An Innovative Technique for Anterior Cervical Surgery in Sub-axial Cervical Fracture Dislocation with incomplete spinal cord injury: A Paradigm Shift in Surgical Approach
Article Information
Shah Alam1*, Sharif Ahmed Jonayed2, Sarwar Jahan3, Abdullah Al Mamun Choudhury4, O Z M Dastagir5
1Professor and Chief Consultant, Department of Orthopaedics, Bangladesh Spine and Orthopaedic Hospital, Dhaka, Bangladesh
2Assistant Professor, Department of Orthopaedics, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
3Junior Consultant, Department of Orthopaedics, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
4Senior Consultant, Department of Orthopaedics, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
5Senior Consultant, Department of Orthopaedics, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
*Corresponding Author: Shah Alam, Professor and Chief Consultant, Department of Orthopaedics, Bangladesh Spine and Orthopaedic Hospital, Dhaka, Bangladesh
Received: 01 September 2023; Accepted: 11 September 2023; Published: 20 September 2023
Citation: Shah Alam, Sharif Ahmed Jonayed, Sarwar Jahan, Abdullah Al Mamun Choudhury, O Z M Dastagir. An Innovative Technique for Anterior Cervical Surgery in Sub-axial Cervical Fracture Dislocation with incomplete spinal cord injury: A Paradigm Shift in Surgical Approach. Journal of Orthopedics and Sports Medicine. 5 (2023): 375-380.
Share at FacebookAbstract
Introduction: Cervical spine injury was the most common cause of spinal cord injury worldwide in 2013, accounting for 43.9% to 61.5% of all cases. Prior to injury, the majority of individuals with a cervical spine injury was in their prime years and led an active lifestyle. The aim of the study was to evaluate the safety & efficacy of the proposed innovative technique to reduce all cases of subaxial cervical fracture-dislocation.
Methods: This was a retrospective study and was conducted in the Department of Orthopaedic Surgery during the period from January 2020 to June 2023. In our study, we included 336 patients with subaxial cervical fracture dislocation who underwent ACDF. We routinely used an anterior approach with a left-sided transverse incision for surgery.
Results: The mean age was 34.61 ± 12.37 years with a male predominance. The most common mechanism of injury was RTA (39.29%) and most common level of fracture at C5/C6 was 38.10%. Mean operative time was 70.2 + 19.1 mins, and mean blood loss 142.72 ± 82.27 ml. The mean NDI improved to 10.7 ± 6.8, VAS improved to 3.1 ± 1.4 at the final followup which showed majority of our patients could return to their daily life activities. Majority (83.04%) of our patients had no complications and dysphagia was 4.17 %. Majority of 236(70.24%) patients had no disability.
Conclusions: In our study, we found that a single anterior approach is a safe and effective procedure for subaxial cervical spine dislocation treatment with satisfactory radiological, neurological and functional outcomes.
Orthopaedics articles Orthopaedics Research articles Orthopaedics review articles Orthopaedics PubMed articles Orthopaedics PubMed Central articles Orthopaedics 2023 articles Orthopaedics 2024 articles Orthopaedics Scopus articles Orthopaedics impact factor journals Orthopaedics Scopus journals Orthopaedics PubMed journals Orthopaedics medical journals Orthopaedics free journals Orthopaedics best journals Orthopaedics top journals Orthopaedics free medical journals Orthopaedics famous journals Orthopaedics Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Spine articles Spine Research articles Spine review articles Spine PubMed articles Spine PubMed Central articles Spine 2023 articles Spine 2024 articles Spine Scopus articles Spine impact factor journals Spine Scopus journals Spine PubMed journals Spine medical journals Spine free journals Spine best journals Spine top journals Spine free medical journals Spine famous journals Spine Google Scholar indexed journals Cervical spine injury articles Cervical spine injury Research articles Cervical spine injury review articles Cervical spine injury PubMed articles Cervical spine injury PubMed Central articles Cervical spine injury 2023 articles Cervical spine injury 2024 articles Cervical spine injury Scopus articles Cervical spine injury impact factor journals Cervical spine injury Scopus journals Cervical spine injury PubMed journals Cervical spine injury medical journals Cervical spine injury free journals Cervical spine injury best journals Cervical spine injury top journals Cervical spine injury free medical journals Cervical spine injury famous journals Cervical spine injury Google Scholar indexed journals Disc herniation articles Disc herniation Research articles Disc herniation review articles Disc herniation PubMed articles Disc herniation PubMed Central articles Disc herniation 2023 articles Disc herniation 2024 articles Disc herniation