Adult Scheuermann Kyphosis Surgical Treatment by Single Posterior Approach
Article Information
Joana Pereira*, Ana Sofia Esteves, Pedro Ribeiro, José Miradouro, Helder Nogueira, Jorge Alves
Tâmega e Sousa Hospital Center, Portugal
*Corresponding Author: Joana Pereira, Tâmega e Sousa Hospital Center, Portugal
Received: 16 August 2021; Accepted: 24 August 2021; Published: 28 August 2021
Citation:
Joana Pereira, Ana Sofia Esteves, Pedro Ribeiro, José Miradouro, Helder Nogueira, Jorge Alves. Adult Scheuermann Kyphosis Surgical Treatment by Single Posterior Approach. Journal of Spine Research and Surgery 3 (2021): 091-098.
Share at FacebookAbstract
This is a case report of an 40 years female patient with Scheuermann Kyphosis with a rigid thoracic hyperkyphosis of 90º and compensatory lumbar hyperlordosis of 92º, treated with a single posterior approach, Ponte osteotomy and instrumented posterolateral fusion. There is some discussion about the best surgical approach. Combined approach was classically considered the gold-standard, but recent studies revealed that posterior-only approach allows comparable corrections with less complications rate. Posterior-only approach good results are related with advances in posterior instrumentation combined with posterior column shortening techniques, such Ponte osteotomies. Preoperative planning is essential. Spine instrumentation should extend from proximal end vertebra to sagittal stable vertebra.
Keywords
Scheuermann Disease, Kyphosis, Ponte Osteotomies, Sagittal Stable Vertebra, Proximal End Vertebra, Vitamin D
Scheuermann Disease articles Scheuermann Disease Research articles Scheuermann Disease review articles Scheuermann Disease PubMed articles Scheuermann Disease PubMed Central articles Scheuermann Disease 2023 articles Scheuermann Disease 2024 articles Scheuermann Disease Scopus articles Scheuermann Disease impact factor journals Scheuermann Disease Scopus journals Scheuermann Disease PubMed journals Scheuermann Disease medical journals Scheuermann Disease free journals Scheuermann Disease best journals Scheuermann Disease top journals Scheuermann Disease free medical journals Scheuermann Disease famous journals Scheuermann Disease Google Scholar indexed journals Kyphosis articles Kyphosis Research articles Kyphosis review articles Kyphosis PubMed articles Kyphosis PubMed Central articles Kyphosis 2023 articles Kyphosis 2024 articles Kyphosis Scopus articles Kyphosis impact factor journals Kyphosis Scopus journals Kyphosis PubMed journals Kyphosis medical journals Kyphosis free journals Kyphosis best journals Kyphosis top journals Kyphosis free medical journals Kyphosis famous journals Kyphosis Google Scholar indexed journals Ponte Osteotomies articles Ponte Osteotomies Research articles Ponte Osteotomies review articles Ponte Osteotomies PubMed articles Ponte Osteotomies PubMed Central articles Ponte Osteotomies 2023 articles Ponte Osteotomies 2024 articles Ponte Osteotomies Scopus articles Ponte Osteotomies impact factor journals Ponte Osteotomies Scopus journals Ponte Osteotomies PubMed journals Ponte Osteotomies medical journals Ponte Osteotomies free journals Ponte Osteotomies best journals Ponte Osteotomies top journals Ponte Osteotomies free medical journals Ponte Osteotomies famous journals Ponte Osteotomies Google Scholar indexed journals Sagittal Stable Vertebra articles Sagittal Stable Vertebra Research articles Sagittal Stable Vertebra review articles Sagittal Stable Vertebra PubMed articles Sagittal Stable Vertebra PubMed Central articles Sagittal Stable Vertebra 2023 articles Sagittal Stable Vertebra 2024 articles Sagittal Stable Vertebra Scopus articles Sagittal Stable Vertebra impact factor journals Sagittal Stable Vertebra Scopus journals Sagittal Stable Vertebra PubMed journals Sagittal Stable Vertebra medical journals Sagittal Stable Vertebra free journals Sagittal Stable Vertebra best journals Sagittal Stable Vertebra top journals Sagittal Stable Vertebra free medical journals Sagittal Stable Vertebra famous journals Sagittal Stable Vertebra Google Scholar indexed journals Proximal End Vertebra articles Proximal End Vertebra Research articles Proximal End Vertebra review articles Proximal End Vertebra PubMed articles Proximal End Vertebra PubMed Central articles