A Rare Case of Postoperative Acanthamoeba Endophthalmites after Uneventful Cataract Surgery
Article Information
Antonio Berarducci1*, Martina Colasante1, Mariateresa Laborante2, Antonio Laborante1
1Eye Clinic, Head and Neck Department, IRCCS Casa Sollievo della Sofferenza Hospital, 71017 San Giovanni Rotondo, Foggia, Italy
2Faculty of Medicine and Surgery, UCBM Campus Bio-Medico University of Rome, 21 Via Álvaro del Portillo
00128 Rome, Italy
*Corresponding Author: Antonio Berarducci, Eye Unit, IRCCS Casa Sollievo della Sofferenza Hospital, 71017 San Giovanni Rotondo, Foggia, Italy.
Received: 03 May 2023; Accepted: 12 May 2023; Published: 21 July 2023
Citation: Antonio Berarducci, Martina Colasante, Mariateresa Laborante, Antonio Laborante. A Rare Case of Postoperative Acanthamoeba Endophthalmites after Uneventful Cataract Surgery. Archives of Clinical and Medical Case Reports. 7 (2023): 318-321.
Share at FacebookAbstract
Purpose: To report a rare case of postoperative Acanthamoeba endophthalmites after uncomplicated cataract surgery in an otherwise healthy patient.
Case Description: A patient with preexisting glaucoma and CNV in both eyes underwent uneventful cataract surgery (PHACO + IOL + intracamerular cefuroxima) in his right eye. Nine days after surgery, patient presented in eye casualty complaining drop in vision, eye pain and violent diarrhoea. Pars plana vitrectomy was performed and Acanthamoeba protozoa was isolated. Empirical therapy including intravenous voriconazole 2, 5 mg twice a day, a single shot of intravitreal voriconazole 1% in 0,1 ml and topical chlorhexidine 0,02% topical was started immediately.
Conclusions: sixteen days from the initial symptoms a complete resolution of the endophthalmites was reported as well as an improvement in the visual acuity. Physicians should be aware of Acanthamoeba infection as a cause of eye infection in any patient, not just contact lens wearers; intravitreal and systemic administration of voriconazole can be successfully used to treat Acanthamoeba endophthalmitis
Keywords
Acanthamoeba; Cataract; Endophthalmitis; Vitrectomy
Article Details
Abbreviations
CNV: Choroidal Neovascularization; DALK: Deep Anterior Lamellar Keratoplasty
1. Introduction
The increased number of eye surgery worldwide and the widespread use of contact lenses have led to an increase in the incidence of severe ocular infections sometimes resulting in irreversible loss of vision. Infectious endophthalmitis following intraocular surgery is a complication that can cause severe visual loss or loss of the eye. Microbiological diagnosis is necessary when the lesions are non-specific, recurrent or unresponsive to antibiotic therapy, but is hampered by the difficulty of analysing limited sample volumes containing small inocula [1]. The categorisation of the event that led to intraocular infection will help the clinician to predict the infectious agent and begin appropriate therapy [2] but, despite this, Acanthamoeba diagnosis is often a clinical challenge. In most cases of corneal involvement, it is primarily confused with herpes keratitis and supra or co-infection with bacteria or fungi can lead to a delayed diagnosis and initiation of treatment [3]. Not many cases of Acanthamoeba in the anterior chamber have been described in literature, therefore in the presence of a negative tap for bacteria or fungi, Acanthamoeba should always be considered as a potential cause of infection.
