An Unusual Case of Mucinous Cystic Neoplasms of the Pancreas at Pregnancy
Article Information
Misgav Rottenstreich1*, Reut Rotem1, Menahem Ben-Haim2, Sorina Grisaru-Granovsky1, Orna Reichman A1, Hen Y Sela1
1Department of Obstetrics and Gynecology, Shaare Zedek Medical Center, Hebrew University Medical School, Jerusalem, Israel
2Department of General Surgery, Shaare Zedek Medical Center, Hebrew University Medical School, Jerusalem, Israel
*Corresponding author: Misgav Rottenstreich, Department of Obstetrics and Gynecology, Shaare Zedek Medical Center, Hebrew University Medical School, 12 Bayit Street, Jerusalem, Israel
Received: 28 August 2020; Accepted: 04 September 2020; Published: 19 September 2020
Citation:
Misgav Rottenstreich, Reut Rotem, Menahem Ben-Haim, Sorina Grisaru-Granovsky, Orna Reichman A, Hen Y Sela. An Unusual Case of Mucinous Cystic Neoplasms of the Pancreas at Pregnancy. Journal of Women’s Health and Development 3 (2020): 398-401.
Share at FacebookAbstract
A mucinous cystic neoplasm (MCNs) of the pancreas is an uncommon tumor that occurs mostly in females and are potentially sex hormone-sensitive. However, a MCN occurring during pregnancy is quite rare. A 25-year-old woman in the 35 week of gestation was referred to us because of a left flank pain. After unsuccessful treatment for pyelonephritis, a MRI revealed a large intra-abdominal cystic lesion. The patient subsequently underwent cesarean delivery and latter had tumor resection with distal pancreatectomy and splenectomy. Histopathological revealed a pancreatic MCN with low grade dysplasia. Our case strongly indicates the importance of further evaluation for uncommon causes for left flank pain.
Keywords
Mucinous cystic neoplasm, Pancreatic tumor, Pregnancy
Mucinous cystic neoplasm articles Mucinous cystic neoplasm Research articles Mucinous cystic neoplasm review articles Mucinous cystic neoplasm PubMed articles Mucinous cystic neoplasm PubMed Central articles Mucinous cystic neoplasm 2023 articles Mucinous cystic neoplasm 2024 articles Mucinous cystic neoplasm Scopus articles Mucinous cystic neoplasm impact factor journals Mucinous cystic neoplasm Scopus journals Mucinous cystic neoplasm PubMed journals Mucinous cystic neoplasm medical journals Mucinous cystic neoplasm free journals Mucinous cystic neoplasm best journals Mucinous cystic neoplasm top journals Mucinous cystic neoplasm free medical journals Mucinous cystic neoplasm famous journals Mucinous cystic neoplasm Google Scholar indexed journals Pancreatic tumor articles Pancreatic tumor Research articles Pancreatic tumor review articles Pancreatic tumor PubMed articles Pancreatic tumor PubMed Central articles Pancreatic tumor 2023 articles Pancreatic tumor 2024 articles Pancreatic tumor Scopus articles Pancreatic tumor impact factor journals Pancreatic tumor Scopus journals Pancreatic tumor PubMed journals Pancreatic tumor medical journals Pancreatic tumor free journals Pancreatic tumor best journals Pancreatic tumor top journals Pancreatic tumor free medical journals Pancreatic tumor famous journals Pancreatic tumor Google Scholar indexed journals Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals pancreas articles pancreas Research articles pancreas review articles pancreas PubMed articles pancreas PubMed Central articles pancreas 2023 articles pancreas 2024 articles pancreas Scopus articles pancreas impact factor journals pancreas Scopus journals pancreas PubMed journals pancreas medical journals pancreas free journals pancreas best journals pancreas top journals pancreas free medical journals pancreas famous journals pancreas Google Scholar indexed journals tumors articles tumors Research articles tumors review articles tumors PubMed articles tumors PubMed Central articles tumors 2023 articles tumors 2024 articles tumors Scopus articles tumors impact factor journals tumors Scopus journals tumors PubMed journals tumors medical journals tumors free journals tumors best journals tumors top journals tumors free medical journals tumors famous journals tumors Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals demonstrated splenomegaly articles demonstrated splenomegaly Research articles demonstrated splenomegaly review articles demonstrated splenomegaly