Accuracy of Ultrasound in Determining Proximal Humeral Epiphyseal Widening in Youth Athletes: A Case Series
Article Information
Scott C Everett1*, Andrew L Alejo1, Blake Boggess2, Emily Reinke2, Cindy Green2, Emily Poehlein2, Benjamin Boswell3,4
1College of Medicine, Northeast Ohio Medical University (NEOMED), Rootstown OH, USA
2Department of Sports Medicine, Duke University, Durham NC, USA
3Department of Sports Medicine, University Hospitals, Cleveland OH, USA
4Department of Emergency Medicine, University Hospitals, Cleveland OH, USA
*Corresponding Author: Scott C Everett, College of Medicine, Northeast Ohio Medical University (NEOMED), Rootstown OH, USA.
Received: 08 May 2023; Accepted: 19 May 2023; Published: 25 May 2023
Citation:
Scott C Everett, Andrew L Alejo, Blake Boggess, Emily Reinke, Cindy Green, Emily Poehlein, Benjamin Boswel. Accuracy of Ultrasound in Determining Proximal Humeral Epiphyseal Widening in Youth Athletes: A Case Series. Journal of Orthopedics and Sports Medicine. 5 (2023): 260-264.
Share at FacebookAbstract
Exposing children to numerous radiographs in order to diagnose various musculoskeletal injuries is not ideal due to the deleterious side effects of ionizing radiation on growth plates. In particular, Little Leaguer’s Shoulder is a common pediatric and adolescent injury that relies mainly on radiographs in order to recognize and treat. Thus, if other imaging modalities without ionizing radiation, such as ultrasound, can be shown to be reliable and accurate in measuring humeral physeal width, it may serve as a better means of identifying these injuries. The purpose of this study was to assess the consistency of two separate physician measures of proximal humeral epiphysis widening in children ages 12-16. Inter-rater and intra-rater reliability of ultrasound measurements of the proximal humeral epiphysis was calculated among twelve patients with open physes. Longitudinal measurements of the epiphyseal plate were obtained in three locations: just distal to the most lateral aspect of the acromion, 2 cm anterior to that line, and 2 cm posterior to that line with the same measurements repeated on the opposite arm. Measurements were then averaged for an overall width. Overall, no statistically significant variation was found when comparing epiphyseal plate width on dominant versus non-dominant arms. Ultrasonographic measurement of proximal humeral epiphyseal width shows narrow variability when used and interpreted by a sports medicine physician.
Keywords
Exposing children to numerous radiographs in order to diagnose various musculoskeletal injuries is not ideal due to the deleterious side effects of ionizing radiation on growth plates. In particular, Little Leaguer’s Shoulder is a common pediatric and adolescent injury that relies mainly on radiographs in order to recognize and treat. Thus, if other imaging modalities without ionizing radiation, such as ultrasound, can be shown to be reliable and accurate in measuring humeral physeal width, it may serve as a better means of identifying these injuries. The purpose of this study was to assess the consistency of two separate physician measures of proximal humeral epiphysis widening in children ages 12-16. Inter-rater and intra-rater reliability of ultrasound measurements of the proximal humeral epiphysis was calculated among twelve patients with open physes. Longitudinal measurements of the epiphyseal plate were obtained in three locations: just distal to the most lateral aspect of the acromion, 2 cm anterior to that line, and 2 cm posterior to that line with the same measurements repeated on the opposite arm. Measurements were then averaged for an overall width. Overall, no statistically significant variation was found when comparing epiphyseal plate width on dominant versus non-dominant arms. Ultrasonographic measurement of proximal humeral epiphyseal width shows narrow variability when used and interpreted by a sports medicine physician.
