in 29.8% of the cases, good in 14.6% of the cases, and bad in 2% of the cases. After the COVID – 19 year (2021), this achievement changed to excellent in 54.3% of the cases, very good in 26,3% of the cases, good in 14.1% of the cases, and bad in 5.3% of the cases. Nearly two thirds of students (62.4%) have not been diagnosed with COVID – 19, and the majorities (87.4%) are vaccinated Table (1).
|
Variable |
No (%) 396 |
|
Age (21.23 ± 1.664) |
|
|
Less than and equal to 21years |
195 (49.2) |
|
More than 21 years |
201 (50.8) |
|
Gender |
|
|
Males |
128 (32.3) |
|
Females |
268(67.7) |
|
University |
|
|
Governmental |
346 (87.4) |
|
Private |
50 (12.6) |
|
Faculties |
|
|
Biotechnology |
3 (8) |
|
Dentistry |
22 (5.6) |
|
Medicine |
311(78.5) |
|
Nursery |
1 (.3) |
|
Pharmacy |
33 (8.3) |
|
Physical Therapy |
13 (3.3) |
|
Science |
13 (3.3) |
|
Academic year |
|
|
1st year |
9 (2.3) |
|
2nd year |
101 (25.5) |
|
3rd year |
50 (12.6) |
|
4th year |
36 (9.1) |
|
5th year |
167 (42.2) |
|
6th year |
33 (8.3) |
|
Fathers' education |
|
|
High |
292 (73.7) |
|
Middle |
92 (23.2) |
|
Low |
12 (3.0) |
|
Fathers' occupation |
|
|
Governmental |
230 (58.1) |
|
Private |
166 (41.9) |
|
Mother's education |
|
|
High |
263 (66.4) |
|
Middle |
29 (7.3) |
|
Low |
104 (26.3 |
|
Mother's occupation |
|
|
Housewife |
184 (46.5) |
|
Paid job |
212 (53.5) |
|
Residence |
|
|
Urban |
245 (61.9) |
|
Rural |
151 (38.1) |
|
Family income |
|
|
Enough and saving |
180 (45.5) |
|
Enough |
187 (47.2) |
|
Not enough |
29 (7.3) |
|
Academic achievement before COVID19 |
|
|
Excellent |
212 (53.5) |
|
Very good |
118 (29.8) |
|
Good |
58 (14.6) |
|
Bad |
8 (2.0) |
|
Academic achievement After COVID19 |
|
|
Excellent |
215 (54.3) |
|
Very good |
104 (26.3) |
|
Good |
56 (14.1) |
|
Bad |
21 (5.3) |
|
Infected with COVID19 |
|
|
Yes |
149 (37.6) |
|
No |
247 (62.4) |
|
Vaccinated against COVID 19 |
|
|
Yes |
346 (87.4) |
|
No |
50 (12.6) |
Table 1: Characteristics of the study participants.
4.2 Prevalence of anxiety and depressive symptoms
Figure (1) showed that 35.8% are normal students with no anxiety symptoms, 28.5% experience signs of anxiety but are borderline, and 35.6% are diagnosed with anxiety disorder. Figure (2) shows that 40.7% are normal, 21.2% have borderline symptoms, and 38.1% show clear signs of depression.
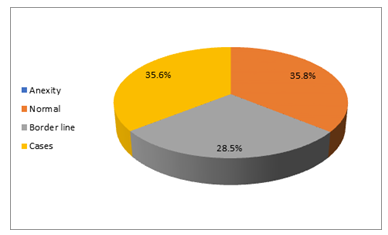
Figure 1: Prevalence of anxiety during COVID19 among study participants.
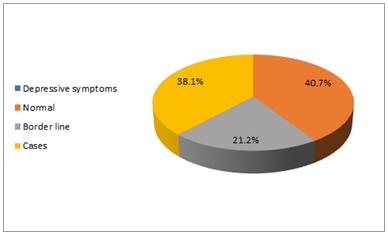
Figure 2: Prevalence of depressive symptoms during COVID19 among study participants.