Scopus articles Disc herniation impact factor journals Disc herniation Scopus journals Disc herniation PubMed journals Disc herniation medical journals Disc herniation free journals Disc herniation best journals Disc herniation top journals Disc herniation free medical journals Disc herniation famous journals Disc herniation Google Scholar indexed journals Vertebral body fractures articles Vertebral body fractures Research articles Vertebral body fractures review articles Vertebral body fractures PubMed articles Vertebral body fractures PubMed Central articles Vertebral body fractures 2023 articles Vertebral body fractures 2024 articles Vertebral body fractures Scopus articles Vertebral body fractures impact factor journals Vertebral body fractures Scopus journals Vertebral body fractures PubMed journals Vertebral body fractures medical journals Vertebral body fractures free journals Vertebral body fractures best journals Vertebral body fractures top journals Vertebral body fractures free medical journals Vertebral body fractures famous journals Vertebral body fractures Google Scholar indexed journals Bilateral facet injuries articles Bilateral facet injuries Research articles Bilateral facet injuries review articles Bilateral facet injuries PubMed articles Bilateral facet injuries PubMed Central articles Bilateral facet injuries 2023 articles Bilateral facet injuries 2024 articles Bilateral facet injuries Scopus articles Bilateral facet injuries impact factor journals Bilateral facet injuries Scopus journals Bilateral facet injuries PubMed journals Bilateral facet injuries medical journals Bilateral facet injuries free journals Bilateral facet injuries best journals Bilateral facet injuries top journals Bilateral facet injuries free medical journals Bilateral facet injuries famous journals Bilateral facet injuries Google Scholar indexed journals Spinal cord articles Spinal cord Research articles Spinal cord review articles Spinal cord PubMed articles Spinal cord PubMed Central articles Spinal cord 2023 articles Spinal cord 2024 articles Spinal cord Scopus articles Spinal cord impact factor journals Spinal cord Scopus journals Spinal cord PubMed journals Spinal cord medical journals Spinal cord free journals Spinal cord best journals Spinal cord top journals Spinal cord free medical journals Spinal cord famous journals Spinal cord Google Scholar indexed journals Blood loss articles Blood loss Research articles Blood loss review articles Blood loss PubMed articles Blood loss PubMed Central articles Blood loss 2023 articles Blood loss 2024 articles Blood loss Scopus articles Blood loss impact factor journals Blood loss Scopus journals Blood loss PubMed journals Blood loss medical journals Blood loss free journals Blood loss best journals Blood loss top journals Blood loss free medical journals Blood loss famous journals Blood loss Google Scholar indexed journals Cervical plate articles Cervical plate Research articles Cervical plate review articles Cervical plate PubMed articles Cervical plate PubMed Central articles Cervical plate 2023 articles Cervical plate 2024 articles Cervical plate Scopus articles Cervical plate impact factor journals Cervical plate Scopus journals Cervical plate PubMed journals Cervical plate medical journals Cervical plate free journals Cervical plate best journals Cervical plate top journals Cervical plate free medical journals Cervical plate famous journals Cervical plate Google Scholar indexed journals Bone graft articles Bone graft Research articles Bone graft review articles Bone graft PubMed articles Bone graft PubMed Central articles Bone graft 2023 articles Bone graft 2024 articles Bone graft Scopus articles Bone graft impact factor journals Bone graft Scopus journals Bone graft PubMed journals Bone graft medical journals Bone graft free journals Bone graft best journals Bone graft top journals Bone graft free medical journals Bone graft famous journals Bone graft Google Scholar indexed journals Sternocleidomastoid muscle articles Sternocleidomastoid muscle Research articles Sternocleidomastoid muscle review articles Sternocleidomastoid muscle PubMed articles Sternocleidomastoid muscle PubMed Central articles Sternocleidomastoid muscle 2023 articles Sternocleidomastoid muscle 2024 articles Sternocleidomastoid muscle Scopus articles Sternocleidomastoid muscle impact factor journals Sternocleidomastoid muscle Scopus journals Sternocleidomastoid muscle PubMed journals Sternocleidomastoid muscle medical journals Sternocleidomastoid muscle free journals Sternocleidomastoid muscle best journals Sternocleidomastoid muscle top journals Sternocleidomastoid muscle free medical journals Sternocleidomastoid muscle famous journals Sternocleidomastoid muscle Google Scholar indexed journals Strap muscles articles Strap muscles Research articles Strap muscles review articles Strap muscles PubMed