A Prospective Study on the Reliability of First-Trimester Ultrasound in Identifying the Gestational Sac Implantation Site
Article Information
Ran Svirsky MD1, 4,*, Omer Moore MD2,4, Noam Smorgick MD2,4, Uri Rozovski MD3,4, Ariel Zimerman MD2,4, Ron Maymon MD2,4
1 Division of Obstetrics and Gynecology, Genetic Unit Samson Assuta Ashdod medical center, Ashdod , Israel
2 Department of Obstetrics and Gynecology, The Yitzhak Shamir Medical Center (formerly Assaf Harofeh Medical Center), Zerifin, Israel
3 Institute of Hematology, Davidoff Cancer Center, Beilinson Hospital, Petach, Tikva, Israel
4 Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
*Corresponding Author: Ran Svirsky, MD, Division of Obstetrics and Gynecology, Genetic Unit Samson Assuta Ashdod medical center, Ashdod, Israel.
Received: 20 February 2023; Accepted: 27 February 2023; Published: 03 March 2023
Citation: Ran Svirsky, Omer Moore, Noam Smorgick, Uri Rozovski, Ariel Zimerman, Ron Maymon. A prospective study on the reliability of first-trimester ultrasound in identifying the gestational sac implantation site. Obstetrics and Gynecology Research. 6 (2023): 84-87
Share at FacebookAbstract
Objectives:
Normal and abnormal implantation of the gestational sac may affect obstetrical outcomes. We sought to evaluate whether ultrasound can correctly identify the first-trimester gestational sac implantation wall compared to diagnostic hysteroscopy.
Methods:
Consecutive women diagnosed with first-trimester pregnancy loss who opted for surgical termination of pregnancy were prospectively recruited to the study. Pre-operatively, an ultrasound scan was performed to assess for the gestational sac implantation wall. Subsequently, the surgical procedure of diagnostic hysteroscopy combined with suction and curettage was performed. The sonographers were blinded to the hysteroscopy results. The gestational sac implantation wall was determined and compared between the two modalities.
Results:
Twenty-three women were included in the study. The median gestational age 9 (range: 6 to 13) weeks, and the median crown-rump length was 7 (range 6-9) mm. In one case, the implantation site was determined only by the U.S. In the remaining, the U.S. and hysteroscopy gestational sac location were identical (21/22, 95%). Thus, the correlation between the sonographic and hysteroscopy findings was 0.96.
Conclusion:
Ultrasound is a reliable method for the detection of the early gestational sac implantation site.
Keywords
Gestational sac; implantation; ultrasound scan; hysteroscopy; first trimester
Gestational sac articles Gestational sac Research articles Gestational sac review articles Gestational sac PubMed articles Gestational sac PubMed Central articles Gestational sac 2023 articles Gestational sac 2024 articles Gestational sac Scopus articles Gestational sac impact factor journals Gestational sac Scopus journals Gestational sac PubMed journals Gestational sac medical journals Gestational sac free journals Gestational sac best journals Gestational sac top journals Gestational sac free medical journals Gestational sac famous journals Gestational sac Google Scholar indexed journals implantation articles implantation Research articles implantation review articles implantation PubMed articles implantation PubMed Central articles implantation 2023 articles implantation 2024 articles implantation Scopus articles implantation impact factor journals implantation Scopus journals implantation PubMed journals implantation medical journals implantation free journals implantation best journals implantation top journals implantation free medical journals implantation famous journals implantation Google Scholar indexed journals ultrasound scan articles ultrasound scan Research articles ultrasound scan review articles ultrasound scan PubMed articles ultrasound scan PubMed Central articles ultrasound scan 2023 articles ultrasound scan 2024 articles ultrasound scan Scopus articles ultrasound scan impact factor journals ultrasound scan Scopus journals ultrasound scan PubMed journals ultrasound scan medical journals ultrasound scan free journals ultrasound scan best journals ultrasound scan top journals ultrasound scan free medical journals ultrasound scan famous journals ultrasound scan Google Scholar indexed journals hysteroscopy articles hysteroscopy Research articles hysteroscopy review articles hysteroscopy PubMed articles hysteroscopy PubMed Central articles hysteroscopy 2023 articles hysteroscopy 2024 articles hysteroscopy Scopus articles hysteroscopy impact factor journals hysteroscopy Scopus journals hysteroscopy PubMed journals hysteroscopy medical journals hysteroscopy free journals hysteroscopy best journals hysteroscopy top journals hysteroscopy free medical journals hysteroscopy famous journals hysteroscopy Google Scholar indexed journals first trimester articles first trimester Research articles first trimester review articles first trimester PubMed articles first trimester PubMed Central articles first trimester 2023 articles first trimester 2024 articles first trimester Scopus articles first trimester impact factor journals first trimester Scopus journals first trimester PubMed journals first trimester medical journals first trimester free journals first trimester best journals first trimester top journals first trimester free medical journals first trimester famous