A Posterior Mediastinal Neurofibroma in a Five-Year-Old Girl
Article Information
Roeya kolsi¹*, Rim Belhaj¹, Amina Kammoun², Yosr Hentati², Zeineb Mnif², Hajer Aloulou¹, Ines Maaloul¹, Thouraya Kammoun¹
1Sfax Medical School, Department of Pediatrics, Hedi Chaker Hospital, Sfax, Tunisia
2Sfax Medical School, Department of Radiology, Hedi Chaker Hospital, Sfax, Tunisia
*Corresponding Author: Roeya kolsi, AHU, Department of pediatrics, Hédi Chaker Hospital, El Ain street Km 0,5, 3029, Sfax, Tunisia.
Received: 01 September 2023; Accepted: 07 September 2023; Published: 29 December 2023
Citation: Roeya kolsi, Rim Belhaj, Amina Kammoun, Yosr Hentati, Zeineb Mnif, Hajer Aloulou, Ines Maaloul, Thouraya Kammoun. A Posterior Mediastinal Neurofibroma in a Five-Year-Old Girl. Archives of Clinical and Medical Case Reports. 7 (2023): 453-455.
Share at FacebookAbstract
Neurofibromas are rare tumors that are often benign. We present the case of a 5-year-old girl who presented with a cough in a febrile context. The chest X-ray showed a posterior mediastinal syndrome and the spinal MRI showed a right posterior mediastinal mass, with regular outlines, with an extension at the level of the right conjugation foramen at the T11-T12 level. The biopsy showed a compatible aspect with a neurofibroma without histological signs of malignancy. The Checkup MRI showed a slight increase in tumor size and the therapeutic decision was to abstain with regular radiological monitoring.
Keywords
Neurofibroma; Mediastinal Tumor; Médiastinal Neurofibroma; Pediatrics
Neurofibroma articles; Mediastinal Tumor articles; M?diastinal Neurofibroma articles; Pediatrics articles.
Article Details
1. Introduction
Neurogenic tumors represent almost 30% of mediastinal tumors in children. Neurofibroma is the second neurogenic tumor, after schwannoma. It can be a sporadic tumor or part of Von Reklinghaussen disease. The clinical signs are not specific, the radiological diagnosis is not always obvious and the confirmation is histological.
2. Case Report
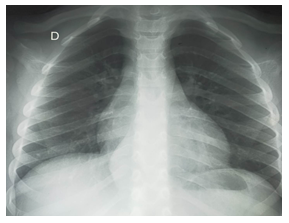
A 5-year-old girl was admitted with a cough associated with fever. The physical examination was unremarkable. The inflammatory assessment was negative. A chest x-ray was performed (Figure 1). It showed an oval opacity, with a long vertical axis, with regular external outlines, pushing back the right paravertebral line, with an infero-external contour joining the spine testifying to its purely thoracic location, without obvious bone lysis.
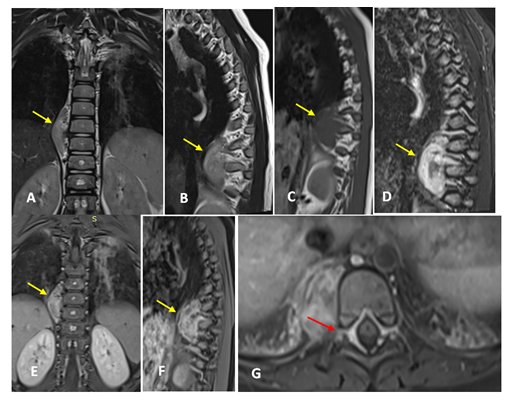
The thoraco-abdomino-pelvic scanner revealed a right posterior mediastinal tissue mass, with regular outlines, of homogeneous density, measuring 14*31*43 mm, at the height of the T9-T10 vertebrae, with extension at the level of the foramina of respective conjugations, without signs of bone erosion or pleural infiltration. To better study this mass, a thoraco-medullary MRI is completed (Figure 2). The latter showed a right posterior mediastinal mass, oval, with regular outlines, responsible for an extension at the level of the right conjugation foramen at the T11-T12 level.