articles Strap muscles PubMed Central articles Strap muscles 2023 articles Strap muscles 2024 articles Strap muscles Scopus articles Strap muscles impact factor journals Strap muscles Scopus journals Strap muscles PubMed journals Strap muscles medical journals Strap muscles free journals Strap muscles best journals Strap muscles top journals Strap muscles free medical journals Strap muscles famous journals Strap muscles Google Scholar indexed journals Osteophytes articles Osteophytes Research articles Osteophytes review articles Osteophytes PubMed articles Osteophytes PubMed Central articles Osteophytes 2023 articles Osteophytes 2024 articles Osteophytes Scopus articles Osteophytes impact factor journals Osteophytes Scopus journals Osteophytes PubMed journals Osteophytes medical journals Osteophytes free journals Osteophytes best journals Osteophytes top journals Osteophytes free medical journals Osteophytes famous journals Osteophytes Google Scholar indexed journals Body Mass Index articles Body Mass Index Research articles Body Mass Index review articles Body Mass Index PubMed articles Body Mass Index PubMed Central articles Body Mass Index 2023 articles Body Mass Index 2024 articles Body Mass Index Scopus articles Body Mass Index impact factor journals Body Mass Index Scopus journals Body Mass Index PubMed journals Body Mass Index medical journals Body Mass Index free journals Body Mass Index best journals Body Mass Index top journals Body Mass Index free medical journals Body Mass Index famous journals Body Mass Index Google Scholar indexed journals
Article Details
1. Introduction
A cervical spine injury is a dreadful event that can result in disabilities and even death if not handled properly. It occurs in 2-6% of all blunt trauma cases, with 55% having associated spinal cord injury and 10% to 25% deteriorating later [1]. The most prevalent causes are traffic accidents and falls. Age and male gender are risk factors for cervical injury, and instant death may occur in up to 20% of senior patients [2].
Cervical spine injury was the most common cause of spinal cord injury worldwide in 2013, accounting for 43.9% to 61.5% of all cases [3]. Prior to injury, the majority of individuals with a cervical spine injury was in their prime years and led an active lifestyle. Over the past ten years, the fundamental management strategies for cervical spine fractures and dislocations have hardly changed. The decision regarding which surgical approach to use for treating cervical facet dislocations varies and is dependent on several variables, including the patient's neurological condition, the presence of traumatic disc herniation, the success of closed reduction, the presence of uni- or bilateral facet dislocations, the presence of vertebral body fractures, and the experience and training of the surgeon [4,5]. Decompression of nerve tissues and stability of the damaged vertebral segment are the main goals of surgical management of injuries caused by trauma to the cervical spine.
This enables the patient to be treated for their injuries more quickly, accelerates rehabilitation, and makes it easier for them to resume their professional duties [6]. Anterior or posterior approach, a combination of both, or phased anterior/posterior/anterior approaches are the surgical technique options for unilateral or bilateral facet injuries [5]. Although cervical spine dislocation can be successfully treated with both anterior and posterior procedures, the anterior approach has gained popularity during the past ten years [7-11]. The anterior approach is generally low-risk and traumatic, with a low rate of complications that can be performed in a supine position.
A further advantage of the anterior approach is the removal of disc pieces that have entered the spinal canal. This approach allows treating just one motion section, which leads to fewer neck issues, and compared to the posterior approach, which requires more than one motion segment to be fused to achieve the same realignment. However, the posterior approach carries risks such as excessive dissection, postoperative pain, blood loss, and issues maintaining safe vital signs in the prone position [5,12-14]. In the meantime, due to subsequent disc degeneration with observed increasing instability, the affected segment develops kyphosis during short-level posterior fixation. Once more, fixation through a combination of approaches is quite difficult. The main drawbacks are a longer recovery period after surgery, more bleeding, slow wound healing, and difficulty in altering posture [15].
Considering all these factors, we have opted to manage all cases of cervical spine dislocation in a simplified manner by a single anterior approach; in this study, we aimed to evaluate the safety and efficacy of the proposed innovative technique to reduce all cases of subaxial cervical fracture-dislocation.