journals first trimester Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals embryo's viability articles embryo's viability Research articles embryo's viability review articles embryo's viability PubMed articles embryo's viability PubMed Central articles embryo's viability 2023 articles embryo's viability 2024 articles embryo's viability Scopus articles embryo's viability impact factor journals embryo's viability Scopus journals embryo's viability PubMed journals embryo's viability medical journals embryo's viability free journals embryo's viability best journals embryo's viability top journals embryo's viability free medical journals embryo's viability famous journals embryo's viability Google Scholar indexed journals gestational age articles gestational age Research articles gestational age review articles gestational age PubMed articles gestational age PubMed Central articles gestational age 2023 articles gestational age 2024 articles gestational age Scopus articles gestational age impact factor journals gestational age Scopus journals gestational age PubMed journals gestational age medical journals gestational age free journals gestational age best journals gestational age top journals gestational age free medical journals gestational age famous journals gestational age Google Scholar indexed journals early pregnancy loss articles early pregnancy loss Research articles early pregnancy loss review articles early pregnancy loss PubMed articles early pregnancy loss PubMed Central articles early pregnancy loss 2023 articles early pregnancy loss 2024 articles early pregnancy loss Scopus articles early pregnancy loss impact factor journals early pregnancy loss Scopus journals early pregnancy loss PubMed journals early pregnancy loss medical journals early pregnancy loss free journals early pregnancy loss best journals early pregnancy loss top journals early pregnancy loss free medical journals early pregnancy loss famous journals early pregnancy loss Google Scholar indexed journals anterior uterine wall articles anterior uterine wall Research articles anterior uterine wall review articles anterior uterine wall PubMed articles anterior uterine wall PubMed Central articles anterior uterine wall 2023 articles anterior uterine wall 2024 articles anterior uterine wall Scopus articles anterior uterine wall impact factor journals anterior uterine wall Scopus journals anterior uterine wall PubMed journals anterior uterine wall medical journals anterior uterine wall free journals anterior uterine wall best journals anterior uterine wall top journals anterior uterine wall free medical journals anterior uterine wall famous journals anterior uterine wall Google Scholar indexed journals
Article Details
INTRODUCTION
An ultrasound scan is commonly performed in the first trimester of pregnancy to confirm the embryo's viability, estimate the gestational age, and establish the gestational sac's intrauterine location. This simple procedure requires relatively little expertise and is typically done in an office setting. During this scan, it is essential to exclude abnormal implantation of the gestational sac, such as implantation on a previous cesarean section scar. Upon diagnosis, refer those women to high-risk expert care. Accordingly, the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) guidelines state that determining the implantation site is an integral part of the first-trimester scan.[1] Nevertheless, the use of ultrasound for this purpose has not been systematically studied to date.
In this prospective study, we sought to estimate the accuracy of the first-trimester ultrasound scan in identifying the implantation site in women undergoing surgical termination of pregnancy for early pregnancy loss. For this purpose, we prospectively compared the ultrasound findings with those of diagnostic hysteroscopy in a blinded design.
Methods
This prospective cohort study was conducted at the Department of Obstetrics and Gynecology of the Shamir Medical Center (previously Assaf Harofe) between Julay 2021 and August 2022. The study was approved by the institutional review board and was registered at the clinicaltrial.gov database (https://clinicaltrials.gov/NCT04579796).
Women aged >18 years were recruited from a separate study in our department to assess the technique of hysteroscopy-guided suction and curettage for early pregnancy loss. In that study, following signed informed consent, diagnostic hysteroscopy was performed in the operative room under general anesthesia to determine the location of the gestational sac's insertion, followed by suction and curettage directed at the implantation wall. Recruitment took place before the scheduled surgical procedure.
Before the surgical procedure, ultrasound scans were obtained to assess the gestational sac location using the transabdominal approach. When that was insufficient for determining the implantation site, a transvaginal scan was added. Two experienced sonographers conducted the scans using equipment from different manufacturers with variable focus 3.5- to 5-MHz curvilinear and transvaginal probes. The implantation site was determined using direct visualization and demonstrating a feeding vessel from the uterine wall to the gestational sac with Doppler flow (Figure 1, Transvaginal ultrasound demonstrating gestational sac implantation in the anterior uterine wall).
