Addressing Female Sexual Dysfunction during Novel 2019-Coronavirus Pandemic in Infertile Women Living in North-East Italy
Article Information
Loris Marin1*, Alessandra Andrisani1, Giovanni Buzzaccarini1, Giampiero Capobianco2, Francesco Dessole2, Eugenio Ragazzi3, Giulia Manzin4, Stefania Mannarini4, Guido Ambrosini1
1Department of Women’s and Children’s Health, University of Padua, Padua, Italy
2Department of Surgical, Microsurgical and Medical Sciences, Gynecologic and Obstetric Clinic, University of Sassari, Sassari, Italy
3Department of Pharmaceutical and Pharmacological Sciences, University of Padua, Padua, Italy
4Department of Philosophy, Sociology, Education, and Applied Psychology, Section of Applied Psychology, University of Padua, Padua, Italy
*Corresponding author: Loris Marin, Department of women’s and children’s health, University of Padua, Via Giustiniani 3, 35100, Padova, Italy
Received: 01 February 2021; Accepted: 11 February 2021; Published: 17 February 2021
Citation:
Loris Marin, Alessandra Andrisani, Giovanni Buzzaccarini, Giampiero Capobianco, Francesco Dessole, Eugenio Ragazzi, Giulia Manzin, Stefania Mannarini, Guido Ambrosini. Addressing Female Sexual Dysfunction during Novel 2019-Coronavirus Pandemic in Infertile Women Living in North-East Italy. Journal of Women’s Health and Development 4 (2021): 026-035.
Share at FacebookAbstract
Objectives: To identify whether the coronavirus infection had a negative influence on female sexual function of infertile women living in North-East Italy.
Methods: A survey was submitted during SARS-CoV-2 pandemic to 570 infertile women. The survey consisted of questions regarding employment, whether respon-dents lived with a partner or other family members, the time spent seeking pregnancy and previously assisted reproductive technology treatments and of the self-reported validated Italian Female Sexual Function Index questionnaire. A cut-off total score of ≤ 26.55 has been used for diagnosis of female sexual dysfunction.
Results: The survey response rate was 17.8%. The mean intercourse frequency during SARS-CoV-2 pandemic was >10 times month in 12.7%, 5-10 times month in 35.3%, 5-10 times month in 38%. The total median FSFI score was 27.4. A positive correlation has been shown between intercourse frequency and occupation, living with a partner or other family members, the time spent seeking a pregnancy and previous assisted reproductive treatments. No significant difference was seen regarding the type of treatment.
Conclusion: Most women scored well in sexual domains during SARS-CoV-2 pandemic. Indeed, as a consequence of their infertility, they seem to have a better coping strategy than the general population.
Keywords
Covid-19, Female Sexual Dysfunction, Italian Female Sexual Function Index, Infertility
Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Female Sexual Dysfunction articles Female Sexual Dysfunction Research articles Female Sexual Dysfunction review articles Female Sexual Dysfunction PubMed articles Female Sexual Dysfunction PubMed Central articles Female Sexual Dysfunction 2023 articles Female Sexual Dysfunction 2024 articles Female Sexual Dysfunction Scopus articles Female Sexual Dysfunction impact factor journals Female Sexual Dysfunction Scopus journals Female Sexual Dysfunction PubMed journals Female Sexual Dysfunction medical journals Female Sexual Dysfunction free journals Female Sexual Dysfunction best journals Female Sexual Dysfunction top journals Female Sexual Dysfunction free medical journals Female Sexual Dysfunction famous journals Female Sexual Dysfunction Google Scholar indexed journals Italian Female Sexual Function Index articles Italian Female Sexual Function Index Research articles Italian Female Sexual Function Index review articles Italian Female Sexual Function Index PubMed articles Italian Female Sexual Function Index PubMed Central articles Italian Female Sexual Function Index 2023 articles Italian Female Sexual Function Index 2024 articles Italian Female Sexual Function Index Scopus articles Italian Female Sexual Function Index impact factor journals Italian Female Sexual Function Index Scopus journals Italian Female Sexual Function Index PubMed journals Italian Female Sexual Function Index medical journals Italian Female Sexual Function Index free journals Italian Female Sexual Function Index best journals Italian Female Sexual Function Index top journals Italian Female Sexual Function Index free medical journals Italian Female Sexual Function Index famous journals Italian Female Sexual Function Index Google Scholar indexed journals Infertility articles Infertility Research articles Infertility review articles Infertility PubMed articles Infertility PubMed Central articles Infertility 2023 articles Infertility 2024 articles Infertility Scopus articles Infertility impact factor journals Infertility Scopus journals Infertility PubMed journals Infertility medical journals Infertility free journals Infertility best journals Infertility top journals Infertility free medical journals Infertility famous journals Infertility Google Scholar indexed journals Coronavirusá articles Coronavirusá Research articles Coronavirusá review articles Coronavirusá PubMed articles Coronavirusá PubMed Central articles Coronavirusá 2023 articles Coronavirusá 