2. Case Description
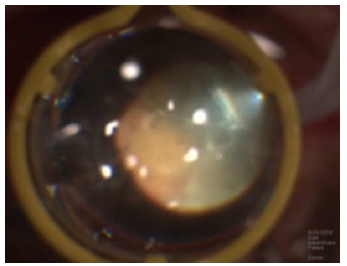
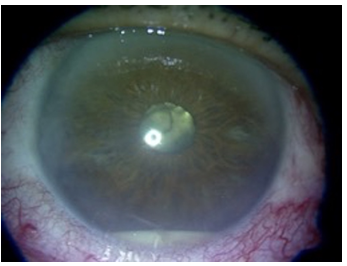
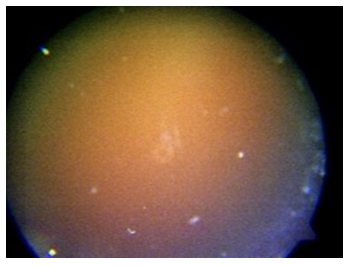
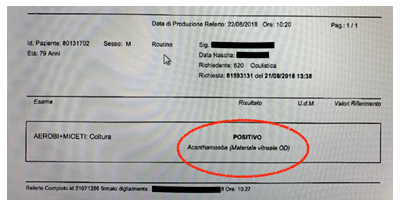
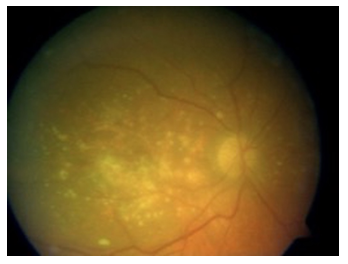
We describe the clinical course of a seventy-nine years old patient, retired fishmonger, with pre-existing glaucoma and longstanding and stable CNV in both eyes but no other general health issues. Despite having had an uncomplicated PHACO/IOL procedure in his right eye, he presented in eye casualty complaining eye pain, diarrhoea and loss in vision nine days after the cataract surgery and a few days after having attended an exhibition of fresh seafood from lake. Visual acuity was counting finger in his affected eye and the anterior segment assessment consisted with conjunctival hyperaemia, fibrin and hypopyon in the anterior chamber as well as corneal endothelial precipitates (no sign of corneal infiltrates, ulcer or erosion was seen). Retinal assessment was not carried out because of the obscured fundus view (Figure 1); ultrasound B-scan examination confirmed vitreitis with severe vitreous debris. Pars plana vitrectomy followed by vancomycin 1 mg/0,1 ml intravitreal injection was performed on emergency basis (intraoperative ceftazidime intravitreal injection was not done due to hospital shortage); vitreous sample was sent to the laboratories for microbiological purposes. Despite the emergency procedure, hypopyon (Figure 2) as well as severe vitreitis (Figure 3) persisted postoperatively with a positive culture for Acanthamoeba protozoa (Figure 4). Diagnosis was made by directly seen the Acanthamoeba trophozoites under inverted phase contrast microscope and previous stain with haematoxylin and eosin; molecular tests to perform differential diagnosis between the different Acanthamoeba genotypes was not carried out.
Tests to exclude immune depression, stool and urine contamination were normal; only CRP seemed to be slightly increased up to 1, 18 mg/L. An empirical treatment consisting with intravenous voriconazole 2, 5 mg twice a day, intravitreal voriconazole 1% in 0,1 ml in a single shot and topical chlorhexidine 0,02% was immediately started. Seven days after activating protocol, patient was complaining severe hallucinations and MRI scan and electroencephalography of the brain were performed to exclude intracranial protozoa localizations. The tests confirmed the hallucination to be a voriconazole side effect and sulfamethoxazole 400 mg/trimethoprim 80 mg (Bactrim) three times per day was introduced instead. Sixteen days from the initial symptoms, a complete endophthalmitis resolution (Figure 5) was documented as well as an improvement in the visual acuity up to 1,1 logMAR. No sign of reoccurrence of infection was reported at 12 months’ time follow up.
3. Discussion and Conclusions
The genus Acanthamoeba is a group of about 25 species comprising 18 genotypes (T1-T18) that has a worldwide distribution causing rare, but severe, infections of the eye, skin, lungs, and central nervous system (CNS). Studies on sequence analysis demonstrates that T4 is the predominant genotype in non-AK infections, including those in brain, cerebrospinal fluid, nasal passages, skin, lung and rare genotypes (T1, T10, and T12) have been isolated from brain infections [4]. However, even if variations in the pathogenicity of different Acanthamoeba strains have been recognized in various studies, the relevance of these results to human disease is unclear [5] and many people will be exposed to Acanthamoeba during their lifetime, but very few will become sick from this exposure.