2. Methodology and Materials
This was a retrospective study and was conducted in the Department of Orthopaedic Surgery of National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka Medical College Hospital (DMCH), Bangladesh Spine and Orthopaedic Hospital (BSOH) Dhaka, Bangladesh during the period from January 2020 to June 2023. In our study, we took 336 cases with subaxial cervical fracture dislocation (either unilateral or bilateral) based on our inclusion and exclusion criteria.
These are the following criteria to be eligible for the enrollment as our study participants: a) Patients aged between 14-53 years; b)Patients with subaxial cervical fracture dislocation; c) Patients with fracture less than three weeks ; d) Patients who underwent anterior cervical discectomy and fusion (ACDF) using a tricortical bone graft & were stabilized by cervical plate & screws; e) Patients who were followed from 3 months to 24 months were included in the study And a) Patients with polytrauma, head injury, multiple fractures & open pathological fractures; b) Patients with ASIA A neurology were excluded from our study.
The patients signed informed written consent forms that detailed the operation and treatment options. The patients were initially resuscitated according to the advanced trauma life support (ATLS) protocol in the emergency department. After initial stabilization with a rigid cervical collar, a thorough history and examination (including information on the patient's gender, age, mechanism of injury, comorbidities, and occupation) were taken. The neurological problems that existed prior to surgery were categorized using the American Spinal Injury Association (ASIA) Impairment Scale. Plain cervical spine X-rays were acquired in each case. In certain situations, a computed tomography (CT) scan and magnetic resonance imaging (MRI) was done afterward. The patient had surgery on the following possible dates. Data such as the length of the procedure and any intraoperative complications were recorded. Patients were mobilized as soon as their conditions allowed, which was usually the following day. For the first three weeks, all patients wore a rigid cervical collar before moving to a gentle collar for the remaining three weeks. Patients were seen in the outpatient department (OPD) every two weeks for the first three months, then monthly for the next three months, and finally every six months. At each follow-up, the visual analog scale (VAS), Neck Disability Index (NDI), and ASIA grading were performed. X-rays and CT scans were performed to determine implant fixation and fusion [15].
2.1 Surgical Technique:
Patients who showed a fracture dislocation of sub axial cervical spine underwent ACDF. We routinely used an anterior approach with a left-sided transverse incision for surgery.
- Positioning, Draping & Marking.
- Incision & dissection from midline to lateral border of sternocleidomastoid muscle. The platysma muscle is incised along the line of skin incision, developing plane between sternocleidomastoid & strap muscles. Sternocleidomastoid and carotid sheath are retracted laterally and the trachea, esophagus, and strap retracted medially.
- Locate damaged disc, Removal of disc, free fragments & osteophytes. The cartilage endplates on the vertebral bones are also removed to reveal the hard cortical bone underneath. Curette all osteophytes & removal of uncovertebral joint in piecemeal by 1mm Kerrison rongeur.
- Casper screws were employed, and a discectomy was performed to achieve local kyphosis per-operatively.
- In the empty disc space, a small periosteal elevator was inserted into the lower vertebra's posterior border, leveraging the superior vertebra.
- Then gentle manipulation was done by applying backward and forward pressure to the caudal vertebrae by the periosteal elevator while the cephalad vertebral body was pushed back.
- Head end assistant: Gradual & longitudinal traction with axial rotation of head
- Leg end assistant: Stabilize by counter traction Leg end assistant
- Chief Surgeon: Reduce the dislocated vertebra by using special instrument like periosteum elevator.
- After the reduction, ACDF was performed.
2.2 Statistical Analysis:
All data were recorded systematically in preformed data collection form and quantitative data was expressed as mean and standard deviation and qualitative data was expressed as frequency distribution and percentage. Statistical analysis was performed by using SPSS 21 (Statistical Package for Social Sciences). Probability value <0.05 was considered as level of significance. The study was approved by Ethical Review Committee of Bangladesh Spine and Orthopaedic Hospital (BSOH), Dhaka, Bangladesh (Figure 1).