Sports medicine articles Sports medicine Research articles Sports medicine review articles Sports medicine PubMed articles Sports medicine PubMed Central articles Sports medicine 2023 articles Sports medicine 2024 articles Sports medicine Scopus articles Sports medicine impact factor journals Sports medicine Scopus journals Sports medicine PubMed journals Sports medicine medical journals Sports medicine free journals Sports medicine best journals Sports medicine top journals Sports medicine free medical journals Sports medicine famous journals Sports medicine Google Scholar indexed journals Baseball articles Baseball Research articles Baseball review articles Baseball PubMed articles Baseball PubMed Central articles Baseball 2023 articles Baseball 2024 articles Baseball Scopus articles Baseball impact factor journals Baseball Scopus journals Baseball PubMed journals Baseball medical journals Baseball free journals Baseball best journals Baseball top journals Baseball free medical journals Baseball famous journals Baseball Google Scholar indexed journals Shoulder articles Shoulder Research articles Shoulder review articles Shoulder PubMed articles Shoulder PubMed Central articles Shoulder 2023 articles Shoulder 2024 articles Shoulder Scopus articles Shoulder impact factor journals Shoulder Scopus journals Shoulder PubMed journals Shoulder medical journals Shoulder free journals Shoulder best journals Shoulder top journals Shoulder free medical journals Shoulder famous journals Shoulder Google Scholar indexed journals Tennis players articles Tennis players Research articles Tennis players review articles Tennis players PubMed articles Tennis players PubMed Central articles Tennis players 2023 articles Tennis players 2024 articles Tennis players Scopus articles Tennis players impact factor journals Tennis players Scopus journals Tennis players PubMed journals Tennis players medical journals Tennis players free journals Tennis players best journals Tennis players top journals Tennis players free medical journals Tennis players famous journals Tennis players Google Scholar indexed journals Proximal humerus articles Proximal humerus Research articles Proximal humerus review articles Proximal humerus PubMed articles Proximal humerus PubMed Central articles Proximal humerus 2023 articles Proximal humerus 2024 articles Proximal humerus Scopus articles Proximal humerus impact factor journals Proximal humerus Scopus journals Proximal humerus PubMed journals Proximal humerus medical journals Proximal humerus free journals Proximal humerus best journals Proximal humerus top journals Proximal humerus free medical journals Proximal humerus famous journals Proximal humerus Google Scholar indexed journals Bilateral arms articles Bilateral arms Research articles Bilateral arms review articles Bilateral arms PubMed articles Bilateral arms PubMed Central articles Bilateral arms 2023 articles Bilateral arms 2024 articles Bilateral arms Scopus articles Bilateral arms impact factor journals Bilateral arms Scopus journals Bilateral arms PubMed journals Bilateral arms medical journals Bilateral arms free journals Bilateral arms best journals Bilateral arms top journals Bilateral arms free medical journals Bilateral arms famous journals Bilateral arms Google Scholar indexed journals Soccer player articles Soccer player Research articles Soccer player review articles Soccer player PubMed articles Soccer player PubMed Central articles Soccer player 2023 articles Soccer player 2024 articles Soccer player Scopus articles Soccer player impact factor journals Soccer player Scopus journals Soccer player PubMed journals Soccer player medical journals Soccer player free journals Soccer player best journals Soccer player top journals Soccer player free medical journals Soccer player famous journals Soccer player Google Scholar indexed journals Physeal fragmentation articles Physeal fragmentation Research articles Physeal fragmentation review articles Physeal fragmentation PubMed articles Physeal fragmentation PubMed Central articles Physeal fragmentation 2023 articles Physeal fragmentation 2024 articles Physeal fragmentation Scopus articles Physeal fragmentation impact factor journals Physeal fragmentation Scopus journals Physeal fragmentation PubMed journals Physeal fragmentation medical journals Physeal fragmentation free journals Physeal fragmentation best journals Physeal fragmentation top journals Physeal fragmentation free medical journals Physeal fragmentation famous journals Physeal fragmentation Google Scholar indexed journals Cheerleader articles Cheerleader Research articles Cheerleader review articles Cheerleader PubMed articles Cheerleader PubMed Central articles Cheerleader 2023 articles Cheerleader 2024 articles Cheerleader Scopus articles Cheerleader impact factor journals Cheerleader Scopus journals Cheerleader PubMed journals Cheerleader medical journals Cheerleader free journals Cheerleader best journals Cheerleader top journals Cheerleader free medical journals Cheerleader famous journals Cheerleader Google Scholar indexed journals Swimmer articles Swimmer Research articles Swimmer review articles Swimmer PubMed articles Swimmer PubMed Central articles Swimmer 2023 articles Swimmer 2024 articles Swimmer