2024 articles Coronavirusá Scopus articles Coronavirusá impact factor journals Coronavirusá Scopus journals Coronavirusá PubMed journals Coronavirusá medical journals Coronavirusá free journals Coronavirusá best journals Coronavirusá top journals Coronavirusá free medical journals Coronavirusá famous journals Coronavirusá Google Scholar indexed journals reproductive technology articles reproductive technology Research articles reproductive technology review articles reproductive technology PubMed articles reproductive technology PubMed Central articles reproductive technology 2023 articles reproductive technology 2024 articles reproductive technology Scopus articles reproductive technology impact factor journals reproductive technology Scopus journals reproductive technology PubMed journals reproductive technology medical journals reproductive technology free journals reproductive technology best journals reproductive technology top journals reproductive technology free medical journals reproductive technology famous journals reproductive technology Google Scholar indexed journals intercourseá articles intercourseá Research articles intercourseá review articles intercourseá PubMed articles intercourseá PubMed Central articles intercourseá 2023 articles intercourseá 2024 articles intercourseá Scopus articles intercourseá impact factor journals intercourseá Scopus journals intercourseá PubMed journals intercourseá medical journals intercourseá free journals intercourseá best journals intercourseá top journals intercourseá free medical journals intercourseá famous journals intercourseá Google Scholar indexed journals Infertile Women articles Infertile Women Research articles Infertile Women review articles Infertile Women PubMed articles Infertile Women PubMed Central articles Infertile Women 2023 articles Infertile Women 2024 articles Infertile Women Scopus articles Infertile Women impact factor journals Infertile Women Scopus journals Infertile Women PubMed journals Infertile Women medical journals Infertile Women free journals Infertile Women best journals Infertile Women top journals Infertile Women free medical journals Infertile Women famous journals Infertile Women Google Scholar indexed journals Sexual Dysfunction articles Sexual Dysfunction Research articles Sexual Dysfunction review articles Sexual Dysfunction PubMed articles Sexual Dysfunction PubMed Central articles Sexual Dysfunction 2023 articles Sexual Dysfunction 2024 articles Sexual Dysfunction Scopus articles Sexual Dysfunction impact factor journals Sexual Dysfunction Scopus journals Sexual Dysfunction PubMed journals Sexual Dysfunction medical journals Sexual Dysfunction free journals Sexual Dysfunction best journals Sexual Dysfunction top journals Sexual Dysfunction free medical journals Sexual Dysfunction famous journals Sexual Dysfunction Google Scholar indexed journals Children?s Health articles Children?s Health Research articles Children?s Health review articles Children?s Health PubMed articles Children?s Health PubMed Central articles Children?s Health 2023 articles Children?s Health 2024 articles Children?s Health Scopus articles Children?s Health impact factor journals Children?s Health Scopus journals Children?s Health PubMed journals Children?s Health medical journals Children?s Health free journals Children?s Health best journals Children?s Health top journals Children?s Health free medical journals Children?s Health famous journals Children?s Health Google Scholar indexed journals
Article Details
1. Introduction
Novel 2019-Coronavirus (SARS-CoV-2) pandemic became widespread from February 2020 and many countries all over the world implemented unprecedented strict quarantine measures. In the post-peak infection, containment measures continue to be operative to reduce the risk of new outbreaks. These contagion prevention measures have caused significant adverse effects to people’s physical health and lives due to isolation and anxiety created by the fear of contracting the SARS-CoV-2 infection [1]. Posttraumatic stress disease and impairment in sleep quality have been linked to the virus infection with a significant prevalence in the female population [2]. Women also seem to face other peculiar sexual issues. Despite an increase in sexual desire and sexual intercourse frequency during this pandemic, an increase in menstrual disorders and a decrease in sexual well-being have also been reported [3]. Infertility is a detrimental condition affecting 8-12% of couples in developed countries [4] and it causes negative emotions [5] and psychological distress and may hamper the marital relationship and sexual wellbeing [6]. Sexual dysfunction is known to affect infertile women and all sexual domains are affected, in particular lubrication, orgasm, and satisfaction [7-9]. It seems quite reasonable that during SARS-CoV-2 pandemic, infertile women faced stress and anxiety due to both fear of virus infection and infertility issues. The aim of the study is to assess female sexual wellbeing through the Italian validated Female Sexual Function Index (FSFI) test in a population of infertile women during SARS-CoV-2 pandemic. To the best of our knowledge, this is the first original article combining sexual dysfunction rising from both infertility and SARS-CoV-2 pandemic.