Proximal End Vertebra 2023 articles Proximal End Vertebra 2024 articles Proximal End Vertebra Scopus articles Proximal End Vertebra impact factor journals Proximal End Vertebra Scopus journals Proximal End Vertebra PubMed journals Proximal End Vertebra medical journals Proximal End Vertebra free journals Proximal End Vertebra best journals Proximal End Vertebra top journals Proximal End Vertebra free medical journals Proximal End Vertebra famous journals Proximal End Vertebra Google Scholar indexed journals Vitamin D articles Vitamin D Research articles Vitamin D review articles Vitamin D PubMed articles Vitamin D PubMed Central articles Vitamin D 2023 articles Vitamin D 2024 articles Vitamin D Scopus articles Vitamin D impact factor journals Vitamin D Scopus journals Vitamin D PubMed journals Vitamin D medical journals Vitamin D free journals Vitamin D best journals Vitamin D top journals Vitamin D free medical journals Vitamin D famous journals Vitamin D Google Scholar indexed journals thoracolumbar articles thoracolumbar Research articles thoracolumbar review articles thoracolumbar PubMed articles thoracolumbar PubMed Central articles thoracolumbar 2023 articles thoracolumbar 2024 articles thoracolumbar Scopus articles thoracolumbar impact factor journals thoracolumbar Scopus journals thoracolumbar PubMed journals thoracolumbar medical journals thoracolumbar free journals thoracolumbar best journals thoracolumbar top journals thoracolumbar free medical journals thoracolumbar famous journals thoracolumbar Google Scholar indexed journals lumbar hyperlordosis articles lumbar hyperlordosis Research articles lumbar hyperlordosis review articles lumbar hyperlordosis PubMed articles lumbar hyperlordosis PubMed Central articles lumbar hyperlordosis 2023 articles lumbar hyperlordosis 2024 articles lumbar hyperlordosis Scopus articles lumbar hyperlordosis impact factor journals lumbar hyperlordosis Scopus journals lumbar hyperlordosis PubMed journals lumbar hyperlordosis medical journals lumbar hyperlordosis free journals lumbar hyperlordosis best journals lumbar hyperlordosis top journals lumbar hyperlordosis free medical journals lumbar hyperlordosis famous journals lumbar hyperlordosis Google Scholar indexed journals anteroposterior articles anteroposterior Research articles anteroposterior review articles anteroposterior PubMed articles anteroposterior PubMed Central articles anteroposterior 2023 articles anteroposterior 2024 articles anteroposterior Scopus articles anteroposterior impact factor journals anteroposterior Scopus journals anteroposterior PubMed journals anteroposterior medical journals anteroposterior free journals anteroposterior best journals anteroposterior top journals anteroposterior free medical journals anteroposterior famous journals anteroposterior Google Scholar indexed journals hiperlordosis articles hiperlordosis Research articles hiperlordosis review articles hiperlordosis PubMed articles hiperlordosis PubMed Central articles hiperlordosis 2023 articles hiperlordosis 2024 articles hiperlordosis Scopus articles hiperlordosis impact factor journals hiperlordosis Scopus journals hiperlordosis PubMed journals hiperlordosis medical journals hiperlordosis free journals hiperlordosis best journals hiperlordosis top journals hiperlordosis free medical journals hiperlordosis famous journals hiperlordosis Google Scholar indexed journals
Article Details
1. Introduction
Scheuermann disease, first described by Holger Werfel Scheuerman in 1921, is an idiopathic structural sagittal plan deformity [1]. It´s traditionally defined as thoracic or thoracolumbar hyperkyphosis caused by three consecutive vertebrae with ≥5º of anterior wedging (Sorensen criteria). Other radiographic changes can be found like endplate irregularity, loss of disc space height and sometimes Schmorl´s nodes [2]. The incidence ranges from 1% to 8% with a male-to-female ratio that ranges from 2:1 to 7:1. Generally it presents in adolescence but a subset of patients present in adulthood [3]. Disease aetiology it’s unknown. It´s believed that it is a result of a development error in collagen aggrega-tion with disturbance of endochondral ossification of the vertebral end plates. This results in wedge-shaped vertebra and increased kyphosis [3].