Scopus articles Swimmer impact factor journals Swimmer Scopus journals Swimmer PubMed journals Swimmer medical journals Swimmer free journals Swimmer best journals Swimmer top journals Swimmer free medical journals Swimmer famous journals Swimmer Google Scholar indexed journals Non-athlete articles Non-athlete Research articles Non-athlete review articles Non-athlete PubMed articles Non-athlete PubMed Central articles Non-athlete 2023 articles Non-athlete 2024 articles Non-athlete Scopus articles Non-athlete impact factor journals Non-athlete Scopus journals Non-athlete PubMed journals Non-athlete medical journals Non-athlete free journals Non-athlete best journals Non-athlete top journals Non-athlete free medical journals Non-athlete famous journals Non-athlete Google Scholar indexed journals Juvenile males articles Juvenile males Research articles Juvenile males review articles Juvenile males PubMed articles Juvenile males PubMed Central articles Juvenile males 2023 articles Juvenile males 2024 articles Juvenile males Scopus articles Juvenile males impact factor journals Juvenile males Scopus journals Juvenile males PubMed journals Juvenile males medical journals Juvenile males free journals Juvenile males best journals Juvenile males top journals Juvenile males free medical journals Juvenile males famous journals Juvenile males Google Scholar indexed journals Forearm fracture articles Forearm fracture Research articles Forearm fracture review articles Forearm fracture PubMed articles Forearm fracture PubMed Central articles Forearm fracture 2023 articles Forearm fracture 2024 articles Forearm fracture Scopus articles Forearm fracture impact factor journals Forearm fracture Scopus journals Forearm fracture PubMed journals Forearm fracture medical journals Forearm fracture free journals Forearm fracture best journals Forearm fracture top journals Forearm fracture free medical journals Forearm fracture famous journals Forearm fracture Google Scholar indexed journals Bias articles Bias Research articles Bias review articles Bias PubMed articles Bias PubMed Central articles Bias 2023 articles Bias 2024 articles Bias Scopus articles Bias impact factor journals Bias Scopus journals Bias PubMed journals Bias medical journals Bias free journals Bias best journals Bias top journals Bias free medical journals Bias famous journals Bias Google Scholar indexed journals Leaguer’s shoulder articles Leaguer’s shoulder Research articles Leaguer’s shoulder review articles Leaguer’s shoulder PubMed articles Leaguer’s shoulder PubMed Central articles Leaguer’s shoulder 2023 articles Leaguer’s shoulder 2024 articles Leaguer’s shoulder Scopus articles Leaguer’s shoulder impact factor journals Leaguer’s shoulder Scopus journals Leaguer’s shoulder PubMed journals Leaguer’s shoulder medical journals Leaguer’s shoulder free journals Leaguer’s shoulder best journals Leaguer’s shoulder top journals Leaguer’s shoulder free medical journals Leaguer’s shoulder famous journals Leaguer’s shoulder Google Scholar indexed journals
Article Details
Abbreviations:
BA: Bland-Altman; CI: Confidence Interval; LOA: Limits of Agreement; SD: Standard Deviation; US: Ultrasound
Introduction
Every year, millions of children play Little League baseball in the United States. Little Leaguer’s Shoulder is a common injury that occurs most frequently in male overhead pitchers; however, it has also been observed in female overhead pitchers, youth catchers and tennis players. Little Leaguer’s Shoulder is a common overuse injury occurring in young baseball pitchers resulting in epiphysiolysis of the proximal humerus. This injury typically appears between the ages of 11-16 years old and is increasing as rising numbers of youth athletes are developing sport specialization at a younger age. Currently, the diagnosis of Little Leaguer’s Shoulder is made by comparing proximal humeral epiphyseal plate widening of the affected arm versus the unaffected arm by using ionizing plain film radiography [1-3].
Various studies that compared ultrasound (US) to x-ray in pediatric forearm fractures found that ultrasound was cheaper, faster, and less painful for patients in addition to avoiding the use of ionizing radiation [4]. Sensitivity for ultrasound, compared to an x-ray gold standard, was 85% for metaphyseal humeral fractures in pediatric patients with a 75% negative predictive value [5]. MRI on the other hand, has also been shown to be helpful in diagnosing injuries to the growth plate that was not found on radiographs and allows the physician to follow the patient’s progress during their recovery without the use of ionizing radiation, however it is often costly to the patient [6].
The most common ultrasound finding in juvenile males diagnosed with Little Leaguer’s Shoulder was epiphyseal widening [7]. Other findings on sonography of the dominant shoulder displayed were physeal irregularities (45%), physeal fragmentation (21%), periosteal thickening (36%), and physeal widening (83%) [8]. Given the advantages of ultrasonography and the likelihood of success, we aimed to test the ability to consistently measure proximal humeral epiphyseal width in children ages 12-16 by using point of care US to see if it might be possible to use US in place of radiographs.