4.3 Anxiety and depressive symptoms and students’ related determinants (psychological impact)
On the Scale of Anxiety: approximately 34.4% of participants aged 21 years old or less, experience borderline symptoms of anxiety compared to 40% who showed clear signs of anxiety disorder among those who are >21 years old. With respect to gender, females are the dominant part accounting for 29.1% with borderline symptoms, and 41.4% show clear signs of anxiety. The preclinical academic level had higher percentage of borderline symptoms (31.2%) compared to 40.3% of clinical academic level are diagnosed with anxiety. The academic performance of students with borderline symptoms was stable by 30.7% but jumped to 42.7% in students with clear signs. Individuals uninfected with COVID – 19 virus experience borderline symptoms by 30.4%. However, 40.3% of the infected students are diagnosed with anxiety. Approximately one third (30.3%) of students who are vaccinated have borderline symptoms and 36.4 % are diagnosed with anxiety.
On the Scale of Depression: the group aged 21 years old or less is dominant in borderline symptoms (24.1%) and actual depressive symptoms are found in 34.9%. Females have higher prevalence of borderline and actual symptoms accounting for 21.3% and 40.3% respectively. Paramedical faculties experience borderline symptoms by 23.1%, and 42.3% are diagnosed with depression. 23.8% of preclinical level students have borderline symptoms Compared to 39.4% clinical level students. Stable academic performance was reported by 23.6% of the borderline group and increased to 44% of the group diagnosed with depression. Nearly 22% of uninfected students had borderline symptoms, and 42.3% of infected students are diagnosed with depression. Approximately 22% of the unvaccinated had borderline symptoms, and 39% of the vaccinated are diagnosed with such disorder Table (2).
|
Anxiety |
Depressive symptoms |
|||||
|
Borderline No (%) 113 (28.5) |
Case No (%) 141 (35.6) |
X2 (P) |
Borderline No (%) 84 (21.2) |
Case No (%) 151 (38.1) |
X2 (P) |
|
|
Age groups |
||||||
|
≤21 years |
67 (34.4) |
59 (30.3) |
7.678 |
47 (24.1) |
68 (34.9) |
2.596 |
|
>21 years |
46 (22.9) |
82 (40.8%) |
(0.022)* |
37 (18.4) |
83 (41.3) |
-0.27 |
|
Gender |
||||||
|
Males |
35 (27.3) |
30 (23.4) |
15.315 |
27 (21.1) |
43 (33.6) |
2.031 |
|
Females |
78 (29.1) |
111 (41.4) |
(0.000)* |
57 (21.3) |
108 (40.3) |
-0.36 |
|
University |
||||||
|
Governmental |
89 (25.7) |
12 (35.3) |
15.315 |
71 (20.5) |
131 (37.9) |
1.295 |
|
Private |
24 (48.0) |
19 (38.0) |
(0.000)* |
13 (26.0) |
20 (40.0) |
-0.52 |
|
Faculties |
||||||
|
Medical |
104 (28.1) |
134 (36.2) |
1.002 |
78 (21.1) |
140 (37.8) |
0.423 |
|
Para-medical |
9 (34.6) |
7 (26.9) |
-0.606 |
6 (23.1) |
11 (42.3) |
-0.81 |
|
Academic level |
||||||
|
Preclinical |
50 (31.2) |
46 (28.8) |
5.522 |
38 (23.8) |
58 (36.2) |
1.093 |
|
Clinical |
63 (26.7) |
95 (40.3) |
-0.063 |
46 (19.5) |
93 (39.4) |
-0.58 |
|
Academic performance |
||||||
|
Increase |
24 (29.3) |
35 (42.7) |
6.33 |
17 (20.7) |
36 (43.9) |
|
|
Decrease |
24 (23.5) |
41 (40.2) |
-0.176 |
17 (16.7) |
43 (42.2) |
4.421 |
|
Stable |
65 (30.7) |
65 (30.7) |
50 (23.6) |
72 (34.0) |
-0.35 |
|
|
Infection with COVID19 |
||||||
|
Yes |
38 (25.5) |
60 (40.3) |
2.405 |
30 (20.1) |
63 (42.3) |
1.765 |
|
No |
75 (30.4) |
81 (32.8) |
-0.3 |
54 (21.9) |
88 (35.6) |
-0.41 |
|
Vaccination against COVID 19 |
||||||
|
Yes |
105 (30.3) |
126 (36.4) |
8.908 |
73 (21.1) |
135 (39.0) |
0.983 |
|
No |
8 (16.0) |
15 (30.0) |
(0.012)* |
11 (22.0) |
16 (32.0) |
-0.61 |
|
*Significant |
||||||
Table 2: Students' related determinants of anxiety and depressive symptoms during COVID 19 pandemics.