Disease can be classified into typical and atypical forms. The typical form is more common and comprise a thoracic hyperkyphosis with nonstructural lumbar hyperlordosis. Atypical form, also called type II or lumbar Scheuermann disease, is generally seen in active, athletic periadolescent boys that present with thoracolumbar kyphosis. Changes at thoracolumbar junction are typically painful [3]. Pain and disability are more common in adults with this deformity when compared with other adults with same age [3]. Adult Scheuermann kyphosis can be managed conservative or surgically. Nonsurgical measures include anti- inflammatory drugs and physical therapy. This should focus in postural improvement exercises and trunk extensor strengthening. Deformity correction shouldn’t be expected but may improve general physical conditioning and alleviate pain. Bracing it’s also an option, particularly in patients with severe pain who aren’t surgical candidates. However its role is limited and most times poorly tolerated [3]. Surgery it’s indicated when conservative treatment fail. Indications for surgery are: severe deformity (Cobb >75º), deformity progression, severe pain and functional disability, cosmesis and, rarely, cardiopulmonary (Cobb >100º) or neurological compromise [3-5]. There is some discussion regarding the best approach, fixation levels and use of adjunctive osteotomy techniques [3-9]. This case report presents an 40 years old patient with Scheuermann Kyphosis treated with a single posterior approach, Ponte osteotomy and instrumented posterolateral fusion.
2. Case Report
40 years old, female patient, without relevant medical history, presents with chronic pain (6-8/10 on Visual Analogic Scale) located at thoracolumbar transition and severe disability, with 48% on Oswestry Disability Index (ODI). Patient had a thoracic hyperkyphosis with low flexibility on Adam test (Figure 1). Neurological examination without abnormalities. Routine standing anteroposterior and lateral radiographs of the entire spine confirmed deformity, with a thoracic kyphosis Cobb angle of 90º. Patient had a compensatory lum-bar hyperlordosis with 92º. Sagittal Vertical Axis was - 4,3 cm (Figure 2). An additional view in hyperextension showed a reduction of deformity to 62º (flexibility of 21%) (Figure 3). MRI study exclude intracanalar abnormal changes (Figure 4). Preoperative analytical study revealed a Vitamin D deficiency (4 ng/ml). Deformity correction was performed by single posterior approach, with apical osteotomy’s (Ponte) and D3-L2 instrumented posterolateral fusion. During intervention there were no changes in neuromonitoring signals. Surgical procedure and follow-up evolved without complications. A 40º Cobb angle correction was accomplished. At 3 years follow-up patient had residual pain (VAS 2/10) and a slight functional disability (ODI 18%). Lumbar lordosis improved to 62º and SVA to -3.6cm (Figure 5).

Figure 1: Clinical examination with thoracic hiperkyphosis and lumbar hiperlordosis.
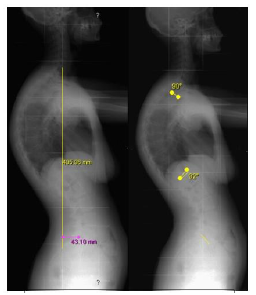
Figure 2: Long spine lateral radiograph with Sagital Vertical Axis of – 4,3 cm, 90º of thoracic hiperkyphosis and 92º of lumbar hyperlordosis.
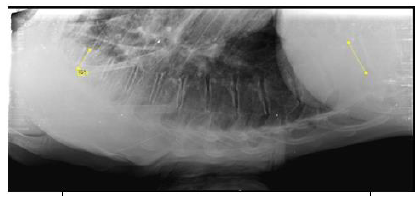
Figure 3: Hiperextension view with thoracic kyphosis reduced to 62º.

Figure 4: MRI without intracanalar abnormalities.
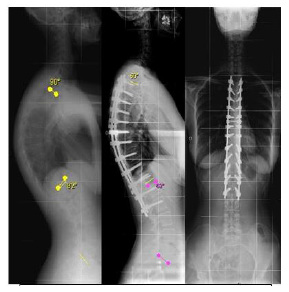
Figure 5: Radiographic study revealing thoracic kyphosis to 50º and compensation of lumbar lordosis to 62º, 3 years after surgery.
