An Unusual Presentation of Rectal Injury Following Radical Prostatectomy
Article Information
Sara Mohammed Jinnaah MBBS*, Ankur Sidhu MBBS, FRACS, Neil Strugnell MBBS, FRACS
Northern Health, Epping, Victoria, Australia
*Corresponding Author: Sara Mohammed Jinnaah, Northern Health, Epping, Victoria, Australia
Received: 20 February 2020; Accepted: 02 March 2020; Published: 06 March 2020
Citation: Sara Mohammed Jinnaah, Ankur Sidhu, Neil Strugnell. An Unusual Presentation of Rectal Injury Following Radical Prostatectomy. Journal of Radiology and Clinical Imaging 3 (2020): 043-047.
Share at FacebookKeywords
Rectal; Rectal injury, Extraperitoneal space
Rectal; Rectal injury articles, Extraperitoneal space articles
Extraperitoneal space articles Extraperitoneal space Research articles Extraperitoneal space review articles Extraperitoneal space PubMed articles Extraperitoneal space PubMed Central articles Extraperitoneal space 2023 articles Extraperitoneal space 2024 articles Extraperitoneal space Scopus articles Extraperitoneal space impact factor journals Extraperitoneal space Scopus journals Extraperitoneal space PubMed journals Extraperitoneal space medical journals Extraperitoneal space free journals Extraperitoneal space best journals Extraperitoneal space top journals Extraperitoneal space free medical journals Extraperitoneal space famous journals Extraperitoneal space Google Scholar indexed journals Rectal injury articles Rectal injury Research articles Rectal injury review articles Rectal injury PubMed articles Rectal injury PubMed Central articles Rectal injury 2023 articles Rectal injury 2024 articles Rectal injury Scopus articles Rectal injury impact factor journals Rectal injury Scopus journals Rectal injury PubMed journals Rectal injury medical journals Rectal injury free journals Rectal injury best journals Rectal injury top journals Rectal injury free medical journals Rectal injury famous journals Rectal injury Google Scholar indexed journals Rectal articles Rectal Research articles Rectal review articles Rectal PubMed articles Rectal PubMed Central articles Rectal 2023 articles Rectal 2024 articles Rectal Scopus articles Rectal impact factor journals Rectal Scopus journals Rectal PubMed journals Rectal medical journals Rectal free journals Rectal best journals Rectal top journals Rectal free medical journals Rectal famous journals Rectal Google Scholar indexed journals Radical Prostatectomy articles Radical Prostatectomy Research articles Radical Prostatectomy review articles Radical Prostatectomy PubMed articles Radical Prostatectomy PubMed Central articles Radical Prostatectomy 2023 articles Radical Prostatectomy 2024 articles Radical Prostatectomy Scopus articles Radical Prostatectomy impact factor journals Radical Prostatectomy Scopus journals Radical Prostatectomy PubMed journals Radical Prostatectomy medical journals Radical Prostatectomy free journals Radical Prostatectomy best journals Radical Prostatectomy top journals Radical Prostatectomy free medical journals Radical Prostatectomy famous journals Radical Prostatectomy Google Scholar indexed journals laparoscopic articles laparoscopic Research articles laparoscopic review articles laparoscopic PubMed articles laparoscopic PubMed Central articles laparoscopic 2023 articles laparoscopic 2024 articles laparoscopic Scopus articles laparoscopic impact factor journals laparoscopic Scopus journals laparoscopic PubMed journals laparoscopic medical journals laparoscopic free journals laparoscopic best journals laparoscopic top journals laparoscopic free medical journals laparoscopic famous journals laparoscopic Google Scholar indexed journals type 2 diabetes articles type 2 diabetes Research articles type 2 diabetes review articles type 2 diabetes PubMed articles type 2 diabetes PubMed Central articles type 2 diabetes 2023 articles type 2 diabetes 2024 articles type 2 diabetes Scopus articles type 2 diabetes impact factor journals type 2 diabetes Scopus journals type 2 diabetes PubMed journals type 2 diabetes medical journals type 2 diabetes free journals type 2 diabetes best journals type 2 diabetes top journals type 2 diabetes free medical journals type 2 diabetes