2. Materials and Methods
The aims of this study were: (a) to identify whether the SARS-CoV-2 pandemic had a negative influence on female sexual function of infertile women living in North-East Italy and (b) to explore whether employment, cohabitation with a partner or other family members, the time spent seeking pregnancy and previously assisted reproductive technology (ART) treatments could contribute in coping stress during SARS-CoV-2 pandemic. This is an observational study of infertile women enrolled in a longitudinal research cohort at a single academic center. All infertile women who attended IVF Unit at Padua University Hospital in the north-east Italy between January 2017 and December 2019 (570 women) and met the inclusion criteria were enrolled. As questions of the questionnaire concern the four weeks preceding the compilation of the same, the time to answer the survey started on the 1 April 2020 and ended on 1 May 2020, covering the month during which there was the peak of SARS-CoV-2 infections in Italy and the implementation of the strictest restriction measures. Inclusion criteria were: infertile women age between 18 and 50 years and completion of the survey. This study was exempt from the approval of the ethical review committee, because the procedure was part of the healthcare assistance protocol provided to infertile women. All subjects provided their consent prior to their participation in the study. All patients were asked to fill in a short anamnestic questionnaire and to complete the self-reported Italian validated version of the FSFI questionnaire. The questionnaire allows us to obtain individual domain scores and full-scale scores up to 36), with higher scores indicating better female sexual function [10, 11]. A cutoff score of 26, 55 has been used to diagnose sexual dysfunction. The test, which includes 19 questions, assesses sexual function during a 4-week period on a 5-point scale with excellent psychometric properties and evaluates six domains including desire, arousal, lubrication, orgasm, satisfaction and pain [12]. Each domain has his own impact on the final score.
2.1 Data analysis
The statistical analysis was performed using JMP® Version Pro 14 software for Windows (SAS Institute Inc, Cary, NC, USA) and Microsoft Excel 365, Version 2004. The Shapiro–Wilk W test was used to check the normality of the quantitative variables. Quantitative data are expressed as median (with min-max values). Qualitative data are expressed as frequencies and percentages. Comparisons between quantitative variables were obtained with Wilcoxon/Kruskal-Wallis non-parametric test or Mann–Whitney U test. Comparisons between qualitative variables were performed with Pearson’s chi-square test. The relationships between variables was explored with Spearman’s ρ non-parametric correlation coefficient. The non-parametric multivariate method of Principal Component Analysis was also used to assess any relationships among answers from FSFI questionnaire, considering answers from each item, or grouped as domains [11]. Cluster analysis (Ward’s method) was used as an additional exploratory technique in order to find grouping among patients, according to answers to FSFI questionnaire. For all the statistical evaluations, a P<0.05 was considered statistically significant.