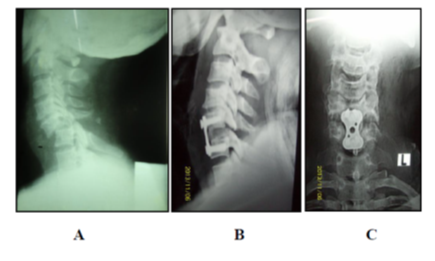
Figure 1: ACDF with anterior cervical plate & screw - A) Preoperative and B) & C) Postoperative
3. Results
Table 1 shows the baseline and clinical characteristics of our study patients. We found the mean age was 34.61 ± 12.37 5R$years. The most common mechanism of injury was RTA (39.29%), falls from height (37.50%), and followed by fall while carrying a heavy weight on the head (23.21%). The majority (63.69%) of our patients had bilateral dislocation while 36.31% had unilateral. The most common level of fracture at C5/C6 was 38.10%, followed by C6/C7 was 24.11%, C4/C5 and C3/C4 was 20.83% and 16.96% respectively.
Table 1: Baseline and Clinical Characteristics of study participants.
|
Baseline and Clinical characteristics |
N |
P(%) |
|
Mean age (in years) |
34.61 ± 12.37 |
|
|
Gender |
||
|
Male |
226 |
67.26 |
|
Female |
110 |
32.74 |
|
Mechanism of injury |
||
|
Fall from height |
126 |
37.5 |
|
Road traffic accident (RTA) |
132 |
39.29 |
|
Fall for carrying a heavy weight on the head |
78 |
23.21 |
|
Type of dislocation |
||
|
Bilateral |
214 |
63.69 |
|
Unilateral |
122 |
36.31 |
|
Level of fracture |
||
|
C3/C4 |
57 |
16.96 |
|
C4/C5 |
70 |
20.83 |
|
C5/C6 |
128 |
38.1 |
|
C6/C7 |
81 |
24.11 |
|
Clinical Characteristics |
||
|
Height (cm) |
163.5 ± 7.9 |
|
|
Weight (cm) |
67.06 ± 8.92 |
|
|
Body Mass Index (kg/m2) |
27.50 ± 6.8 |
|
|
Mean operative time(min) |
70.2 ± 19.1 |
|
|
Mean blood loss (ml) |
142.72 ± 82.27 |
|
Table 2: Comparison of functional and neurological outcomes after ACDF by NDI, VAS, and AIS score.
|
Functional outcome |
Pre-operative |
Post-operative |
P-value |
||
|
Neck Disability Index (NDI) |
18.7 ± 9.5 |
10.7 ± 6.8 |
<0.05 |
||
|
Visual Analog Score (VAS) |
7.1 ± 2.4 |
3.1 ± 1.4 |
<0.05 |
||
|
Neurological outcome |
|||||
|
ASIA B |
100 |
29.76 |
13 |
3.87 |
|
|
ASIA C |
144 |
42.86 |
30 |
8.93 |
|
|
ASIA D |
92 |
27.38 |
57 |
16.96 |
|
|
ASIA E |
0 |
0 |
236 |
70.24 |
|
|
a) ASIA = American Spinal Injury Association; b) AIS= ASIA Impairment Scale |
|||||
Table 2 shows that functional outcome was assessed using the NDI and the VAS. The mean preoperative NDI was 18.7 ± 9.5, which improved to 10.7 ± 6.8 at the final follow-up, and the mean pre-operative VAS 7.1 ± 2.4 was improved to 3.1 ± 1.4 at the final follow-up with a p-value of <0.05. According to the ASIA, out of 336 patients 100 (29.76%) patients had AISA B, 144 (42.86%) patients had ASIA C, and 92 (27.38%) patients had ASIA D neurology at the preoperative phase. Postoperatively, 13(3.87%) had ASIA B, 30(8.93%) had ASIA C, 57 (16.96%) had ASIA D and 236 (70.24%) had ASIA E neurology. In the current study, a two-grade and a one-grade improvement was noted in all our patients.
Table 3: Distribution of our study patients by complications
|
Complications |
N |
P(%) |
|
Dysphagia |
14 |
4.17 |
|
Inadequate reduction |
5 |
1.49 |
|
C5 palsy |
3 |
0.89 |
|
Excessive bleeding |
7 |
2.08 |
|
Recurrent laryngeal nerve palsy |
8 |
2.38 |
|
Screw broke |
3 |
0.89 |
|
Screw pullout |
4 |
1.19 |
|
Graft dislodgement |
6 |
1.79 |
|
Nonunion |
7 |
2.08 |
|
No complications |
279 |
83.04 |
Table 3 shows the majority (83.04%) of our patients had no complications, followed by 4.17% had dysphagia, less than 3% had recurrent laryngeal nerve palsy, excessive bleeding and nonunion, less than 2% had screw pullout, graft dislodgement, inadequate reduction and less than 1% had C5 palsy and broken screw.
