Acute Pancreatitis Following the Third Dose of the BNT162b2 COVID-19 Vaccine
Article Information
Omar Fakhreddine1, Omar Chaabo1, Alaa Sharara2, Mohammad Samir Arnaout1*
1Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
2Division of Gastroenterology, department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
*Corresponding Author: Mohamad Samir Arnaout, Professor of clinical medicine, Internal medicine department Cardiology division, American University of Beirut Medical Center, Beirut, Lebanon
Received: 11 March 2022; Accepted: 29 March 2022; Published: 18 April 2022
Citation:
Omar Fakhreddine, Omar Chaabo, Alaa Sharara, Mohammad Samir Arnaout. Acute Pancreatitis Following the Third Dose of the BNT162b2 COVID-19 Vaccine. Archives of Clinical and Medical Case Reports 6 (2022): 278-280.
Share at FacebookAbstract
In December 2020, BNT162b2 vaccine developed by Pfizer and BioNTech became the first mRNA-based vaccine approved for human use against COVID-19. The emergence of such techniques in vaccine development have raised concerns about possible side effects. We present the case of a 64-year-old male who presented with acute onset of severe diffuse abdominal pain few days after receiving the third dose of Pfizer BioNTech COVID-19 vaccine. He was diagnosed with acute pancreatitis based on his lipase level of 1483 U/L as well as radiological evidence of pancreatic inflammation. Investigations were unable to detect any evident etiology. He was admitted for observation and conservative management for 24 hours, after which he was discharged home. Few cases of bouts of acute pancreatitis have been reported after the first and second dose of BNT162b2 vaccine. To our knowledge this is the first case of acute pancreatitis after the third dose of vaccine.
Keywords
BNT162b2 vaccine; COVID-19; Pancreatic inflammation; Pfizer and BioNTech
BNT162b2 vaccine articles; COVID-19 articles; Pancreatic inflammation articles; Pfizer and BioNTech articles
BNT162b2 vaccine articles BNT162b2 vaccine Research articles BNT162b2 vaccine review articles BNT162b2 vaccine PubMed articles BNT162b2 vaccine PubMed Central articles BNT162b2 vaccine 2023 articles BNT162b2 vaccine 2024 articles BNT162b2 vaccine Scopus articles BNT162b2 vaccine impact factor journals BNT162b2 vaccine Scopus journals BNT162b2 vaccine PubMed journals BNT162b2 vaccine medical journals BNT162b2 vaccine free journals BNT162b2 vaccine best journals BNT162b2 vaccine top journals BNT162b2 vaccine free medical journals BNT162b2 vaccine famous journals BNT162b2 vaccine Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals cancer articles cancer Research articles cancer review articles cancer PubMed articles cancer PubMed Central articles cancer 2023 articles cancer 2024 articles cancer Scopus articles cancer impact factor journals cancer Scopus journals cancer PubMed journals cancer medical journals cancer free journals cancer best journals cancer top journals cancer free medical journals cancer famous journals cancer Google Scholar indexed journals Splenectomy articles Splenectomy Research articles Splenectomy review articles Splenectomy PubMed articles Splenectomy PubMed Central articles Splenectomy 2023 articles Splenectomy 2024 articles Splenectomy Scopus articles Splenectomy impact factor journals Splenectomy Scopus journals Splenectomy PubMed journals Splenectomy medical journals Splenectomy free journals Splenectomy best journals Splenectomy top journals Splenectomy free medical journals Splenectomy famous journals Splenectomy Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Radiology articles Radiology Research articles Radiology review articles Radiology PubMed articles Radiology PubMed Central articles Radiology 2023 articles Radiology 2024 articles Radiology Scopus articles Radiology impact factor journals Radiology Scopus journals Radiology PubMed journals Radiology medical journals Radiology free journals Radiology best journals Radiology top journals Radiology free medical journals Radiology famous journals Radiology Google Scholar indexed journals Pancreatic inflammation articles Pancreatic inflammation Research articles Pancreatic inflammation review articles Pancreatic inflammation PubMed articles Pancreatic inflammation PubMed Central articles Pancreatic inflammation 2023 articles Pancreatic inflammation 2024 articles Pancreatic inflammation Scopus articles Pancreatic inflammation impact factor journals Pancreatic inflammation Scopus journals Pancreatic inflammation PubMed journals Pancreatic inflammation medical journals Pancreatic inflammation free journals Pancreatic inflammation best journals Pancreatic inflammation top journals Pancreatic inflammation free medical journals Pancreatic inflammation famous journals Pancreatic inflammation Google Scholar indexed journals Pfizer and BioNTech articles Pfizer and BioNTech Research articles Pfizer and BioNTech review articles Pfizer and BioNTech PubMed articles Pfizer and BioNTech PubMed Central articles Pfizer and BioNTech 2023 articles Pfizer and BioNTech 2024 articles Pfizer and BioNTech Scopus articles Pfizer and BioNTech impact factor journals Pfizer and BioNTech Scopus journals Pfizer and BioNTech PubMed journals Pfizer and BioNTech medical journals Pfizer and BioNTech free journals Pfizer and BioNTech best journals Pfizer and BioNTech top journals Pfizer and BioNTech free medical journals Pfizer and BioNTech famous journals Pfizer and BioNTech Google Scholar indexed journals
Article Details
1. Case Presentation
We present the case of a 64-year-old male who presented to the emergency department complaining of few hours’ history of diffuse abdominal pain that awakened him from sleep. The pain was stabbing in nature, severe in intensity (9/10) with no radiations. It was as associated with low grade fever, myalgia, arthralgia, generalized fatigue as well as nausea. He denied vomiting or diarrhea. The patient also denied use of any new medications, no dietary changes or any recent travel or sick contacts. He is previously healthy, with no significant surgical history. He is not receiving any chronic medications. He does not smoke or use alcohol. To note that few days prior to his presentation, the patient received his third dose of the BNT162b2 COVID-19 vaccine. He doesn’t report any similar episodes after receiving the first two doses.