5. Anxiety and depressive Symptoms and Family Related Determinants (psychological impact)
5.1 On the scale of anxiety
Residents of rural areas have borderline symptoms by 33.8%, on the contrary 37.6% of the group living in urban areas have been diagnosed with anxiety. Students with fathers working for the private sector account for 32% of borderline symptom. However, 37% of participants’ fathers with governmental jobs are diagnosed with anxiety. Borderline symptoms are present in 32.1% of students whose mothers are housewives, however, 39.2% of students with mothers having paid jobs are diagnosed with such disorder. 29.4% of students with sufficient saving and family income have borderline symptoms; however, 51.7% of those with insufficient income are diagnosed with such disorder.
5.2 On the scale of depression
Rural areas residents had both borderline & cases by 23.8%, 40.4% respectively. In addition, 22.6% of borderline cases were found among those whose fathers had governmental jobs. But 39.2% of actual cases were found among those with fathers' private jobs. Also, 21.7% of borderline cases had mothers with paid jobs, and 40.2% of actual cases had housewives’ mothers. Not sufficient family income was reported by 31% of borderline cases and 55.2% of actual cases Table (3).
|
Anxiety |
Depressive symptoms |
|||||
|
Borderline No (%) 113(28.5) |
Case No (%) 141(35.6) |
X2 (P) |
Borderline No (%) 84(21.2) |
Case No (%) 151(38.1) |
X2 (P) |
|
|
Residence |
||||||
|
Urban |
62(25.3) |
92(37.6) |
3.326 |
48(19.6) |
90(36.7) |
2.562 |
|
Rural |
51(33.8) |
49(32.5) |
-0.19 |
36(23.8) |
61(40.4) |
-0.278 |
|
Fathers' education |
||||||
|
High |
86(29.5) |
102(34.9) |
3.645** |
55(18.8) |
108(37.0) |
7.827 |
|
Middle |
26(28.3) |
35(38.0) |
-0.449 |
27(29.3) |
37(40.2) |
-0.098 |
|
Low |
1(8.3) |
4(33.3) |
2(16.7) |
6(50.0) |
||
|
Fathers' occupation |
||||||
|
Governmental |
60(26.1) |
85(37.0) |
1.618 |
52(22.6) |
86(37.4) |
0.641 |
|
Private |
53(31.9) |
56(33.7) |
-0.449 |
32(19.3) |
65(39.2) |
-0.726 |
|
Mother's education |
||||||
|
High |
72(27.4) |
98(37.3) |
1.474 |
48(18.3) |
97(36.9) |
9.975 |
|
Middle |
32(30.8) |
35(33.7) |
-0.834 |
6(20.7) |
12(41.4) |
-0.092 |
|
Low |
9(31.0) |
8(27.6) |
30(28.8) |
42(40.4) |
||
|
Mother's occupation |
||||||
|
Housewife |
59(32.1) |
58(31.5) |
3.14 |
38(20.7) |
74(40.2) |
0.64 |
|
Paid job |
54(25.5) |
83(39.2) |
-0.206 |
46(21.7) |
77(36.3) |
-0.726 |
|
Family income |
||||||
|
Enough and saving |
53(29.4) |
52(28.9) |
36(20.0) |
54(30.0) |
||
|
Enough |
54(28.9) |
74(39.6) |
9.123 |
39(20.9) |
81(43.3) |
18.187 |
|
Not enough |
6(20.7) |
15(51.7) |
-0.057 |
9(31.0) |
16(55.2) |
(0.001) * |
|
**Fishers Exact test *significant |
||||||
Table 3: Home (family) related determinants of anxiety and depressive symptoms during COVID 19 pandemics among participants.
5.3 Determinants of anxiety and depression among students during COVID 19 pandemic (psychological impact)
Students at governmental universities have a greater chance of protection against borderline anxiety symptoms (Odds ratio=0.285). Males also have a much higher chance of protection against actual anxiety disorder compared to females (odds ratio= 0 .271).
Regarding depressive symptoms, those with sufficient income have a much greater chance of protection against the borderline symptoms compared to those with insufficient saving and family income (odds ratio=0.256 and 0.171 respectively). Those with actual depressive symptoms have a much greater chance of protection against depression among students with their family income was sufficient (odds ratio=0.298) and those with their family income sufficient and saving (odds ratio=0.153) (Table 4).
Table 4: Multivariate analysis of determinants of anxiety and depression among students during COVID 19 pandemic.