Table 4: Functional result assessment by NDI scale.
|
Final outcome |
N |
P(%) |
|
No disability |
236 |
70.24 |
|
Mild disability |
57 |
16.96 |
|
Moderate disability |
30 |
8.93 |
|
Severe disability |
13 |
3.87 |
|
Complete disability |
0 |
0 |
Table 4 shows functional results assessed by NDI scale, 236(70.24%) patients had no disability, 57(16.96%) patients had mild disability, 30(8.93%) patients had moderate disability, and 13(3.87%) patients had severe disability.
4. Discussion
It is crucial to treat subaxial cervical fracture dislocations properly and promptly. The choice between surgical treatment and a reduction is still up for dispute. Each tactic has advantages and disadvantages. The optimal therapeutic approach for each patient should be chosen by the spine surgeon in order to provide positive outcomes. In this investigation, we decided to treat every case of Subaxial cervical fracture dislocation using the anterior-only method.
In our study majority of patients were 44-53 years old and mean age was 34.61 ± 12.37 years. A study done by Jonayed et al. [15] found the average age was 34.50±11.92 years (16-70 years) which was similar to our study. Abdelgawaad et al. [16] found the mean age 39.1 ± 13.8 years ranged from 17 to 60 years. Most of the patients in our series were adults as compared to Laus et al. [17] and Singhal et al. [18]. Majority (67%) of our patients were male. Jonayed et al. [15] and Abdelgawaad et al. [16] had male predominance with 90.62% and 90.5% respectively. Other studies also showed the majority of young male patients in their studies [17,18].
In the current study, the most common mechanism of injury was RTA (39.29%). Abdelgawaad et al. [16] and Laus et al. [17] also showed that the common cause of injury was RTA (55%) and (85%), respectively. On the other hand, Jonayed et al. [15] showed the most common mechanism of injury was a fall while carrying a heavy weight on the head (51.6%), followed by falls from height (29.7%).
The most common level of fracture was C5/C6 was 38.10%, followed by C6/C7 was 24.11%. Similar results were observed by Jonayed et al. [15], which were C5-C6 (57.7%), followed by C6-C7 (26.6%). Singhal et al. [18] found the most involved level of the spine was C5/C6 & C6/C7 which were 53.7% and 28.1% respectively. Laus et al. [17] found the involved vertebra was C5 in seven cases. Abdelgawaad et al. [16] found the most common injury level was at C4-5 (47.6%).
For reduction, we performed GardnerWells traction in all of our cases. None of our patients showed neurologic damage during reduction. In other studies, they had performed awake traction prior to MRI because obtaining an MRI could cause the reduction to be delayed. Sometimes it takes a longer time to do an MRI. So, it was recommended not to postpone reduction for MRI though cervical fracture-dislocation is frequently associated with disc disruption [15,19-21]. However, paralysis secondary to retropulsion fragments is rare. Although up to 22% of patients have been found to have significant disc herniation post-reduction, these do not correlate with neurologic deterioration [20].
In our study, the mean operative time was 70.2 ± 19.1 minutes and mean blood loss was 142.72 ± 82.27 ml. In other studies, the average operational time was 84.25±9.55 and 65.2 ± 15.1 minutes, with a mean blood loss of 112.12 ± 25.27 and 416.7 ± 82.7 ml [15,16]. The anterior method takes less time to perform than the posterior technique, with Kwon et al. [22] reporting a mean operative time of 103 minutes. Yukawa et al. [23] observed similar findings on the posterior route, with a mean operational time of 101 minutes and a mean blood loss of 190 ml. Obviously, the combined approach would take more time as well as would result in higher blood loss. This confirms that the anterior approach, which takes less operative time, is suitable for patients who cannot withstand a long time of anesthesia and for those with neurological impairment, as time is a critical factor for them [15,16]. However, our study shows that the anterior approach may lead to more intraoperative blood loss, compared to posterior approach.