3. Results
The survey response rate was 17.8% (101/570); 101 women completed the questionnaire and were included in the study. Baseline characteristics of study participants are reported in Table 1. At the time of the survey, median age was 36.9 years (26 - 50) and 81.4% were Italian. 59.8% of the participants were born in Veneto, a region of north east Italy where the in vitro fertilization center is located and one of the most affected by SARS-CoV-2. 84.3% of the women are employed. Among employed women (86), 14.7% work in healthcare. Partners are employed in 94.1% and 5.2% work in healthcare. In the four weeks preceding the compilation of the questionnaire, most of the women lived only with their partner (76.5%), 22.5% also lived with other family members and 1% lived alone. Infertility duration mean is 4.7 ± 3.7 years. At the time of the survey, participating women had already performed an ART treatment in 52.9%, in particular 13.7 % performed timed intercourse, 19.6% intrauterine insemination and 66.7% IVF treatment. The mean intercourse frequency during SARS-CoV-2 pandemic was >10 times month in 12.7%, 5-10 times month in 35.3%, 5-10 times month in 38%, 1-2 times month in 9%, and less than once month in 4% of cases.
3.1 Female Sexual Function Index domains and total FSFI score
A cut-off total score of ≤ 26.55 has been used for the diagnosis of female sexual dysfunction [10]. Forty-three women (42.57%) showed a total score of lower than 26.55 in our study. The entire cohort showed a FSFI score divided per domain as described in Table 2. The total FSFI score distribution shows a tri-modal pattern (Figure 1). Spearman’s and Mann-Whitney analysis has been performed in order to find the correlation between general features and FSFI items. All domains were significantly correlated to intercourse frequency (Table 3). Desire domain significantly correlated with age (p 0.02), arousal domain significantly correlated to women’s work occupation (p 0.02), lubrication domain significantly correlated to age (p 0.05) and women’s occupation (p 0.04), and pain domain significantly correlated to presence of family members (p 0.02) (Table 3). Related to general features, intercourse frequency has been correlated to patient characteristics (Supplement file 1). A positive correlation has been shown between intercourse frequency and occupation (P 0.003), living with a partner or other family members (P 0.0306), the time spent seeking a pregnancy (P < 0.001) and previous ART treatments (P 0.044). However, no significant difference was seen regarding the type of ART treatment. Total domain and answer distribution for every patient involved in the study are shown in Figure 2. Graphically, a blue spot means lower scores and a red spot higher scores.
|
Parameter |
Median or frequencya |
|
Age (y) |
36 (26-50) |
|
Infertility duration (months) |
48 (12-288) |
|
Country of origin (Italy/abroad) |
82/19 (81%/19%) |
|
Job (yes/no) |
86/15 (85%/15%) |
|
Healthcare worker (yes/no) |
14/87 (14%/86%) |
|
Partner’s job (yes/no) |
96/5 (95%/5%) |
|
Partner is a healthcare workerb (yes/no) |
5/95 (5%/95%) |
|
Cohabitants (alone/with partner only/with partner and other family members) |
1/77/23 (1%/76%/23%) |
|
Family membersb (parents or relatives/children/children and parents or relatives) |
8/14/1 (35%/61%/4%) |
|
PMA treatmentsb (yes/no) |
49/52 (49%/51%) |
|
Treatment typeb (timed intercourse/IUI/FIVET-ICSI) |
7/10/34 (14%/20%/66%) |
|
Intercourse frequencyc (level 0/1/2/3/4) |
4/9/39/36/13 (4%/9%/38%/35%/13%) |
a Quantitative variables are expressed as median (in parentheses are min-max values). Qualitative values are expressed as frequencies (in parentheses are percentages).
b Some data are lacking.
c Intercourse frequency was categorized as level 0: <1 once/month; level 1: 1-2 times/month; level 2: 2-5 times/month; level 3: 5-10 times/month; level 4: >10 times/month.
Table 1: General characteristics of the cohort (n=101).
|
FSFI Domain |
Item number |
Median score (range) |
|
Desire |
1,2 |
4.2 (0.6-5.4) |
|
Arousal |
3,4,5,6 |
4.2 (0-5.7) |
|
Lubrification |
7,8,9,10 |
5.1 (0-6) |
|
Orgasm |
11,12,13 |
4.8 (0-6) |
|
Satisfaction |
14,15,16 |
4.8 (0-6) |
|
Pain |
17,18,19 |
5.6 (0-6) |
|
Total score |
1-19 |
27.4 (0.6-34.8) |
Table 2: Domain scoring obtained with FSFI in the considered cohort.