3. Discussion
Surgical treatment main goals; are pain relief, functional improvement and deformity correction. It allows deformity correction but also prevents its progression [3-5]. MRI was made to check signs of hernia or other intracanalar pathology that could cause cord compression after deformity correction [3]. Neurological surveillance during surgery it’s mandatory. There is some controversy about the best surgical approach. Correction can be accomplished by anterior-only, combined or posterior-only approach. Since Bradford et al publication in 1980 combined approach was considered the gold-standard [3, 5, 7, 8]. Anterior approach involves interbody release and fusion with segmental instrumentation. It has the advantage of allowing anterior longitudinal ligament release and create an interbody fusion under compression rather tension, as occurs in posterior surgery. Combined approach, with anterior apical release and fusion followed by posterior instrumentation and fusion, is usually reserved for bigger (Cobb angle >80º) and stiffer deformity’s (flexibility <50%), or in the presence of anterior bone bridges.
Advances in posterior instrumentation with advent of pedicle screw fixation, combined with posterior column shortening techniques, such as Ponte osteotomies, turned posterior-only approach the preferred approach in most cases of Scheuermann disease. Ponte osteotomy´s described by Alberto Ponte in 1984, consists of wide facectomies, resection of spinous processes, ligamentum flavum and inferior and superior lamina borders [10]. Posterior only-approach allows corrections compared to combined approaches with less complication rates, even in the presence of large and stiff deformities like in the clinical case presented. It`s associated with less blood loss and shorter surgical time, avoiding a thoracotomy and consequent morbidity [3-5, 7, 8, 11] Preoperative planning of the levels to fuse it´s essential to avoid postoperative junctional kyphosis. Most of the spine surgeons agree that that the upper limit of the fusion must be the proximal end vertebra in the measured kyphosis. On the other end, there is some discussion about the distal fusion level. The current consensus for the distal fusion level is to include the distal end vertebra and first lordotic disc beyond the transitional zone distally.
However, determining the end vertebra isn´t easy because the wedging of the vertebral body and the irregular endplate common in Scheuermann disease. The first lordotic disc it’s defined as the most proximal disc in the lumbar spine whose endplates converge posteriorly, but it´s often difficult to measure the convergence of disc space at transitional thoracolumbar junction. Kyu-Jung et al. developed the sagittal stable vertebra (SSV) concept. SSV is defined as the most proximal vertebra touched by the posterior sacral vertical line (PSVL), which is a line drawn vertically from the posterior-superior corner of the sacrum on the lateral upright radiography. So the lowest instrumented vertebra should include the SSV to avoid impaired sagittal balance and to center fusion mass over the sacrum. This authors have proved that fusion shorter than SSV resulted in the distal end of the fusion mass behind the sacrum, with global sagittal imbalance and a tendency to develop distal junctional kyphosis. Deformity correction shouldn’t exceed 50% of initial curve. Superior corrections are associated with increased risk of junctional kyphosis [4, 7, 9]. After radiographic analysis, D3 was defined as the proximal end vertebra and L2 as the SSV (Figure 6), and our patient was proposed to D3-L2 instrumented posterolateral fusion. This approach allowed a good correction without signs of junctional kyphosis.
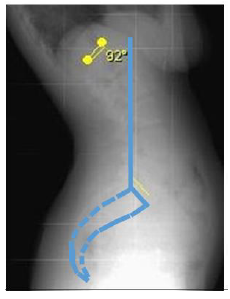
Figure 6: SSV determination. Vertical line drawn from posterior-superior corner of the sacrum (PSVL) touching L2 vertebra on lateral lumbosacral study.
Complications are more frequent in adults. Most common are: loss of correction, junctional kyphosis and infection. Pseudarthrosis its also a fearsome complication in adults, so patients should be optimized previous to surgery [3]. There is evidence that vitamin D deficiency can affect the time and rate of successful arthrodesis [12, 13]. Vitamin D has a central roll in bone metabolism and its deficiency results in low bone mineral density and osteoporosis. Normal values are considered to be >30 ng/ml. Vitamin D levels less than 20 ng/ml are considered as deficiency and levels of 20-30 ng/ml as insufficient levels. Low vitamin D levels are associated with low calcium absorption at intestinal level. This increases parathormone secretion and osteoclast activity which can impair arthrodesis rate or lead to longer times to fusion, with a consequent increase of implant stress and potential loosening. Ravindra et al, recently analysed the relationship between vitamin D deficiency and rates of pseudarthrosis following spine fusion. In their work they find a high rate of vitamin D deficiency (23%) and stablished that vitamin D deficiency was an independent predictor to pseudarthrosis and increased time to fusion [13-18].