The mean NDI improved to 10.7 ± 6.8, which showed that most of our patients had mild disability and no disability at all. The mean VAS improved to 3.1 ± 1.4 at the final follow-up which showed majority of our patients could return to their daily life activities. In one study, the mean VAS improved to 2.05 ± 0.98 at the last follow-up, which was statistically significant and similar to our study [15]. In 52 (81.3%) instances, their NDI scoring revealed minimal to no disability [15].
Among all patients, majority (42.86%) had ASIA C, followed by 29.76% had ASIA B, and 27.38% patients had ASIA D. Postoperatively, a two-grade and a one-grade improvement was noted in 59.82% and 36.31% patients respectively. In a study done by Jonayed et al., where two grade improvement was noted in 30 (46.9%) patients, followed by one-grade improvement in 26 (40. 63%) patients, and all patients with ASIA A showed no neurological recovery [15]. Mcafee et al. [24] observed a shift of ASIA grade 1 in 76% of cases and a change of ASIA grade 2 in 12% of cases. We observed only one case had a transient neuro-deficit that was recovered fully and improved neurologically at the final follow-up, as seen by Mcafee et al [24]. It indicates the safety of the single anterior approach.
In the present study, majority (83.04%) of our patients had no complications, followed by 4.17% had dysphagia, less than 3% had recurrent laryngeal nerve palsy, excessive bleeding & nonunion, less than 2% had screw pullout, graft dislodgement, inadequate reduction and less than 1% had C5 palsy & broken screw. A study found 2 (9.5%) patients deteriorated post operation by 1 or 2 grades of AIS; however, both of them improved during late follow-up and 2 (9.5%) patients developed radiculopathy, only 1 case lost reduction and 3 patients (14.3%) complained of persistent dysphagia at late follow-up [16]. Implant failure, graft dislodgement, hematoma, revision, and deformity are uncommon complications [23]. At two weeks, the most common problem was mild dysphagia in 15 (23.4%) patients [15]. In the first two weeks, the reported incidence was around 71% [20]. Donor site pain was found in five (7.8%) patients and dural injury in three (4.7%) patients [15]. Aronson et al. [25] also reported temporary dysphagia (4.7%) and temporary hoarseness (2.32%) in 100 patients; dura was injured in one (8.3%) patient, which is 11% in Brodke et al [26].
In terms of neurological outcome, there was no significant difference between anterior and posterior techniques compared to the literature data [21,22,27]. The study by Nakashima et al. [28] on posterior approach for cervical fracture-dislocations with traumatic disc herniation showed that 9 of 12 incomplete paralysis patients (75%) showed postoperative improvement by more than 1 grade in their AIS. Brodke et al. [26] also found no significant difference between methods, with 70% and 57% of individuals with poor neurology improving when treated anteriorly and posteriorly, respectively. This is the reason we chose the anterior-only approach to manage the subaxial CSD cases in our study.
5. Conclusions and Recommendations
In our study, after evaluating our patients by VAS, NDI and ASIA scale we found that a single anterior approach is a safe and effective procedure for subaxial cervical spine dislocation treatment with satisfactory radiological, neurological and functional outcomes. The surgical treatment of subaxial cervical traumatic injuries with anterior reduction, decompression, and fusion is effective in terms of fusion state and patient satisfaction. In comparison to the combined anterior and posterior approach, the anterior-only procedure appears to be less traumatic to patients and takes shorter time. Most subaxial cervical spine dislocations can be minimized using GardnerWells traction and successfully fixed with anterior surgery alone.
So, further study with a prospective and longitudinal study design including larger sample size needs to be done to identify more advantages of ACDF to relieve pain & prevent morbidity.
Limitations of the study
We could observe a few complications within our short study period. There are more advantages and disadvantages of performing surgery with single anterior approach on cervical spine dislocated patients’ that needs to be evaluated. There is more scoring scale like NDI was not assessed in our study. We evaluated our patients with a maximum 2 year follow up and have not known other possible interference that may happen in the long term with these patients.
Conflict of Interest:
None
References
- Hong R, Meenan M, Prince E, et al. Comparison of three prehospital cervical spine protocols for missed injuries. West J Emerg Med 15 (2014): 471-479.
- Harris MB, Reichmann WM, Bono CM, et al. Mortality in elderly patients after cervical spine fractures . J Bone Joint Surg Am 92 (2010): 567-574.