6. Discussion
Over the years, anxiety and depression constitute a major public health issue that is addressed among different groups of people. COVID – 19 has emerged and affected all people. Medical field students are expected to show greater suffering from anxiety and depressive symptoms due to lockdown and online learning [4].
According to this study, it is found that there has been a significant association between lower family income and the severity of anxiety scores. This finding is in line with the study conducted in Jorden and China [10,11]. In addition, both sufficient saving and family income are found to be significantly protective against actual depressive symptoms (odds ratio=0.298 and 0.153 respectively). However, sufficient family income shows a significantly higher chance of protection against the borderline condition compared to insufficient saving and family income (odds ratio=0.256 and 0.171 respectively). However, both had higher protection compared to families with lower income. This finding proves that financial stability of families during global pandemics can greatly affect the metal state of family members. During COVID-19 pandemic, there was spreading fear of the need to be hospitalized in severe infections which will cost a lot. Students who knew that their family financial state was sufficient and saving had been protected against anxiety or depression during COVID-19.
The study reported that most students in the Jorden (54%) have negative experience toward the learning process during COVID-19 quarantine period. However, approximately (68%) students show positive impact on their academic performance which was proven by their higher GPA [10]. This is explained in the study by higher probability of students to receive help in answering their exams due to deficiency of proper invigilation [12]. In this study, (42.7%) of anxiety cases and (44%) of depression cases have showed greater academic performance. This can be explained by the same improper invigilation of students during the exam time. In addition, the more stressed and anxious students are due to uncertainty during COVID-19, the more efforts they must put into studying and focusing on exams. Moreover, the lockdown and social distancing help students save time and spend this time in studying. However, this point might need an extra case control study to investigate the association between student stress and academic performance.
There were more anxiety cases among the females (41.4%) leading to a significant difference in the anxiety score (p=0.000). However, there is no significance regarding the gender in terms of the depression score (p=0.362). This is the same finding reported in the Turkish society [13] where females are identified as a risk factor for anxiety rather than depression [13]. Separately, a study performed in Central Region of Saudi Arabia [14] reported no significant correlations between students’ gender, faculty, academic year, and their anxiety score [14]. The increased prevalence of anxiety among females found in this study is linked to high-stress levels among women which can be explained by their hormonal changes. The same observation is noticed among college students. There is a significance in anxiety score (p=0.000) and no significance in the depression score (p=0.523). There is higher percentage in both borderline and cases of anxiety (48% and 38% respectively) in private universities students.
There is no significant correlation between medical and para-medical study fields and anxiety or depression (p= 0.606 and P= 0.809, respectively). This can be explained by the near similar availability of knowledge to all college students nowadays through social media and internet causing them all to be prone to anxiety and depression related to COVID-19 news. This was not the same result for studies performed during MERS-CoV Outbreak [15] who reported that during pandemic times, medical staff had a higher risk than para-medical stuff to suffer from loneliness, anxiety, fear, insomnia, and other mental health problems [15].
Most students aged over 21 years show higher susceptibility (40.8% anxiety cases and 41.3% depression cases). Being medical students, they are more exposed to deal with patients during the clinical rotations, so they are more prone to anxiety about risk of infection and depression symptoms.
The recent spread of the Severe Acute Respiratory Syndrome Coronavirus (COVID – 19) pandemic seems to be associated with psychiatric implications [16]. Preliminary data suggests that patients with COVID–19 might experience delirium, depression, anxiety, and insomnia [17]. This study has found that 40.3% of the infected participants are diagnosed with anxiety and 42.3% are diagnosed with depression. Another cross-sectional study conducted in Iran in 2021 among medical students to evaluate the degree of depression, anxiety, and stress levels indicated that most students there have 2 or 3 days of COVID infection, the anxiety score of participants is 28.56 ± 4.68 and the depression score is 28.99 ± 4.42. Findings also recorded extremely severe clinical depression while anxiety levels are only severe. Severe symptoms of anxiety & depression are estimated to be 99.04%, 69.57% respectively [18].
This study evaluated the vaccination effect on the mental health of the students and recorded 36.4% of the vaccine on the scale of anxiety. 39% of the vaccines are on the Scale of Depression. 22% of the unvaccinated had only borderline symptoms of depression. However, there is no significant association between infection or vaccination and anxiety or depression. A cross sectional study was performed in 2021 among Japanese college students aged 21.4 years to investigate their psychological state and their willingness to be vaccinated. The unvaccinated group demonstrated anxiety associated with their will to receive vaccination. There was no difference in anxiety & depressive mood among the unvaccinated & the vaccinated group [19]. This discrepancy between this study’s findings may be because willingness to get vaccinated could change over time [20,21] and the timing to collect responses was different as they conducted this survey from July to September 2021 at the beginning of the vaccination when anxiety and depression from vaccination couldn’t be determined.