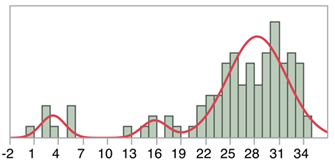
Figure 1: The total FSFI score distribution.
a P according to Spearman’s ρ non-parametric correlation coefficient.
b P according to Mann-Whitney U or c Kruskal-Wallis non-parametric tests.
* denotes a statistically significant value when P<0.05.
Table 3: Significance levels (P) of relationships between various parameters and FSFI domains.
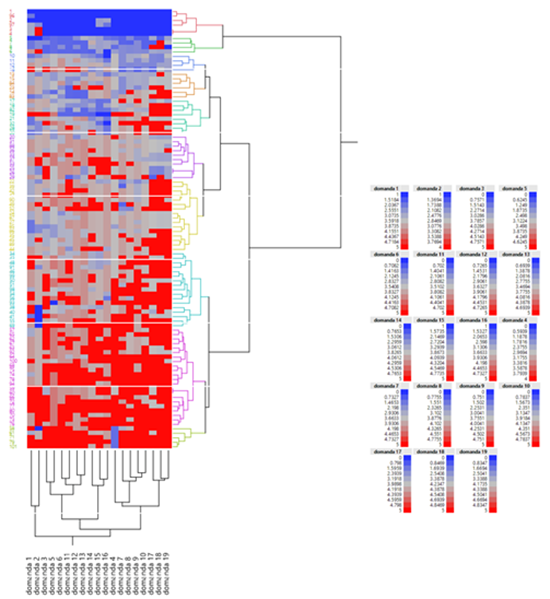
Figure 2: shows total domains and answers distribution for every patient involved in the study. Graphically, blue spot means lower scores and red spot higher scores.
|
Parameter |
P for Intercourse frequencyc |
|
Agea (y) |
0.7733 |
|
Jobb |
0.0028* |
|
Healthcare workerb |
0.3464 |
|
Partner’s jobb |
0.1553 |
|
Partner is a healthcare workerb |
0.2377 |
|
Cohabitantsb |
0.0306* |
|
Family membersb |
0.5093 |
|
Pregnancy seeking timeb |
0.0008* |
|
PMA treatmentsb |
0.0438* |
|
Treatment typeb |
0.1317 |
a P according to Wilcoxon/Kruskal-Wallis non-parametric test.
b P according to Pearson’s chi-square test.
c Intercourse frequency was categorized as level 0: <1 once/month; level 1: 1-2 times/month; level 2: 2-5 times/month; level 3: 5-10 times/month; level 4: >10 times/month.
* denotes a statistically significant value when P<0.05.
Table 4: Significance levels (P) of statistical evaluation of any relationships between Intercourse frequency and various parameters considered in the cohort.
4. Discussion
This study evaluated the effects of SARS-CoV-2 pandemic on sexual dysfunction in infertile women through a validate questionnaire. Our findings indicate that sexual dysfunction was low among infertile women. On average, they achieved good results in all investigated domains in the considered time frame. Sexual intercourse carried out to achieve pregnancy, often tied to the timing of ongoing treatments, can have a psychological impact and cause sexual dysfunction. Furthermore, when there is long-lasting infertility or pregnancy can be achieved only through ART treatments, there is a decrease in the frequency of sexual intercourse and a higher incidence of sexual dysfunction [13]. Female sexual dysfunction has a negative role on quality of life and this can worsen depressive symptoms [6]. The strict quarantine has kept a large number of people in isolation and has brought psychological stress. According to a study focusing on a Chinese population, young women aged 18-30 years old reported significantly higher psychological distress. Moreover, according to International Societies, all scheduled ARTs have been delayed during SARS-CoV-2 pandemic in order to avoid the infection spreading and because the real impact of SARS-CoV-2 on early phases of pregnancy was not known yet. This implies a delay in obtaining a pregnancy for couples who would like to have one as soon as possible and a situation of uncertainty about the possible effects of this new virus on the fetus. For couples who are looking for a child, infertility is an event that has a strong detrimental emotional impact. Moreover, ARTs worsen mental distress and are related to higher levels of depression, anxiety and distress. Conflicting results were obtained by evaluating the impact of these symptoms on the probability of getting pregnant. Psychosocial distress could however worsen the outcome of ART treatments [14]. Surprisingly our results show a positive situation, the median total score of the FSFI is comparable to the general population [15]. Only less than the half of the participants (42.57%) in our study showed results that may be considered at risk for sexual dysfunction. This is an unexpected result because many studies show that infertility has a significant role in sexual dysfunction [16] A study showed that out of 500 patients, of which 267 (53.4%) were suffering from infertility while 233 (46.6%) were fertile women, out of infertile females 63.67% patients had sexual dysfunction as compared to 46.35% of fertile females [17]. A recent review [18] showed that most studies confirmed the negative effects of infertility on couples’ sexuality.
