A Pediatric Case Report: Three-Year-Old Girl Diagnosed with Narcolepsy with Cataplexy
Article Information
Annie Kincaid, RN, MSN, FNP-C1, S. Kamal Naqvi, MD1,2 ?
1Sleep Disorders Center Children’s health Dallas, Texas, USA
2UT Southwestern Medical Center, Department of Pediatrics, Division of Respiratory and Sleep Medicine, Dallas, Texas, USA
*Corresponding Author: Dr. S. Kamal Naqvi, MD, Associate Professor of Pediatrics at UT Southwestern Medical Center, Dallas, Texas, USA
Received: 27 February 2020; Accepted: 10 March 2020; Published: 11 May 2020
Citation: Annie Kincaid, RN, MSN, FNP-C, S. Kamal Naqvi, MD. A Pediatric Case Report: Three-Year-Old Girl Diagnosed with Narcolepsy with Cataplexy. Journal of Psychiatry and Psychiatric Disorders 4 (2020): 75-78.
Share at FacebookAbstract
Narcolepsy with cataplexy is a lifelong disorder of the central nervous system characterized by excessive daytime sleepiness, cataplexy, hypnagogic or hypnopompic hallucinations, sleep paralysis and disrupted nocturnal sleep [1]. We present a case report of a three-year-old girl diagnosed with narcolepsy 7 months after symptoms surfaced, successfully treated with methylphenidate and venlafaxine. The patient underwent a Polysomnography (PSG) followed by a multiple sleep latency test (MSLT). She underwent a brain MRI and a full montage video- electroencephalogram (EEG). Laboratory tests were performed, including human leukocyte antigen (HLA). Actigraphy was also obtained as was the modified Epworth Sleepiness Scale.
Pediatric articles, Case Report articles
electroencephalogram articles electroencephalogram Research articles electroencephalogram review articles electroencephalogram PubMed articles electroencephalogram PubMed Central articles electroencephalogram 2023 articles electroencephalogram 2024 articles electroencephalogram Scopus articles electroencephalogram impact factor journals electroencephalogram Scopus journals electroencephalogram PubMed journals electroencephalogram medical journals electroencephalogram free journals electroencephalogram best journals electroencephalogram top journals electroencephalogram free medical journals electroencephalogram famous journals electroencephalogram Google Scholar indexed journals multiple sleep latency test articles multiple sleep latency test Research articles multiple sleep latency test review articles multiple sleep latency test PubMed articles multiple sleep latency test PubMed Central articles multiple sleep latency test 2023 articles multiple sleep latency test 2024 articles multiple sleep latency test Scopus articles multiple sleep latency test impact factor journals multiple sleep latency test Scopus journals multiple sleep latency test PubMed journals multiple sleep latency test medical journals multiple sleep latency test free journals multiple sleep latency test best journals multiple sleep latency test top journals multiple sleep latency test free medical journals multiple sleep latency test famous journals multiple sleep latency test Google Scholar indexed journals human leukocyte antigen articles human leukocyte antigen Research articles human leukocyte antigen review articles human leukocyte antigen PubMed articles human leukocyte antigen PubMed Central articles human leukocyte antigen 2023 articles human leukocyte antigen 2024 articles human leukocyte antigen Scopus articles human leukocyte antigen impact factor journals human leukocyte antigen Scopus journals human leukocyte antigen PubMed journals human leukocyte antigen medical journals human leukocyte antigen free journals human leukocyte antigen best journals human leukocyte antigen top journals human leukocyte antigen free medical journals human leukocyte antigen famous journals human leukocyte antigen Google Scholar indexed journals quality of life articles quality of life Research articles quality of life review articles quality of life PubMed articles quality of life PubMed Central articles quality of life 2023 articles quality of life 2024 articles quality of life Scopus articles quality of life impact factor journals quality of life Scopus journals quality of life PubMed journals quality of life medical journals quality of life free journals quality of life best journals quality of life top journals quality of life free medical journals quality of life famous journals quality of life Google Scholar indexed journals sleep-onset REM period articles sleep-onset REM period Research articles sleep-onset REM period review articles