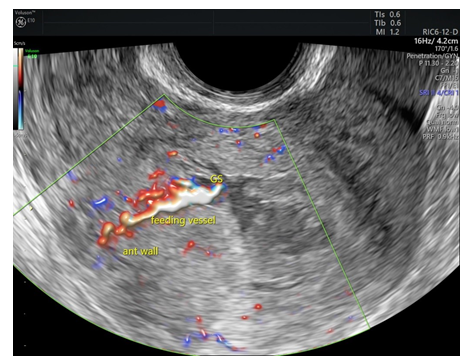
Figure 1: Transvaginal ultrasound demonstrating gestational sac implantation in the anterior uterine wall
On the same day, the surgical procedure combining diagnostic hysteroscopy and suction curettage was performed in the operating room under general anesthesia, as described above. For the diagnostic hysteroscopy, a 30o, 2.9 mm rigid hysteroscope using normal saline as the distention media was used. The implantation site of the gestational sac was observed on hysteroscopy by direct visualization (Figure 2).
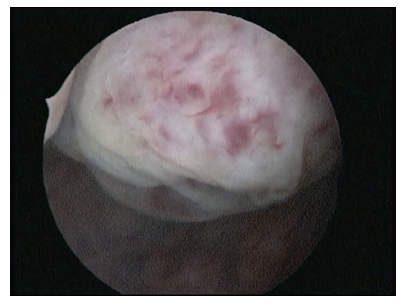
Figure 2: Hysteroscopy demonstrating gestational sac implantation in anterior uterine wall.
The surgical procedure and the ultrasound examination were done by two independent teams who were blinded to the other team's results.
Descriptive statistics are given as frequency (%) for categorical variables and median (range) for continuous variables. We used the Cramer's V correlation coefficient to estimate the correlation between the hysteroscopy and the ultrasound findings. A p-value <0.05 was considered statistically significant. The data were analyzed using SPSS V.25 (SPSS Chicago, IL, USA).
Results
The study included 20 women of those 17 with a singleton pregnancy and 3 with twin's pregnancy. The mean age of the women was 35 (s.d, 4) years. The median gravity was 4.5 (range 1 to 13) pregnancies, and the median parity was 2 (range 0 to 7) pregnancies. At the time of testing, the median gestational age was 9 (range: 6 to 13) weeks, and the median crown to rump length was 7 (range 6 to 9) mm. In 2 cases, we identified the gestational sacs in the cervical canal. The occurrence of incomplete abortion was correctly identified by both hysteroscopy direct observation and ultrasound imaging. The demographic and obstetric characteristics of participants are summarized in Table 1.
|
Characteristic |
|
|
Number of women |
20 |
|
Age, median (range), years |
35 (26 to 40) |
|
Gestational age, median (range), weeks |
9 ( 6 to 13) |
|
Mode of conception |
|
|
Spontaneous |
17 (85) |
|
IVF |
3 (15) |
|
Previous pregnancies, median (range) |
4 (1-13) |
|
Previous deliveries, median (range) |
2 (0-7) |
|
Previous pregnancy loss N (%) |
|
|
None |
7 (37) |
|
1 early missed abortion |
11 (58%) |
|
2 or more early missed abortions |
1 (5%) |
|
Previous cesarean sections |
|
|
None |
7 (37) |
|
1 |
11 (58) |
|
2 or more |
1 (5) |
Table 1: Demographics and Obstetrics characteristics of the study population
On hysteroscopy, the implantation wall was identified in 22 of 23 gestational sacs. In 8 (40%) cases, the gestational sac was identified on the anterior wall, in 9 (45%) on the posterior wall, and 3 (15%) on the fundus. The ultrasound examination identified identical implantation sites, except for one case where the hysteroscopy identified an anterior implantation site while the scan recorded it as posterior (figure 3).
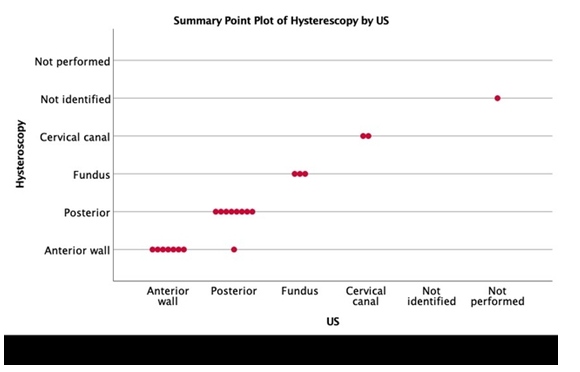
Figure 3: The distribution of gestational implantation site in US (ultrasound scan) versus Hysteroscopy.
The correlation between the sonographic and hysteroscopy findings was 0.96 (P < 0.0001).