The structure of the human eye as well as exposure of the eye directly to the environment renders it vulnerable to a number of rare infectious diseases caused by fungi and parasites; sometime infections arise following bloodborne carriage of the microorganism to the eye or adjacent structures [6]. Endophthalmitis is a rare and severe form of ocular inflammation due to infection of the intraocular cavity that can lead to irreversible visual loss; early diagnosis and proper treatment are key points to saving the eye and possibly the life of the patient. The prognosis is usually poor even with prompt diagnosis, and laboratory examinations are important adjuncts, especially in immunocompromised patients [7]. A recent study conducted in 2019 showed that the distribution of infectious agents for endophthalmitis are coagulase-negative Staphylococcus in 54% of cases, Streptococcus spp. in 21%, S. aureus in 10%, other gram-positives in 8% and gram-negatives 7% of cases [8]. Acanthamoeba protozoa is involved in the 5.2% of keratitis cases [8] where infection is usually initiated by Acanthamoeba-contaminated contact lenses and produces chronic smouldering keratitis, very rarely scleritis, exquisite pain and ulceration of the ocular surface [9]. Pars plana vitrectomy is frequently performed regardless of the presenting vision in eyes with endophthalmitis after cataract surgery and intravitreal injections [10], but in Acanthamoeba infection presenting initially as keratitis, followed by sclerokeratitis and finally histopathology-confirmed endophthalmitis, eradication of organisms may not be possible despite persistent medical and surgical intervention [11]. If from one side, literature suggests therapeutic DALK as a possible new approach to eradicate Acanthamoeba active infection poorly responsive to medical treatment with significant ulcer in the optical zone and no sign of vitreous involvement [12], to the other side, a more aggressive treatment including intracameral voriconazole injections, oral azithromycin, fluconazole, flucytosine, topical and systemic antiamebic medications has been described in cases of diffuse intraocular involvement in order to decreased the inflammation but with uncertain results in terms of infection control [13, 14]. Being the Acanthamoeba an ubiquitous, free-living, microscopic amebae found worldwide in water and soil [4], our suspect is that our patient, retired fishmonger, may have been in contact with contaminated water during a local fresh fish fair on the Varano Lake (the largest one in southern Italy), immediately after having had his cataract surgery procedure done.
Our case report suggests that a full pars plana vitrectomy associated with intravenous and intravitreal voriconazole as well as topical chlorhexidine may lead to a complete resolution of the Acanthamoeba endophthalmitis; in cases of voriconazole side effects, sulfamethoxazole 400 mg/trimethoprim 80 mg (Bactrim) can be used instead. Because of the absence of keratitis and the difficulty in recruiting others specific drugs on urgent basis, we did not consider different molecules such as propamidine isotionate or polyhexanide. In addition, an interesting comparative study demonstrated that Voriconazole eye drops could be used against AK as a first-line treatment or in combination and moxifloxacin eyedrops as adjuvant in order to prevent encystation of the amoeba which often complicates infection resolution. In addition, moxifloxacin seems to be effective in preventing secondary bacterial infections [15] and might be considered in unresponsive or recurrent cases.
Even if fulminant endophthalmitis associated with atypical ring infiltrate has been already described after ocular surgery in immunocompetent individual with no significant preoperative ophthalmic history [16], our report, which is the first of its kind, emphasizes the fact that endophthalmitis can also occur after ocular surgery in healthy patients, with no other sign of corneal involvement.
Even if confirmation of Acanthamoeba infection is classically identified by microscopic examination and culture of corneal tissue and contact lenses or equipment using tap water agar plate overlain with bacteria as a food source for the amebae, unfortunately our laboratory is not prepared to perform genotypic identification of pathogenic isolates and this may represents a limit in this case report. To conclude, not many cases of Acanthamoeba in the anterior chamber have been described in literature, therefore in the presence of a negative tap for bacteria or fungi, Acanthamoeba should always be considered as a potential cause of infection.