Figure 2: MRI of the spinal cord in coronal (A), sagittal (B) T2, sagittal T1 (C) and STIR (D) sections and coronal (E), sagittal (F) and axial T1 FS after injection of gadolinium: Mediastinal mass, right posterior in heterogeneous hypersignal in T2 and STIR, hyposignal T1, enhanced after injection of gadolinium.We note an extension with regard to the conjugation foramen (Arrow red).
Blood smear and tumor lysis assessment were normal. NSE and metanephrine dosages were negative. The bone scan was normal. The scan-guided biopsy showed an aspect compatible with a neurofibroma without histological signs of malignancy. The diagnosis retained was a right posterior mediastinal neurofibroma. Ophthalmological examination did not show any Lish nodules and brain MRI did not show any other tumor masses. MRI check -up showed a slight increase in tumor size. The therapeutic decision was abstention with regular radiological monitoring.
3. Discussion
Neurogenic tumors of the mediastinum are tumors that develop at the expense of structures peripheral nervous system of the mediastinum, sympathetic nervous tissue and paraganglia. They represent approximately 9% of primary tumors of the mediastinum in adults and 30% of tumors in children [1, 2]. and they represent 53.9 of posterior mediastinum tumors[3]. They can occur in any mediastinal compartment. However, about 73 to 95% of them occur in the posterior mediastinum [3]. Neurofibromas represent the second neurogenic tumors after schwannomas, which are the majority [2]. Intrathoracic neurofibromas are rare. They may be solitary tumors, or associated with neurofibromatosis type 1, in 10 to 30% of cases [4]. There are three types of neurofibromas: localized neurofibromas, often sporadic (90%), they can be cutaneous, subcutaneous or intra-neural, the diffuse neurofibromas which are often subcutaneous, affecting the head and neck, they are sporadic in the majority of cases and plexiform neurofibromas, pathognomonic of the neurofibromatosis type 1 [5]. Sporadic intraneural localized neurofibromas appear, on average, between 20 and 30 years of age, without sex predilection [5], but when they have neurofibromatosis type 1, they usually appear in early childhood.
The clinical manifestations differ, depending on the location of the tumor. They result from the effect of mass exerted by the tumor. Extension to the spinal canal can cause pain spinal or motor deficits (para-paresis, paraplegia or tetra-paresis, in case of cervical extension). A lumbosacral extension, with damage to the cauda equina, can cause sensory problems or sphincter disorders [6].
The mediastinal neurofibroma can reach a large volume. However, it remains typically well limited, smooth, rounded or elliptical in the paravertebral space or along the courses of the vagus, phrenic, recurrent laryngeal or intercostal nerves [1, 6]. Macroscopically, the peripheral zone of the tumor is formed of gelatinous tissue and the central area is of solid tissue [6]. This is a benign tumor of the peripheral nerve sheath that contains several types of cells. Neoplastic Schwann cells represent the main cell type. Generally, they are spindle-shaped cells with hyperchromatic corrugated nuclei [7].
On the frontal chest X-ray, the tumor appears as homogeneous of water tone opacity, with a well-defined external border and an internal border contiguous to the mediastinum. Its headquarters at the posterior mediastinum is reflected by its projection on the spine, on the profile view and by the absence of the erasing of the edge of the heart, on the frontal image. When the mass is too large, it can take the entire pulmonary hemi-field. Dorsal spine x-rays often show scalloping of the posterior border of the vertebral bodies adjacent to the tumor and an enlargement of the foramina of conjugation [6]. Most radiological signs of neurofibromas are common to all neurogenic tumors. One of these characteristic signs is the fusiform appearance, following longitudinally the course of the nerve and shows often tapering ends contiguous to the parent nerve. MRI makes it possible to better show this fusiform aspect during nerve sheath tumors peripherals [5].
CT shows a well-defined, smooth or lobulated mass. It has the same or a lower density than that of soft tissues (due to the presence of Schwann cells, neural elements and fat cells) [6, 5]. It may also show a split fat sign [5]. CT allows a very detailed analysis of the bone structures of the spine and the sides. The scalloping of the vertebral bodies and widening of the mating foramina are better visualized on CT [1, 6]. After the injection of the contrast product, it generally appears a homogeneous enhancement with possibility of early central enhancement [8]. More than half of neurofibromas remain hypodense after the injection of contrast product [5].