famous journals type 2 diabetes Google Scholar indexed journals urinalysis articles urinalysis Research articles urinalysis review articles urinalysis PubMed articles urinalysis PubMed Central articles urinalysis 2023 articles urinalysis 2024 articles urinalysis Scopus articles urinalysis impact factor journals urinalysis Scopus journals urinalysis PubMed journals urinalysis medical journals urinalysis free journals urinalysis best journals urinalysis top journals urinalysis free medical journals urinalysis famous journals urinalysis Google Scholar indexed journals leukocytes articles leukocytes Research articles leukocytes review articles leukocytes PubMed articles leukocytes PubMed Central articles leukocytes 2023 articles leukocytes 2024 articles leukocytes Scopus articles leukocytes impact factor journals leukocytes Scopus journals leukocytes PubMed journals leukocytes medical journals leukocytes free journals leukocytes best journals leukocytes top journals leukocytes free medical journals leukocytes famous journals leukocytes Google Scholar indexed journals nitrites. articles nitrites. Research articles nitrites. review articles nitrites. PubMed articles nitrites. PubMed Central articles nitrites. 2023 articles nitrites. 2024 articles nitrites. Scopus articles nitrites. impact factor journals nitrites. Scopus journals nitrites. PubMed journals nitrites. medical journals nitrites. free journals nitrites. best journals nitrites. top journals nitrites. free medical journals nitrites. famous journals nitrites. Google Scholar indexed journals hollow visceral injury articles hollow visceral injury Research articles hollow visceral injury review articles hollow visceral injury PubMed articles hollow visceral injury PubMed Central articles hollow visceral injury 2023 articles hollow visceral injury 2024 articles hollow visceral injury Scopus articles hollow visceral injury impact factor journals hollow visceral injury Scopus journals hollow visceral injury PubMed journals hollow visceral injury medical journals hollow visceral injury free journals hollow visceral injury best journals hollow visceral injury top journals hollow visceral injury free medical journals hollow visceral injury famous journals hollow visceral injury Google Scholar indexed journals
Article Details
1. Case Report
We present a case of a sixty-seven-year-old male with past history of hypertension, hyperlipidemia and type 2 diabetes mellitus, who underwent laparoscopic radical prostatectomy for Gleason 3+4=7 prostate cancer. An intra-operative air leak test was performed which was negative. He had an uncomplicated hospital stay and was discharged day three post-operatively. The patient re-presented on the fifth post-operative day with worsening abdominal pain, temperature of 38.9 degrees and foul smelling, faeculent discharge from the umbilical abdominal extra-peritoneal port site wound. His indwelling urinary catheter was producing clear urine with negative urinalysis for leukocytes and nitrites.
The patient initially underwent a computed tomography with intravenous contrast which demonstrated surgical emphysema and a small amount of free fluid and free gas in the retroperitoneal plane. This was inconclusive in distinguishing between expected post-laparoscopic surgical status from hollow visceral injury (Image 1, Video 1). As the patient did not improve the following morning, he underwent a further computed tomography of the abdomen and pelvis with water soluble rectal contrast without intravenous contrast. This scan showed extensive extravasation of contrast and gas into the extraperitoneal space from a defect in the distal anterior rectal wall (Image 2, 3, Video 2). The patient was taken back to theatre for laparoscopic diversion by means of sigmoid loop colostomy. Extensive faecal contamination of the extraperitoneal space was treated by open irrigation and drain placement.
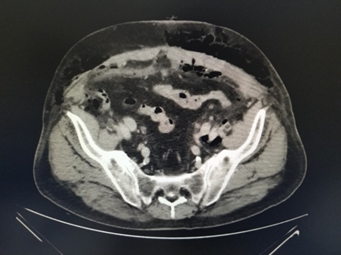
Image 1: CT without rectal contrast showing small volume free fluid and free gas in the extraperitoneal and subcutaneous planes.
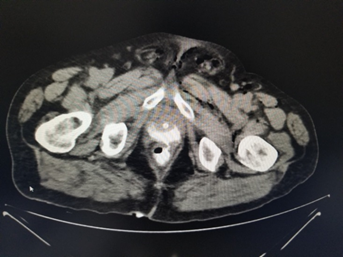
Image 2: CT with rectal contrast demonstrating location of rectal injury.