7. Limitations
This study is a cross sectional study. Therefore, more types of studies with a higher level of substantiation should be conducted on this issue to prove the association between the COVID–19 pandemic and anxiety and depression and cohort studies should be conducted to evaluate anxiety and depression.
8. Conclusion and Recommendations
In Conclusion, there is high prevalence of anxiety and depression among the medical college students during COVID 19 pandemic. In addition, certain protective factors are sufficient saving and family income, and are present among males. There are no significant changes regarding academic performance during the pandemic period. Further studies need to be conducted to assess the long-term effect of the Pandemic on the mental health and academic performance of students.
References
- Gupta P, Anupama BK, Ramakrishna K. Prevalence of Depression and Anxiety among Medical Students and House Staff during the COVID-19 Health-Care Crisis. Academic Psychiatry: the Journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry 45 (2021): 575-580.
- Farooq F, Rathore FA, Mansoor SN. Challenges of Online Medical Education in Pakistan during COVID-19 Pandemic. Journal of the College of Physicians and Surgeons-Pakistan: JCPSP 30 (2020): 67-69.
- Lai J, Ma S, Wang Y, et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA network open 3 (2020): e203976.
- Smith CA. Covid-19: Healthcare Students Face Unique Mental Health Challenges. BMJ (Clinical research ed.) 369 (2020): m2491.
- Khan MS, Mahmood S, Badshah A, et al. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. JPMA. The Journal of the Pakistan Medical Association 56 (2006): 583-586.
- Rakel RE. Depression. Primary care 26 (1999): 211-224.
- Fernandez M, Vieira IS, Silva N, et al. Anxiety symptoms and alcohol abuse during the COVID-19 pandemic: A cross-sectional study with Brazilian dental undergraduate students. Journal of dental education, 85 (2021): 1739-1748.
- Alsairafi Z, Naser AY, Alsaleh FM, et al. Mental Health Status of Healthcare Professionals and Students of Health Sciences Faculties in Kuwait during the COVID-19 Pandemic. International journal of environmental research and public health 18 (2021): 2203.
- Camacho-Zuñiga C, Pego L, Escamilla J, et al. The impact of the COVID-19 pandemic on students' feelings at high school, undergraduate, and postgraduate levels. Heliyon 7 (2021): e06465.
- Basheti IA, Mhaidat QN, Mhaidat HN. Prevalence of anxiety and depression during COVID-19 pandemic among healthcare students in Jordan and its effect on their learning process: A national survey. PloS one 16 (2021): e0249716.
- Liang L, Ren H, Cao R, et al. The Effect of COVID-19 on Youth Mental Health. The Psychiatric quarterly 91 (2020): 841-852.
- Watson GR, Sottile J. Cheating in the digital age: Do students cheat more in online courses? Online Journal of Distance Learning Administration (2010).
- Özdin S, Bayrak Özdin S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. The International journal of social psychiatry 66 (2020): 504-511.
- Mohsin SF, Agwan MA, Shaikh S, et al. COVID-19: Fear and anxiety among healthcare workers in Saudi Arabia. A cross-sectional study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing 58 (2021).
- Khalid I, Khalid TJ, Qabajah MR, et al. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies During a MERS-CoV Outbreak. Clinical medicine and research 14 (2016): 7-14.
- Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, behavior, and immunity 87 (2020): 34-39.
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. The lancet. Psychiatry 7 (2020): 611-627.
- Moayed MS, Vahedian-Azimi A, Mirmomeni G, et al.. Coronavirus (COVID-19)-Associated Psychological Distress among Medical Students in Iran. Advances in experimental medicine and biology 1321 (2021): 245-251.
- Tsutsumi S, Maeda N, Tashiro T, et al. Willingness to Receive the COVID-19 Vaccination and the Psychological State of Japanese University Students: A Cross-Sectional Study. International journal of environmental research and public health 19 (2022): 1654.
- Szilagyi PG, Thomas K, Shah MD, et al. National Trends in the US Public's Likelihood of Getting a COVID-19 Vaccine-April 1 to December 8, 2020. JAMA 325 (2020): 396-398.
- MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 33 (2015): 4161-4164.