PubMed articles demonstrated splenomegaly PubMed Central articles demonstrated splenomegaly 2023 articles demonstrated splenomegaly 2024 articles demonstrated splenomegaly Scopus articles demonstrated splenomegaly impact factor journals demonstrated splenomegaly Scopus journals demonstrated splenomegaly PubMed journals demonstrated splenomegaly medical journals demonstrated splenomegaly free journals demonstrated splenomegaly best journals demonstrated splenomegaly top journals demonstrated splenomegaly free medical journals demonstrated splenomegaly famous journals demonstrated splenomegaly Google Scholar indexed journals papillary tumor articles papillary tumor Research articles papillary tumor review articles papillary tumor PubMed articles papillary tumor PubMed Central articles papillary tumor 2023 articles papillary tumor 2024 articles papillary tumor Scopus articles papillary tumor impact factor journals papillary tumor Scopus journals papillary tumor PubMed journals papillary tumor medical journals papillary tumor free journals papillary tumor best journals papillary tumor top journals papillary tumor free medical journals papillary tumor famous journals papillary tumor Google Scholar indexed journals Hydatid cyst articles Hydatid cyst Research articles Hydatid cyst review articles Hydatid cyst PubMed articles Hydatid cyst PubMed Central articles Hydatid cyst 2023 articles Hydatid cyst 2024 articles Hydatid cyst Scopus articles Hydatid cyst impact factor journals Hydatid cyst Scopus journals Hydatid cyst PubMed journals Hydatid cyst medical journals Hydatid cyst free journals Hydatid cyst best journals Hydatid cyst top journals Hydatid cyst free medical journals Hydatid cyst famous journals Hydatid cyst Google Scholar indexed journals emphasizes articles emphasizes Research articles emphasizes review articles emphasizes PubMed articles emphasizes PubMed Central articles emphasizes 2023 articles emphasizes 2024 articles emphasizes Scopus articles emphasizes impact factor journals emphasizes Scopus journals emphasizes PubMed journals emphasizes medical journals emphasizes free journals emphasizes best journals emphasizes top journals emphasizes free medical journals emphasizes famous journals emphasizes Google Scholar indexed journals
Article Details
1. Short Reports and Comments
Mucinous cystic neoplasms (MCNs) of the pancreas is an uncommon tumor characterized by a proliferation of mucin-producing columnar epithelium, comprise about 23% of all cystic neoplasms[1]. Most pancreatic cystic neoplasms are detected incidentally when abdominal imaging is performed for other indication [2]. MCNs are usually slow-growing tumors, almost exclusively occur in women and are female-hormone dependent, thus pregnancy may increase their size [3, 4]. The incidence of invasive carcinoma (adenocarcinoma) associated with MCN in pregnancy is 30% [5].
2. Case Report
A 25-year-old woman, G3P2, was referred to our center at 35 weeks of gestation due to left flank pain with no fever or urinary symptoms. Her past medical history was unremarkable. On her admission to our medical center, her vital signs were normal the abdomen was soft with normal uterine tonus and left flank tenderness, vaginal examination revealed unfavorable cervix. Her laboratory exams showed no leukocytosis or electrolyte abnormalities but her urine was with leukocyturias. Fetal heart rate monitoring and biophysical profile were normal with no signs of uterine activity. Abdominal ultrasound demonstrated normal urinary tract. Considering all the above and due to her impressive distress, she was admitted with the diagnosis of pyelonephritis for intravenous antibiotic treatment and pain relief medications. On the following days, due to insufficient clinical improvement and negative pre-treatment urine culture, the possibility of adrenal infarct or hemorrhage was raised and a magnetic resonance imaging was performed. The MRI demonstrated splenomegaly up to 16 cm with close 9*8.7 cm cyst in the distal pancreas with septations and suspected small cysts within it (Figure 1). The cyst was compressing the splenic vein almost completely and there were signs of thrombus in the splenic and the right portal veins and varicose in the upper left abdomen.