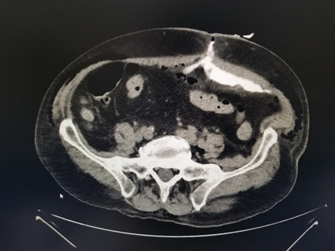
Image 3: CT with rectal contrast showing extravasation of contrast into the retroperitoneal plane and out of the skin wound.
Rectal injury is a rare and serious complication of radical prostatectomy [1, 2], the incidence of which is 0.5% [1]. It is more commonly seen in open rather than laparoscopic radical prostatectomy. Factors associated with a lower risk of rectal injury include robotic assisted laparoscopic radical prostatectomy, high volume center and obesity (owing to increased perirectal adipose tissue potentially acting as a barrier to injury) [3]. The probability of rectal injury during prostatectomy may be influenced by previous TRUS (Transrectal ultrasound) guided biopsies which may result in rectoprostatic adhesions. It is plausible that perineal biopsies may reduce this risk.
Rectal injuries may be identified intraoperatively when the anterior rectal wall is examined by laparoscopic visualisation and or with concurrent digital rectal exam. Air insufflation leak testing, as was done in this case, may also exclude or confirm the presence of rectal injury. In situations where the injury is unrecognized intraoperatively or where a later ischaemic or thermal injury occurs, patients present with signs of an atypical acute abdomen, fever and tachycardia [3]. Our patient, in addition to having those signs, also had the unusual finding of faeculant discharge from the umbilical port site.
In these situations an abdominal computerized tomography along with prompt surgical exploration is recommended [3]. As barium enema is contraindicated when rectal injury is suspected, the addition of water-soluble contrast enema in the above case helped to better identify the rectal injury as well as its location and severity. A review of the literature does show that the use of rectal contrast does improve detection of rectal injury [4]. Identifying the exact anatomical location of injury and differentiating between extraperitoneal and intraperitoneal involvement may help to guide operative approach and management [5].
2. Conclusion
The use of water soluble iodinated rectal contrast during abdominal computed tomography, in patients with suspected rectal injury following radical prostatectomy, allows for better visualization and management of these injuries.
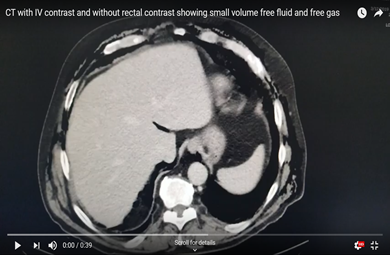
Video 1: CT with IV contrast and without rectal contrast showing small volume free fluid and free gas in the extraperitoneal plane.
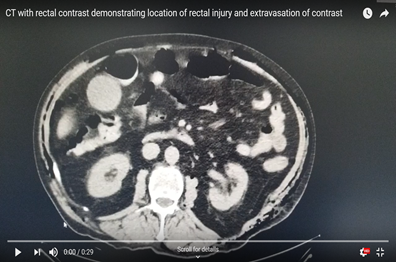
Video 2: CT with rectal contrast demonstrating location of rectal injury and extravasation of contrast in the the retroperitoneal plane and out of the skin wound via the extraperitoneal space.
References
- Mandel P, Linnemannstons A, Chun F, et al. Incidence, Risk Factors, Management, and Complications of Rectal Injuries During Radical Prostatectomy. European urology focus. Netherlands 4 (2018): 554-557.
- Redondo C, Rozet F, Velilla G, et al. Complications of radical prostatectomy. Arch Esp Urol 70 (2017): 766-776.
- Canda AE, Tilki D, Mottrie A. Rectal Injury During Radical Prostatectomy: Focus on Robotic Surgery. European urology oncology. Netherlands 1 (2018): 507-509.
- Tonolini M. Images in medicine: Diagnosis and pre-surgical triage of transanal rectal injury using multidetector CT with water-soluble contrast enema. J Emerg Trauma Shock 6 (2013): 213-215.
- Weinberg JA, Fabian TC, Magnotti LJ, et al. Penetrating rectal trauma: management by anatomic distinction improves outcome. J Trauma 60 (2006): 508-514.