2. Methods
The enrollment phase of the study occurred during a 2-month period at an outpatient sports medicine clinic. During that time, subjects were screened during their evaluations for specific inclusion criteria. These criteria include subjects between ages of 12-16, radiographs within three weeks demonstrating an open physis in any extremity, and the availability of a parent or guardian to give legally effective consent. Exclusion criteria were findings of a proximal humerus fracture on radiographs, closed physeal plates, history of genetic abnormality, history of abnormal development, or inability to provide legally effective consent.
Once patients were enrolled, two primary care sports medicine providers performed US measurements of bilateral arms. Within a 10-week period, subjects returned to obtain another round of measurements by both physicians. Each physician was blinded from all previous measurements to prevent bias, and each measurement round was performed by the same physician separated by at least five days.
Measurements were obtained by placing the US probe on the lateral aspect of the acromion and scanning directly inferior until a long axis view of the humeral epiphyseal growth plate was obtained. Measurements were obtained in the same fashion: 2 cm anterior and posterior to the initial location, obtaining 3 measurements for an average measurement of the humeral epiphyseal plate. These measurements were then repeated on the opposite arm. All measurements were obtained using the linear probe on the same ultrasound machine (Sonosite X-Porte). This method was used to limit potential measurement differences among various machines.
Descriptive statistics were calculated to describe baseline demographic and clinical characteristics of patients undergoing ultrasound of bilateral arms. A paired t-test was used to compare the average dominant and non-dominant arm measurements from the first round of testing. Continuous variables were presented using the mean and standard deviation (SD) or median with 25th and 75th percentiles (Q1-Q3) as appropriate based on variable distribution. Categorical variables were summarized with frequency counts and percentages. Width measurements of the growth plates taken from ultrasound were measured in triplicate on both the right and left side with the average value used for analysis. A linear mixed-effects regression model was used to analyze the average width using both the patient undergoing ultrasound and physician reading ultrasound as the fixed effects and random effects dependent on the model (inter- or intra-rater) to account for the correlation between measurements conducted on the same patient and by the same physician.
Limits of agreement (LOA) and their associated 95% confidence interval (CI) were estimated in order to provide an interval within which 95% of the differences between measurements were expected to be found using the Bland-Altman (BA) method. This method was used for both inter-rater (Physician 1 vs. Physician 2) and intra-rater (Physician 1 vs. Physician 1 and Physician 2 vs. Physician 2) agreement. A BA plot was constructed to visualize both the inter- and intra-rater agreement. The acceptability of these limits of agreement was assessed based on clinician expertise. Analyses were performed using R (Hmisc, BlandAltmanLeh, and Blandr) and SAS version 9.4 (SAS Institute, Inc., Cary, NC).
3. Results
Twelve patients were enrolled in our study after parental consent and patient assent were obtained. Nine patients completed all four rounds of measurements. Two males and one female did not complete more than the first round of measurements. Patient ages ranged from 12 to 15 years, with an average age of 14 +/- 1 year. Seven patients (58.3%) were male and 11 (91.7%) were right arm dominant. Of the patients enrolled, five played baseball, three were gymnasts, one each were a soccer player, cheerleader, swimmer, or non-athlete. There were four patients enrolled who played multiple sports.
Measurements were taken using a static image. Locations used for measurements included the most lateral aspect of the epiphyseal plate extending from the proximal edge (marked by white crosses) to the distal edge (Figure 1). Overall, there was no statistically significant variation when comparing average epiphyseal plate width measured in the first round on dominant versus non-dominant arms (p=0.600) (Figure 2A). We observed what is likely to be the expected negative relationship between physeal width and subject age, but due to small sample size, this could not be statistically described with any significance (Figure 2B).
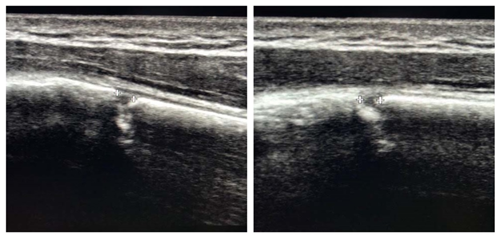
Figure 1: Ultrasonographic measurements obtained in long axis using a linear probe.