The main result of the study is that infertile couples during SARS-CoV-2 period show a good level of sexual function. A study that analyzed sexual behavior during SARS-CoV-2 reports a lower total FSFI score during the last pandemic than before, but above all it shows much lower total scores than those obtained in the present study: FSFI scores before the pandemic compared with scores during the pandemic were 20.52 and 17.56 (P=0.001) [3]. We may hypothesize that a high sexual function score in infertile couples during such a period of distress may be explained because these couples already used to live a stressful situation due to infertility that has perhaps led them to develop coping strategies that are protective against further stressful events; also, in this period people have spent much more time at home. Some FSFI domains have positive significant correlations with the general characteristics of the cohort. The age variable has significant positive correlations to the desire and lubrication domains. In literature we find contrary data, usually low sexual desire is strongly influenced by age [19]; according to one of the largest probability studies focused on women's sexual function, low sexual desire is experienced by the majority (75%) of older women, 39% of women aged 45-64, and 22% of younger women [20]. The study sample, however, is made up of women with fertility issues, the increase in age could therefore be a variable related to the increase in the desire for motherhood, which could explain a greater sexual desire, accompanied by a greater lubrication before and during sexual intercourse. Despite the median age of participants suffering from infertility being 36, lower than usual cohorts, only 25% of the women are older than 41 and this could be another explanation for the high correlation.
The frequency of sexual intercourse correlates with all the domains. This means that the more the woman experiences sexual intercourse with desire, arousal, lubrication, satisfaction, orgasm and less pain, the more frequent sexual intercourse, or vice versa, statistically we are unable to describe the direction of correlation. The analysis of the relationship between the intercourse frequency and the characteristics of the sample shows positive and significant correlations between this variable and being a worker, having other people living at home, more time spent seeking a pregnancy and participation to ART’s treatments. Women with these characteristics are those who report a higher frequency of sexual intercourse. The distribution of total scores calculated on the FSFI questionnaire shows that three different values appear with the maximum frequency in the distribution of data (three modes). This means that the participants were observed in three very different ways, we have a median with a low value, towards the left end of the distribution, probably made up of the group of women who had extremely low total score (Figure 1), these are probably the women who indicated an absent/almost absent sexual activity, their results are much lower than the first quartile (75% of the participants have a total score higher than 23.375). The second curve represents another group of women who have a low total score, even lower than the first quartile and therefore lower than the cut-off, which includes a group of women who are possibly at risk of sexual dysfunction and may be women who had sexual intercourse less frequently. Most of the participants gather around the third mode, perhaps the last group of the trimodal distribution includes women who had sexual intercourse more frequently. This last data allows us to observe that most of the participants obtained a total score ranging from 23.375 to a maximum score of 34.8. This group therefore includes some women considered at risk and women with good sexual functioning. As can be seen graphically in Figure 1 the average of this group is around a score of 28, higher than the cut-off. The trimodal distribution therefore indicates two groups of participants who could certainly benefit from a clinical observation and a third group which shows a wide range of scores, some lower than the cut-off score, others on the cut-off and most of them over the FSFI cut-off, showing good sexual function.