sleep-onset REM period PubMed articles sleep-onset REM period PubMed Central articles sleep-onset REM period 2023 articles sleep-onset REM period 2024 articles sleep-onset REM period Scopus articles sleep-onset REM period impact factor journals sleep-onset REM period Scopus journals sleep-onset REM period PubMed journals sleep-onset REM period medical journals sleep-onset REM period free journals sleep-onset REM period best journals sleep-onset REM period top journals sleep-onset REM period free medical journals sleep-onset REM period famous journals sleep-onset REM period Google Scholar indexed journals sleep articles sleep Research articles sleep review articles sleep PubMed articles sleep PubMed Central articles sleep 2023 articles sleep 2024 articles sleep Scopus articles sleep impact factor journals sleep Scopus journals sleep PubMed journals sleep medical journals sleep free journals sleep best journals sleep top journals sleep free medical journals sleep famous journals sleep Google Scholar indexed journals Pediatric articles Pediatric Research articles Pediatric review articles Pediatric PubMed articles Pediatric PubMed Central articles Pediatric 2023 articles Pediatric 2024 articles Pediatric Scopus articles Pediatric impact factor journals Pediatric Scopus journals Pediatric PubMed journals Pediatric medical journals Pediatric free journals Pediatric best journals Pediatric top journals Pediatric free medical journals Pediatric famous journals Pediatric Google Scholar indexed journals Cataplexy articles Cataplexy Research articles Cataplexy review articles Cataplexy PubMed articles Cataplexy PubMed Central articles Cataplexy 2023 articles Cataplexy 2024 articles Cataplexy Scopus articles Cataplexy impact factor journals Cataplexy Scopus journals Cataplexy PubMed journals Cataplexy medical journals Cataplexy free journals Cataplexy best journals Cataplexy top journals Cataplexy free medical journals Cataplexy famous journals Cataplexy Google Scholar indexed journals Narcolepsy articles Narcolepsy Research articles Narcolepsy review articles Narcolepsy PubMed articles Narcolepsy PubMed Central articles Narcolepsy 2023 articles Narcolepsy 2024 articles Narcolepsy Scopus articles Narcolepsy impact factor journals Narcolepsy Scopus journals Narcolepsy PubMed journals Narcolepsy medical journals Narcolepsy free journals Narcolepsy best journals Narcolepsy top journals Narcolepsy free medical journals Narcolepsy famous journals Narcolepsy Google Scholar indexed journals hypnopompic hallucinations articles hypnopompic hallucinations Research articles hypnopompic hallucinations review articles hypnopompic hallucinations PubMed articles hypnopompic hallucinations PubMed Central articles hypnopompic hallucinations 2023 articles hypnopompic hallucinations 2024 articles hypnopompic hallucinations Scopus articles hypnopompic hallucinations impact factor journals hypnopompic hallucinations Scopus journals hypnopompic hallucinations PubMed journals hypnopompic hallucinations medical journals hypnopompic hallucinations free journals hypnopompic hallucinations best journals hypnopompic hallucinations top journals hypnopompic hallucinations free medical journals hypnopompic hallucinations famous journals hypnopompic hallucinations Google Scholar indexed journals
Article Details
1. Introduction
Narcolepsy is a lifelong disorder of the central nervous system characterized by excessive daytime sleepiness, cataplexy, hypnagogic or hypnopompic hallucinations, sleep paralysis and disrupted nocturnal sleep [1]. Excessive daytime sleepiness that occurs with narcolepsy results in significant daytime impairment, mood or behavior changes, making functioning at school or work challenging. Diagnosing narcolepsy can be difficult due to the variability of symptoms. The HLA-DQB1*06:02 gene variant has a strong relation to narcolepsy, though the absence of this gene cannot exclude narcolepsy as a diagnosis [2]. An early diagnosis of narcolepsy is essential, in order to establish early intervention, thus leading to a better-quality of life.
In general, narcolepsy with cataplexy is rare in children before the age of 5 years old. Narcolepsy may start early in age but may be more noticeable in later childhood and adolescents with symptoms peaking around 14 years of age, though there is often a delay in diagnosis [3]. A database review of over 1200 cases revealed the onset of symptoms of narcolepsy before the age of 5 years old is 2.1% with 1.1% exhibiting cataplexy [3].