In our case we had measured serum Vitamin D levels and found an important deficiency. Patient started vitamin D supplementation, so it was possible to correct a modifiable variable that can affect negatively surgical results and clinical outcome. This clinical case prove that a significant pain relief, good functional outcomes and satisfactory radiological results are possible with a single posterior approach even in larger and stiffer curves. Surgical treatment should be carefully planned. The main goal it’s to achieve correction with a spino-pelvic balance in order to avoid junctional Kyphosis, loosening of the implants, pseudoarthoris and poor clinical outcomes. We recommend extend instrument-tation from proximal end vertebra to SSV. Orthopaedic surgeons and particularly spine surgeons should be aware of the importance of vitamin D deficiency as risk factor for surgical success. We recommend preoperative measure of serum vitamin D to all patients that are elected to surgical treatment and vitamin supple-mentation in the cases of deficiency.
References
- Scheuermann HW. The classic: kyphosis dorsalis juvenilis. Clin Orthop Relat Res (1977): 5-7.
- Sorensen K. Scheuermann’s Juvenile Kyphosis: Clinical Appearances, Radiography, Aetiology and Prognosis. Copenhagen, Denmark, Munksgaard (1964).
- Wood K, Melikian R, Villamil F. Adult Scheurmann Kyphosis: Evaluation, Management, and New Journal of the American Academy of Orthopaedic Surgeons February 20 (2012).
- Etamadifar M, Ebrahimzadeh A, Hadi A, et al. Comparison of Scheuermann’s kyphosis correction by combined anterior–posterior fusion versus posterior-only procedure. Eur Spine J (2015).
- Cobden A, Albayrak A, Camurcu Y, et al. Posterior-Only Approach with Pedicle Screws for the Correction of Scheuermann’s Kyphosis. Asian Spine J 11 (2017): 513-519.
- Ferreira-Alves A, Resina J, Palma- Rodrigues R. Scheuermann kyphosis. The Portuguese technique of surgical treatment. J Bone Joint Surg Br 77 (1995): 943-950.
- Kolier H, Juliane Z, Umstaetter M, et al. Surgical treatment of Scheuermann’s kyphosis using a combined antero-posterior strategy and pedicle screw constructs: efficacy, radiographic and clinical outcomes in 111 cases. Eur Spine J 23 (2014): 180-191.
- Lee SS, Lenke LG, Kuklo TR, et al. Comparison of Scheuermann kyphosis correction by posterior- only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine (Phila Pa 1976) 31 (2006): 2316-2321.
- Cho K, Lenke L, Bridwell K, et al. Selection of the Optimal Distal Fusion Level in Posterior Instrumentation and Fusion for Thoracic Hyperkyphosis. The Sagittal Stable Vertebra Concept. SPINE 34 (2009): 765-770.
- Geck M, Macagno A, Ponte A, et al. The Ponte Procedure. Posterior Only Treatment of Scheuermann’s Kyphosis Using Segmental Posterior Shortening and Pedicle Screw Instrumentation. J Spinal Disord Tech 20 (2007).
- Bradford DS, Moe JH, Montalvo FJ, et al. Scheuermann’s kyphosis: results of surgical treatment by posterior spine arthrodesis in twenty-two patients. J Bone Joint Surg Am 57 (1975): 439-448.
- Kerezoudis P, Rinaldo L, Drazin D, et al. Association Between Vitamin D Deficiency and Outcomes Following Spinal Fusion Surgery: A Systematic Review. World Neurosurgery 95 (2016): 71-76.
- Ravindra V, Godzik J, Dailey A, et al. Vitamin D Levels and 1-Year Fusion Outcomes in Elective Spine Surgery. SPINE 40 (2015): 1536-1541.
- Palazzo C, Sailhan F, Revel M. Scheuermann’s disease: an update. Joint Bone Spine 81 (2014): 209-214.
- Poolman RW, Been HD, Ubags LH. Clinical outcome and radiographic results after operative treatment of Scheuermann disease. Eur Spine J 11 (2002): 561-569.
- Schwalfenberg G. Improvement of chronic back pain or failed back surgery with vitamin D repletion: a case series. J Am Board Fam Med 22 (2009): 69-74.
- Kim TH, Yoon JY, Lee BH, et al. Changes in vitamin D status after surgery in female patients with lumbar spinal stenosis and its clinical significance. Spine 37 (2012): E1326-1330.
- Stoker GE, Buchowski JM, Bridwell KH, et al. Preoperative vitamin D status of adults undergoing surgical spinal fusion. Spine 38 (2013): 507.