Availability of Data and Materials
All the information supporting our conclusions and relevant references are included in the manuscript. There are no datasets related to this case report. The manuscript has not been presented at any meeting/conference.
Conflicts of Interests
The authors declare they have no competing interests.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying additional files.
Funding Statements
No funding received.
Conflicts of Interests
The authors declare they have no competing interests.
References
- López-Cerero L, Etxebarria J, Mensa J. Microbiological Diagnosis of Ocular Infections. Enferm Infecc Microbiol Clin 27 (2009): 531-535.
- Das T, Dogra MR, Gopal L, et al. Postsurgical Endophthalmitis: Diagnosis and Management. Indian J Ophthalmol 43 (1995): 103-116.
- Pascha J, Frings A, Walochnik J, et al. Acanthamoeba Endophthalmitis-A Case Report. Ophthalmologe (2019).
- Booton GC, Visvesvara GS, Byers TJ, et al. Identification and Distribution of Acanthamoeba Species Genotypes Associated with Nonkeratitis Infections. J Clin Microbiol 43 (2005): 1689-1693.
- DeJonckheere J. Growth characteristics, cytopathic effect in cell culture, and virulence in mice of 36 type strains belonging to 19 different Acanthamoeba spp. Appl. Environ. Microbiol 39 (1980): 681-685.
- Klotz SA, Penn CC, Negvesky GJ, et al. Fungal and Parasitic Infections of the Eye. Clin Microbiol Rev 13 (2000): 662-685.
- Sheu SJ. Endophthalmitis. Korean J Ophthalmol 31 (2017): 283-289.
- Kowalski RP, Nayyar SV, Romanowski EG, et al. The Prevalence of Bacteria, Fungi, Viruses, and Acanthamoeba from 3,004 Cases of Keratitis, Endophthalmitis, and Conjunctivitis. Eye Contact Lens (2019).
- Clarke DW, Niederkorn JY. The Pathophysiology of Acanthamoeba Keratitis. Trends Parasitol 22 (2006): 175-180.
- Soliman MK, Gini G, Kuhn F, et al. European Vitreo-Retinal Society Endophthalmitis Study Group. International Practice Patterns for the Management of Acute Postsurgical and Postintravitreal Injection Endophthalmitis: European Vitreo-Retinal Society Endophthalmitis Study Report 1. Ophthalmol Retina 019 (2019): 461-467.
- Mammo Z, Almeida DR, Cunningham MA, et al. Acanthamoeba endophthalmites after recurrent keratitis and nodular scleritis. Retin Cases Brief Rep 11 (2017): 180-182.
- Sarnicola E, Sarnicola C, Sabatino F, et al. Early Deep Anterior Lamellar Keratoplasty (DALK) for Acanthamoeba Keratitis Poorly Responsive to Medical Treatment. Cornea 35 (2016): 1-5.
- Heffler KF, Eckhardt TJ, Reboli AC, et al. Acanthamoeba Endophthalmitis in Acquired Immunodeficiency Syndrome. Am J Ophthalmol 122 (1996): 584-586.
- Kutner A, Aldrich M, Patel S, et al. Acanthamoeba Endophthalmitis during Treatment for Cutaneous Disease in a Renal Transplant Patient. Transpl Infect Dis 20 (2018): e12843.
- Martín-Navarro CM, López-Arencibia A, Arnalich-Montiel F, et al. Evaluation of the in Vitro Activity of Commercially Available Moxifloxacin and Voriconazole Eye-Drops Against Clinical Strains of Acanthamoeba. Graefes Arch Clin Exp Ophthalmol 251 (2013): 2111-2117.
- Raghavan A, Veerappan S, Rangarajan V, et al. Fulminant Acanthamoeba Endophthalmitis After Cataract Surgery-A Case Report. Cornea (2020).