Discussion
Verification of the ultrasound accuracy, compared with direct observation by hysteroscopy to the best of our knowledge, was never tested before. In clinical practice, identifying the implantation site is essential in viable pregnancies. This is especially so in pregnancies among women with a history of cesarean section as they are at high risk of scar pregnancy or placenta accreta with significant complications. The early detection of pathologies in such women will allow for early specialist referral for further evaluation and management.[2] The placenta/sac insertion location is also essential information for cases of first-trimester spontaneous abortion where cesarean scar pregnancy is managed differently and has a different outcome to intrauterine abortion and in cases of uterine malformations or abnormalities (e.g., subserous fibroids, uterine septum, etc.) where the implantation is essential for further counseling the patient.[2],[3] Another aspect of first-trimester spontaneous abortion is intrauterine adhesions. Friedler et al reported on an incidence of 16.3% of intrauterine adhesion in women after one curettage due to first-trimester abortion.[4] Knowing the location of the sac insertion will enable a more guided curettage approach, reduce the time of the procedure, and reduce the risk of intrauterine adhesions and residual trophoblastic tissue.
Our study included a subgroup of patients who participated in more extensive research investigating the procedure of hysteroscopy-guided suction curettage for early pregnancy loss. This provided us with accurate information on the location of the implantation wall on hysteroscopy and allowed us to compare the two modalities. Since the ultrasound team and the surgical team performed their examinations separately, each team was blinded to the other team's results. Although our study included a small patient cohort, our results support the current clinical practice of using ultrasound for identifying the implantation wall in the first trimester.
Among 22 gestational sacs identified, we found high concordance between these two modalities. This is reassuring and in line with current practice.
Although large-scale data using current imaging technology is lacking, early reports identified the uterine fundus and the posterior wall as more common implantation sites.[5] Nonetheless, in our study, implantation loci were evenly distributed between the posterior and the anterior uterine walls. We do not know why this discrepancy exists, although we cannot rule out that implantation in the anterior wall is associated with higher rates of early missed abortion. Other studies demonstrated a connection between placental location and adverse perinatal outcomes such as Preeclampsia and fetal growth restriction.[6],[7] The excellent correlation between the ultrasound scan and the hysteroscopy was demonstrated both in singleton and twin pregnancies. Our group published data regarding factors that allow for the prediction of hypertensive disorders in the first trimester in twin pregnancies[8],[9] so maybe placental location can be thought to be included in further studies.
Our study has several limitations. The study cohort was relatively small and included only women with first-trimester pregnancy loss. Also, the ultrasound scans were performed in optimal conditions (i.e., by expert sonographers using transabdominal and transvaginal probes and Doppler studies). Thus, our results may not be generalized to all practitioners.
In conclusion, an ultrasound scan can accurately identify implantation location in early gestation and compares favorably with diagnostic hysteroscopy.
The accurate identification of the implantation wall could be of benefit in various clinical scenarios such as a history of previous cesarean section, known intrauterine pathologies, and in women undergoing surgical termination of pregnancy.
Acknowledgements
We thank Howard Cuckle, Visiting Associate Professor, Faculty of Medicine, Tel Aviv University, Israel, for his useful remarks.
Disclosures
All of the authors of this article have reported no disclosures.
Funding
No funding was obtained for this study.
REFERENCES
- Salomon LJ, Alfirevic Z, Bilardo CM, et al. ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 2013; 41:102-113.
- Nguyen-Xuan HT, Lousquy R, Barranger E. [Diagnosis, treatment, and follow-up of cesarean scar pregnancy]. Gynecol Obstet Fertil 2014; 42:483-489.
- Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol 2012; 207:44 e1-13.
- Friedler S, Margalioth EJ, Kafka I, Yaffe H. Incidence of post-abortion intra-uterine adhesions evaluated by hysteroscopy--a prospective study. Hum Reprod 1993; 8:442-444.
- Kim SM, Kim JS. A Review of Mechanisms of Implantation. Dev Reprod 2017; 21:351-359.
- Seckin KD, Cakmak B, Karsli MF, et al. Is lateral localisation of placenta a risk factor for adverse perinatal outcomes? J Obstet Gynaecol 2015; 35:696-698.
- Salama-Bello R, Duncan JR, Howard SL, Song J, Schenone MH. Placental Location and the Development of Hypertensive Disorders of Pregnancy. J Ultrasound Med 2019; 38:173-178.
- Svirsky R, Levinsohn-Tavor O, Feldman N, Klog E, Cuckle H, Maymon R. First- and second-trimester maternal serum markers of pre-eclampsia in twin pregnancy. Ultrasound Obstet Gynecol 2016; 47:560-564.
- Svirsky R, Maymon R, Melcer Y, Klog E, Cuckle H. First and second trimester maternal serum inhibin A levels in twins with pre-eclampsia. Prenat Diagn 2016; 36:1071-1074.