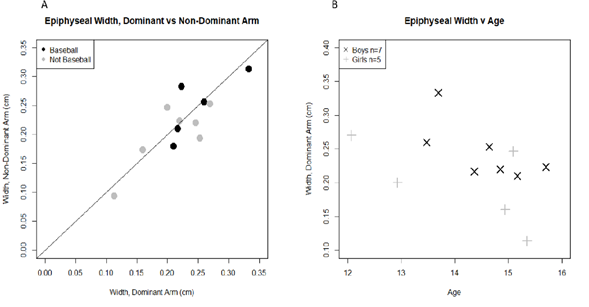
Figure 2: Graphical analysis of average physeal width.
Average physeal width measurement in cm in the dominant vs nondominant arm in baseball (dark circles) and non-baseball players (light circles) at the first testing round (A). Dominant arm average physeal width in cm vs age in boys (black x) and girls (grey +) (B). The diagonal line represents x=y.
Raw comparisons between the two physicians for trial one and comparing between trial one and two for each physician was calculated (Figure 3). These comparisons across the identity line, demonstrate similar tight clustering for intra-rater measurements and looser cluster for inter-rater comparisons. To mathematically describe these comparisons, a Bland-Altman analysis was used (Figure 4). The mean inter-rater difference (bias) between Physician 1 and Physician 2 (Figure 4A) was 0.023 ± 0.045 cm, with a lower LOA of -0.066 cm (95% CI: -0.105 to -0.026) and an upper LOA of 0.112 cm (95% CI: 0.073 to 0.151). The difference between the mean bias and upper- and lower-most 95% CI of the LOA was +/- 0.089 cm. The mean intra-rater difference for Physician 1 (Figure 4B) was 0.018 ± 0.032 cm, with a lower LOA of -0.044 cm (95% CI: -0.072 to 0.017) and an upper LOA of 0.080 cm (95% CI: 0.052 to 0.107). The difference between the mean bias and upper- and lower-most 95% CI of the LOA was +/- 0.062 cm. The mean intrarater difference for Physician 2 (Fig 4C) was 0.010 ± 0.032 cm, with a lower LOA of -0.053 cm (95% CI: -0.082 to -0.025) and an upper LOA of 0.074 cm (95% CI: 0.046 to 0.102). The difference between the mean bias and upper- and lower-most 95% CI of the LOA was +/- 0.064 cm.
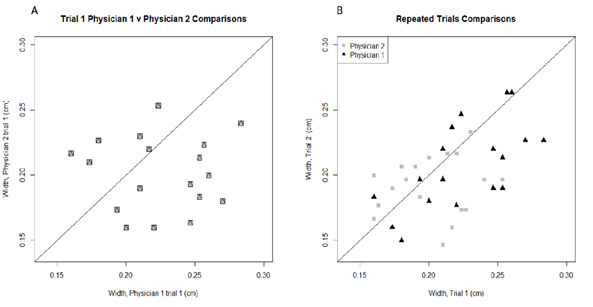
Figure 3: Graphical analysis of physeal width between physicians.
Average physeal width in cm comparisons for Physician 1 vs. Physician 2 on their first trial (A) and Physician 1 trial 1 vs. trial 2 (dark triangles) and Physician 2 trial 1 vs. trial 2 (grey squares) (B). The diagonal line in both graphs represents x=y.
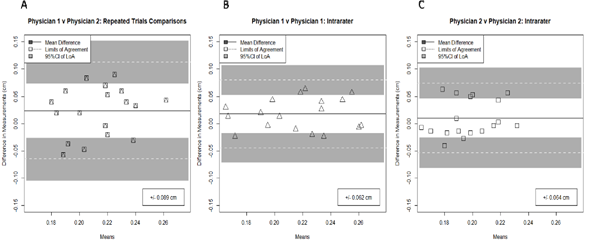
Figure 4: Graphical analysis of inter-rater agreement among physicians.
Inter-rater agreement comparing Physician 1 to Physician 2 (data points for trial 1 only shown) (A), intra-rater agreement for Physician 1 during two trials (B), and intra-rater agreement for Physician 2 during two trials (C) is displayed using a Bland-Altman graph. The value in the boxes in the lower right of each graph represents the distance between the mean difference (bias) and the upper- and lower-most 95% confidence interval for the limits of agreement.
4. Discussion
Our study concluded that the ultrasound measurement of proximal humeral epiphyseal width is promising when used and interpreted by a physician, showing good intra-rater reliability. However, there is a larger variation when two separate physicians are measuring the humeral epiphyseal width, which limits inter-rater reliability. This is similar to what was found in a systematic review of ultrasound measurement of acromiohumeral distance done by McCreesh et al. [9]. A statistically significant difference was not found in epiphyseal width on dominant versus nondominant arms in asymptomatic patients, including both overhead and non-overhead athletes. This is in contrast to a report which found two of ten healthy juvenile males to have proximal humeral widening on radiograph despite the absence of any symptoms [10].