Upon presentation, his vital signs were within normal limits. On physical examination, he had epigastric abdominal tenderness. Laboratory work up including a CBCD, chemistry panel, liver function test, TSH, lipid panel, cardiac enzymes and electrocardiogram were normal. Lipase level was 1483 U/L. CT scan of the abdomen was done and showed a mildly edematous pancreas with peripancreatic inflammatory changes and fluid consistent with acute interstitial pancreatitis. Ultrasound of the gallbladder showed no evidence of cholelithiasis.
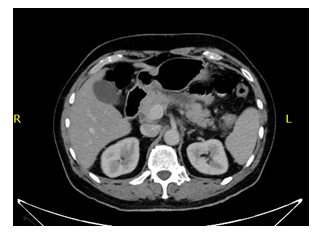
Figure 1: CT scan of the abdomen showing a mildly edematous pancreas with peripancreatic inflammatory changes and fluid.
The patient was diagnosed with acute pancreatitis and admitted to the hospital for 24 hours monitoring and conservative management including intravenous hydration and pain medications. The following day his pain has resolved and he was discharged home. Lipase level was followed few days later and trended down to 54. Given the lack of risk factors of acute pancreatitis and the timing between the administration of the third dose of COVID-19 vaccine administration and the appearance of symptoms, we suspected the vaccine as a possible cause of acute pancreatitis.
2. Discussion
Acute pancreatitis is defined as an inflammatory condition of the pancreas and it is recognized as one of most common causes of gastrointestinal-related hospitalization in the United States [1]. Its presentation varies widely from mild disease that requires conservative management to severe and complicated disease with high rates of morbidity and mortality [2]. Acute pancreatitis can develop due to multiple causes which can be identified in up to 85% of the cases. Some of the most common factors include gallstones, alcohol abuse, drugs, toxins, hypercalcemia and hypertriglyceridemia [3]. In the patient mentioned in this article, all common risk factors previously mentioned were ruled out.
In December 2020, an emergency use authorization has been granted for a SARS-COV-2 vaccine (BNT162b2) developed by Pfizer and BioNTech that became the first mRNA-based vaccine approved for human use against COVID-19 [4]. The rapid development of COVID-19 vaccines with the introduction of emerging technologies such as mRNA based vaccines have raised concerns about possible side effects [5]. Local and systemic reactions were reported after the first and second dose of BNT162b2 vaccine and it included pain at the site of injection, headache, fever, fatigue, nausea, myalgia and arthralgia [6]. Two cases of pancreatitis were reported after the first and second dose of vaccine [7, 8].
Although it is difficult to conclude that the vaccine may be the direct cause of acute pancreatitis, our case was temporally associated with the administration of the BNT162b2 vaccine with absence of any predisposing risk factor, which increased the likelihood of the vaccine as a possible etiology behind the episode of acute pancreatitis.
References
- Chatila AT, Bilal M, Guturu P. Evaluation and management of acute pancreatitis. World J Clin Cases 7 (2019): 1006-1020.
- Gapp J, Chandra S. Acute Pancreatitis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2021).
- Wang G-J, Gao C-F, Wei D, et al. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol 15 (2009): 1427-1430.
- Tumban E. Lead SARS-CoV-2 candidate vaccines: Expectations from phase III trials and recommendations post-vaccine approval. Viruses 13 (2020): 54.
- Alamer E, Alhazmi A, Qasir NA, et al. Side Effects of COVID-19 Pfizer-BioNTech mRNA Vaccine in Children Aged 12-18 Years in Saudi Arabia. Vaccines (Basel) 9 (2021):1297.
- S. Food and Drug Administration. MEETING DATE: Pfizer-BioNTech COVID-19 Vaccine (BNT162, PF-07302048). Vaccines and Related Biological Products Advisory Committee Briefing Document (2020).
- Parkash O, Sharko A, Farooqi A, et al. Acute Pancreatitis: A Possible Side Effect of COVID-19 Vaccine. Cureus 13 (2021): e14741.
- Walter T, Connor S, Stedman C, et al. A case of acute necrotising pancreatitis following the second dose of Pfizer-BioNTech COVID-19 mRNA vaccine. British Journal of Clinical Pharmacology 8 (2022): 1385-1386.