One of the limits of the submitted test is no sexual activity or intercourse that implies that many answers receive zero point. In our survey 7% of women had no sexual activity or intercourse. To explain this rate, it is interesting to note that 14% of the women interviewed work in healthcare. SARS-CoV-2 has placed great strain on the entire healthcare system with the critical issue of healthcare workers psychological well-being. Moreover, because of unavailability of healthcare workers in Italy, many workers had to work also longer than usual. Another limit is that we do not present data that allows us to clearly say if and which part of the questionnaire was influenced by the quarantine. Despite these limitations, we observed that the prevalence of general sexual dysfunction was low among infertile women, less than half of the cohort showed results lower than the cut-off scores. The female infertile population during the pandemic probably did not have particular problems in sexual functioning, instead they reported high levels of desire, arousal, lubrication, orgasm, satisfaction and low levels of pain during sexual intercourse, indicating an absence of any sexual dysfunction in most of the patients.
Conflicts of Interest
None of the authors have any conflicts of interest to declare. This study had no funding.
References
- Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, et al. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. International journal of environmental research and public health 17 (2020).
- Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry research 287 (2020): 112921.
- Yuksel B, Ozgor F. Effect of the COVID-19 pandemic on female sexual behavior. International journal of gynaecology and obstetrics. the official organ of the International Federation of Gynaecology and Obstetrics 150 (2020): 98-102.
- Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clinical biochemistry 62 (2018): 2-10.
- Mannarini S, Boffo M, Bertucci V, et al. A Rasch-based dimension of delivery experience: spontaneous vs. medically assisted conception. Journal of clinical nursing 22 (2013): 2404-2416.
- Luk BH, Loke AY. The Impact of Infertility on the Psychological Well-Being, Marital Relationships, Sexual Relationships, and Quality of Life of Couples: A Systematic Review. Journal of sex & marital therapy 41 (2015): 610-625.
- Mendonça CR, Arruda JT, Noll M, et al. Sexual dysfunction in infertile women: A systematic review and meta-analysis. European journal of obstetrics, gynecology, and reproductive biology 215 (2017): 153-163.
- Omani-Samani R, Amini P, Navid B, et al. Prevalence of Sexual Dysfunction among Infertile Women in Iran: A Systematic Review and Meta-analysis. International journal of fertility & sterility 12 (2019): 278-283.
- Maroufizadeh S, Riazi H, Lotfollahi H, et al. The 6-item Female Sexual Function Index (FSFI-6): factor structure, reliability, and demographic correlates among infertile women in Iran. Middle East Fertility Society Journal 24 (2019): 6.
- Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. Journal of sex & marital therapy 31 (2005): 1-20.
- Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of sex & marital therapy 26 (2000): 191-208.
- Meston C, Trapnell P. Development and validation of a five-factor sexual satisfaction and distress scale for women: the Sexual Satisfaction Scale for Women (SSS-W). The journal of sexual medicine 2 (2005): 66-81.
- Read J. Sexual problems associated with infertility, pregnancy, and ageing. BMJ (Clinical research ed) 329 (2004): 559-561.
- Purewal S, Chapman SCE, van den Akker OBA. A systematic review and meta-analysis of psychological predictors of successful assisted reproductive technologies. BMC research notes 10 (2017): 711.
- Nappi RE, Albani F, Vaccaro P, et al. Use of the Italian translation of the Female Sexual Function Index (FSFI) in routine gynecological practice. Gynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology 24 (2008): 214-219.
- Braverman AM. Psychosocial aspects of infertility: sexual dysfunction. International Congress Series 1266 (2004): 7.
- Aggarwal RS, Mishra VV, Jasani AF. Incidence and prevalence of sexual dysfunction in infertile females. Middle East Fertility Society Journal 18 (2013): 4.
- Starc A, Trampuš M, Pavan Jukic D, et al. Infertility and Sexual Dysfunctions: A Systematic Literature Review. Acta clinica Croatica 58 (2019): 508-515.
- Dennerstein L, Dudley E, Burger H. Are changes in sexual functioning during midlife due to aging or menopause?. Fertility and sterility 76 (2001): 456-460.
- Shifren JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women: prevalence and correlates. Obstetrics and gynecology 112 (2008): 970-978.