These findings were very suggestive of MCN. The differential diagnoses were solid pseudo-papillary tumor, Hydatid cyst and Echinococcal cyst. Tumor panel showed mildly elevated CA125 - 43.6 U/ml (upper limit - 35) and CA 15-3 – 38.1 U/ml (upper limit - 30). Echinococcus antibodies were negative. After an extensive multi-disciplinary discussion, in order to refrain from increase intra-abdominal pressure during labor and because of the malignant potential of the cyst and the potential excessive bleeding during combined cesarean delivery and splenic/pancreatic surgery, a separated cesarean delivery and open distal pancreatectomy and splenectomy were schedule three weeks apart (Figure 2). At 37th weeks of gestation, a 3080-gram male was delivered with normal Apgar scores. Both ovaries were of normal appearance and size. Post-delivery CT scan also supported the suspected diagnosis of MCN. Three weeks following the delivery an open distal pancreatectomy and splenectomy were performed the findings are described in Figure 2. The post-operative course was uneventful and the patient was discharged at the tenth postoperative day. The pathology confirmed a 6*8*9 cm MCN and low grade dysplasia, an ovarian like stromal was present. She is currently followed-up by the general surgery department at our center and is doing well without need of further treatment (1 year following the delivery).
The presence of ovarian like stromal emphasizes that pancreatic MCN is female-hormone dependent which may explain the occurrence of symptoms during the late pregnancy [5]. Our case underlines the fact that obstetricians should remain aware of the differential diagnosis of left flank pain. If no sign of renal cause is evident, further investigations including laboratory analysis and imaging should be performed to search for the underline uncommon etiology. This further highlights that a multidisciplinary approach including a maternal-fetal medicine specialist, hepatobiliary surgeon, hematologist and an anesthesiologist is of utmost importance in the management of these rare phenomena.
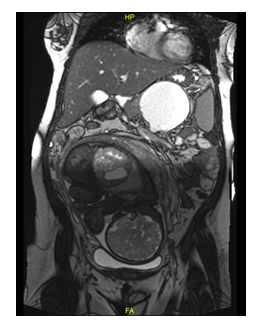
Figure 1: Magnetic Resonance Imaging (coronal view) show large cyst in the distal pancreas with suspected small cysts within it.
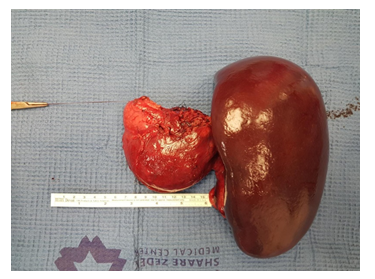
Figure 2: Intraoperative findings and macroscopic observations following distal pancreatectomy and splenectomy.
Acknowledgements
Patient consent form has been completed and signed by the patient.
Disclosure Statement
All authors have no conflict of interest or benefit that has arisen from the direct applications this research to disclose.
Funding
None of the authors have any direct or indirect financial incentive associated with publishing the article.
References
- Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, et al. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery 152 (2012): S4-S12.
- Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg 239 (2004): 651-659.
- Eloubeidi MA, Hawes RH. Mucinous tumors of the exocrine pancreas. Cancer Control 7 (2000): 445-451.
- Ikuta S, Aihara T, Yasui C, Iida H, Yanagi H, Mitsunobu M, et al. Large mucinous cystic neoplasm of the pancreas associated with pregnancy. World J Gastroenterol 14 (2008): 7252-7255.
- Kosumi K, Takamori H, Hashimoto D, Tanaka H, Abe S, Nakahara O, et al. Mucinous cystic neoplasm of the pancreas activated during pregnancy. Surg Case Reports 1 (2015): 13.