In MRI, on T1-weighted images, neurofibromas appear homogeneous, with weak signal to intermediate, with a slightly stronger signal in the center than in the periphery [6, 3, 5]. In T2, the characteristic aspect is made of a hypointense central zone surrounded by a zone peripheral hyperintense (target sign), but the signal may be homogeneous hyperintense. The target sign is described as being pathognomonic for neurofibroma, but it can also be observedin schwannoma and malignant peripheral nerve sheath tumors [5]. Areas nodules or bands, in hypersignal, can separate the central and peripheral zones [6]. After injection of Gadolinium, in two-thirds of cases, an inhomogeneous enhancement is observed.
MRI can distinguish neurofibroma from other nerve tumors. Schwannoma, the most frequent neurogenic tumor, shows a heterogeneous hypersignal, in T2, with a central zone in intense hypersignal and diffuse enhancement after injection of gadolinium. The carrier nerve is eccentric, in case of schwannoma and it is well centered in case of neurofibroma. In the case of neurofibrosarcoma, the internal structure is heterogeneous and irregular in T2, corresponding to areas of necrosis. The large size and heterogeneous appearance described as characteristic signs of sarcomatous degeneration, in neurofibromatosis, could be observed in large benign neurofibromas [6]. The target sign is in favor of the benign nature of benign neurofibroma [9].
The differential diagnosis of neurofibromas arises, mainly, with the shwannoma, but also with neuroblastoma, ganglioneuroma, and neurofibrosarcoma. Other abnormalities may be evoked, in case of paravertebral neurofibroma, such as a meningocele, a neuro-enteric cyst or extramedullary hematopoiesis. When the tumor causes erosion or bone destruction, in a child, Ewing's sarcoma, lymphoma, rhabdomyosarcoma, or bone metastasis can also be mentioned [1, 3, 6].
Complete surgical resection is the treatment of choice for neurogenic tumors of the mediastinum, without the need for a prior biopsy [10]. It is indicated for shapes symptomatic, large volumes or presenting a risk of spinal cord compression. The prognosis is generally good with a low morbidity rate [6].
4. Conclusion
Neurofibroma is a rare tumor, often sporadic. The diagnosis is often fortuitous or made on the occasion of a compression of an adjacent structure. It is usually benign. Surgery is not systematic and the prognosis is good.
Funding
No funding was associated with this article.
Declaration of Interest
The authors declare no conflicts of interest.
References
- Fortman BJ, Kuszyk BS, Urban BA, et al. Neurofibromatosis Type 1. A diagnostic mimicker at CT. Radio Graphics 21 (2001): 601-612.
- Saito H, Yoshihiro Minamiya, Kasumi Tozawa, Ikuo Matsuzaki, Kosei Taguchi, et al. Mediastinal neurofibroma originating from the left intrathoracic phrenic nerve: report of a case. Case Reports 34 (2004): 950-953.
- Topc¸u S, Alper A, Gülhan E, et al. Neurogenic tumors of the mediastinum: a report of 60 cases. Can Respir J 7 (2007): 261-265.
- Tanaka O, Takuji Kiryu, Yoshinobu Hirose, et al. Neurogenic Tumors of the Mediastinum and Chest Wall. J Thorac Imaging 20 (2005): 316-20.
- Pilavaki M, Chourmouzi D, Kiziridou A, et al. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol 52 (2004): 229-239.
- B, Jidal M, Chaouir S, et al. Volumineux neurofibrome médiastinal chez un enfant. Presse Med 37 (2008): 783-786.
- Erika F. Rodriguez, Jones R, Miller D, et al. Neurogenic Tumors of the Mediastinum. Semin Diagn Pathol 37 (2020): 179-186.
- Pavlus J, Carter B, Tolley MD, et al. Imaging of Thoracic Neurogenic Tumors. AJRAm J Roentgenol 207 (2016): 552-561.
- Arazi-kleinmann T, Mor Y, Brand N, Gayer G, et al. Neurofibromatosis diagnosed on CT with MR correlation. Eur J Radiol 42 (2002): 69-73.
- Trousse D, Avaro JP. Introduction aux tumeurs du médiastin. RevPneumol Clin 66 (2010): 3—16.