- Singh A, Tetreault L, Kalsi-Ryan, et al. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 6 (2014): 309-331.
- Elizabeth MY, Ahmad N. Management of cervical facet dislocations: anterior versus posterior approach, in Vaccaro AR, Eck JC (eds): Controversies in Spine Surgery: Best Evidence Recommendations. New York: Thieme Publishers (2010): 48-58
- Lee JY, Nassr A, Eck JC, et al. Controversies in the treatment of cervical spine dislocations. Spine J 9 (2009): 418-423.
- Defino HLA, Figueira FG, de Camargo LS, et al. Treatment of traumatic dislocations of the cervical spine through anterior approach. Acta Ortop Bras 15 (2007): 30-34.
- Pan HC, Huang CI, Chen MT, et al. Anterior cervical stabilization with the synthesis cervical spine locking plate system. Zhonghua Yi Xue Za Zhi (Taipei) 62 (1999): 852-858.
- Lifeso RM, Colucci MA. Anterior fusion for rotationally unstable cervical spine fractures. Spine (Phila Pa 1976) 25 (2000): 2028-2034.
- Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine (Phila Pa 1976) 23 (1998):181-6; discussion 186-7.
- Ebraheim NA, DeTroye RJ, Rupp RE, et al. Osteosynthesis of the cervical spine with an anterior plate. Orthopedics 18 (1995): 141-147.
- Ordonez BJ, Benzel EC, Naderi S, et al. Cervical facet dislocation: techniques for ventral reduction and stabilization. J Neurosurg 92 (2000): 18-23.
- Park HJ, Shim YJ. Treatment of distractive flexion injury in the lower cervical spine using anterior cervical fusion. J Korean Soc Spine Surg 14 (2007): 221-228.
- Jónsson H Jr, Cesarini K, Petrén-Mallmin M, et al. Locking screw-plate fixation of cervical spine fractures with and without ancillary posterior plating. Arch Orthop Trauma Surg 111 (1991): 1-12.
- Liu JK, Das K. Posterior fusion of the subaxial cervical spine: indications and techniques . Neurosurg Focus 10 (2001): E7.
- Jonayed S, Choudhury AAM, Alam MS, et al. Efficacy, Safety, and Reliability of the Single Anterior Approach for Subaxial Cervical Spine Dislocation. Cureus 15 (2023): e34787.
- Abdelgawaad AS, Metry ABS, Elnady B, et al. Anterior Cervical Reduction Decompression Fusion With Plating for Management of Traumatic Subaxial Cervical Spine Dislocations. Global Spine Journal 11 (2020): 312-320.
- Laus M, Pignatti G, Tigani D, et al. Anterior decompression and plate fixation in fracture-dislocations of the lower cervical spine. Eur Spine J 2 (1993): 82-88.
- Singhal B, Mohammed A, Samuel J, et al. Neurological outcome in surgically treated patients with incomplete closed traumatic cervical spinal cord injury. Spinal Cord 46 (2008): 603-607.
- Doran SE, Papadopoulos SM, Ducker TB, et al. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg 79 (1993): 341-345.
- Grant GA, Mirza SK, Chapman JR, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg 90 (1999): 13-18.
- Harrington JF, Likavec MJ, Smith AS. Disc herniation in cervical fracture subluxation . Neurosurgery 29 (1991): 374-379.
- Kwon BK, Fisher CG, Boyd MC, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine 7 (2007): 1-12.
- Yukawa Y, Kato F, Ito K, et al. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J 18 (2009): 1293-1299.
- McAfee PC, Bohlman HH, Ducker TB, et al. One-stage anterior cervical decompression and posterior stabilization. A study of one hundred patients with a minimum of two years of follow-up. J Bone Joint Surg Am 77 (1995): 1791-1800.
- Aronson N, Filtzer DL, Bagan M. Anterior cervical fusion by the smith-robinson approach . J Neurosurg 29 (1968): 396-404.
- Brodke DS, Anderson PA, Newell DW, et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech 16 (2003): 229-235.
- Bolton N: Surgical approaches for cervical spine facet dislocations in adults. Orthop Nurs 35 (2016): 266-267.
- Nakashima H, Yukawa Y, Ito K, et al. Posterior approach for cervical fracture-dislocations with traumatic disc herniation. Eur Spine J 20 (2011): 387-394.