A systematic review by Douma-den Hamer D et al. [11] examined the diagnostic efficacy of using US in metaphyseal forearm fractures in children. They concluded that US carries high sensitivity and specificity. Sensitivity of ultrasound in forearm fracture diagnosis in the study was 97%, while the specificity was 95% [11]. This study also concluded that utilization of ultrasound can be faster, less painful, and more cost-effective, which was in line with our findings. Chen et al. [12] reviewed diagnosing and guiding reduction of forearm fractures in children using bedside ultrasound and found it was a reliable and convenient method to diagnose and reduce these fractures in the emergency room. Their initial success rate of ultrasound-guided reduction was 92%. Ultrasound application has been growing in the emergency department and its use has been advancing to assist physicians throughout various procedures. Decreasing ionizing radiation exposure to pediatric patients by using ultrasound in the previously mentioned studies has been shown to be a good substitute for radiographs. Our study adds onto the available data on using US in order to diagnose Little Leaguer’s Shoulder.
Limitations to this study included a small sample size, selection bias, patients lost to follow-up, and potential for user bias. Additionally, ultrasound in this setting has a potential for user error, absence of radiology comparison, no standard measuring system when crossing imaging modalities, variation in measurements, and potential to miss alternative pathology.
5. Conclusion
Overall, this study demonstrated the potential use of diagnostic ultrasonography for adolescents suffering from Little Leaguer’s Shoulder and/or those who have other epiphyseal stress injuries. Currently, radiographs are the most commonly used imaging modality for the diagnosis of epiphyseal widening, and there is no protocol for the use of US as an alternative imaging technique currently. However, the results of this study demonstrate that ultrasound should be considered as a reliable alternative to imaging as a way of moving away from ionizing radiation in pediatrics and adolescents.
Conflicts of Interest:
The authors have no conflicts of interest to declare.
References
- Osbahr DC, Kim HJ, Dugas JR. Little league shoulder. Curr Opin Pediatr 22 (2010): 35-40.
- Hale CJ. Little Leaguer’s Shoulder. A Report of 23 cases. Am J Sports Med 4 (1998): 575-580.
- Ku JH, Cho HL, Jin HK, et al. Ultrasonographic findings of Little Leaguer’s Shoulder. The Korean Journal of Sports Medicine 34 (2016): 132-138.
- Kanematsu Y, Matsuura T, Kashiwaguchi S, et al. Radiographic follow-up study of Little Leaguer’s Shoulder. Skeletal Radiol 44 (2015): 73-76.
- Akinmade A, Ikem I, Ayoola O, et al. Comparing ultrasonography with plain radiography in the diagnosis of paediatric long-bone fractures. Int Orthop 43 (2019): 1143-1153.
- Song JC, Lazarus ML, Song AP. MRI findings in Little Leaguer’s Shoulder. Skeletal Radiol 35 (2006): 107-179.
- Heyworth BE, Kramer DE, Martin DJ, et al. Trends in the Presentation, Management, and Outcomes of Little League Shoulder. Am J Sports Med 44 (2016): 1431-1438.
- Katzer C, Wasem J, Eckert K, et al. Ultrasound in the Diagnostics of Metaphyseal Forearm Fractures in Children: A Systematic Review and Cost Calculation. Pediatr Emerg Care 32 (2016): 401-407.
- McCreesh KM, Crotty JM, Lewis JS. Acromiohumeral distance measurement in rotator cuff tendinopathy: is there a reliable, clinically applicable method? A systematic review. Br J Sports Med 49 (2015): 298-305.
- Akgul S, Dilickik U, Kanbur NO, et al. Proximal humeral physeal widening: little leaguer’s shoulder or a variation of normal development. Turk J Pediatr 53 (2011): 711-714.
- Douma-den Hamer D, Blanker MH, Edens MA, et al. Ultrasound for Distal Forearm Fracture: A Systematic Review and Diagnostic Meta-Analysis. PLoS One 11 (2016): e0155659.
- Chen L, Kim Y, Moore CL. Diagnosis and guided reduction of forearm fractures in children using bedside ultrasound. Pediatr Emerg Care 23 (2007): 528-531.