2. Report of Case
A 3-year old female was referred to the pediatric sleep disorders clinic for evaluation of excessive daytime sleepiness, aggressive behaviors, sleep terrors and frequent nighttime awakenings. She is developmentally appropriate with no significant past medical history prior to the onset of symptoms 5 months ago. She experienced behavior changes and significant weight gain along with daytime somnolence. Symptoms were not preceded by influenza, influenza vaccine, strep infection and/or head injury. The patient has been difficult to arouse, extremely aggressive when awoken and with sluggish movements. Mother reports the patient sleeps around 20 hours a day. She has been known to fall asleep in school, the bathtub, grocery stores, restaurants, while eating, using the bathroom and during conversations. She experiences muscle weakness in her shoulders, neck and legs when laughing. She has fallen to the ground with laughter. There were reports of nocturnal awakenings due to extremely vivid dreams. Physical exam was remarkable for obesity without narrowing of upper airway.
The polysomnography (PSG) demonstrated no evidence of obstructive or central sleep apnea. No evidence of periodic limb movements was seen. Episodes of muscle weakness, staring spells and aggression were present during the study with no EEG abnormalities noted. The MSLT followed the overnight study showing a mean sleep latency of 6.9 minutes. Sleep was observed in 4 out of 5 naps with sleep-onset REM periods (SOREM) noted in 3 naps.
Narcolepsy HLA DQB1*0602 was positive. Modified Epworth sleepiness scale was 24 demonstrating severe excessive daytime sleepiness. Actigraphy was attempted though no data was collected due to patient noncompliance. MRI brain, routine laboratory tests and EEG revealed no abnormalities.
With these results, she was diagnosed with narcolepsy with cataplexy. Parent was educated on her diagnosis and possible treatment options. In order to minimize daytime somnolence, she was started on methylphenidate 5 mg in the morning. Venlafaxine 37.5 mg was started daily to treat cataplexy. Lifestyle modifications were discussed at length, including routine sleep/wake time, avoiding sleep deprivation and schedule short naps when most sleepy during the day in order to be more productive [1]. Safety concerns were addressed, and school accommodations were mentioned. Patient continuously improved on subsequent clinic visits, returning to optimal daytime functioning over the next year.
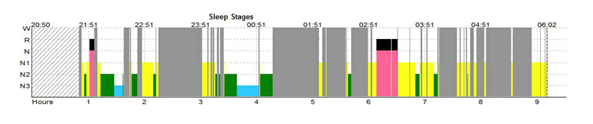
Table 1
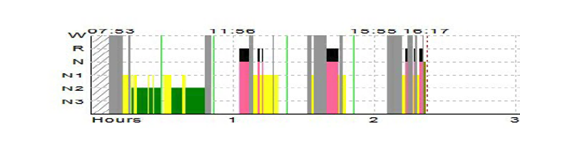
Table 2
3. Discussion
Diagnosing narcolepsy with cataplexy is often delayed as it is a rare disorder. Typically patients are referred to multiple specialists before embarking upon a correct diagnosis of narcolepsy. The diagnosis in children is challenging as their presenting symptoms are usually not straightforward [2]. The average time between onset of symptoms and diagnosis of narcolepsy is 10-15 years [2]. Studies have suggested that most cases of narcolepsy have symptom onset after 10 years of age and only 5% of cases showing an onset of symptoms prior to 10 years of age [2]. The American Academy of Sleep Medicine, proposes diagnostic utility of the MSLT in school age children age 5 years and up [4]. The Epworth sleepiness scale has been used in several research studies and shown validity in assessing sleepiness in children 6-16 years of age [5].
4. Conclusion
In conclusion, early identification and intervention is key for children with narcolepsy with cataplexy. Stimulants in combination with an anti-cataplexy agent, significantly reduces daytime somnolence, cataplexy as well as improved mood and behavior. Assuring adequate sleep opportunity and education of the care providers result in optimal outcomes.
References
- Mindell JA, Owens JA.A clinical guide to pediatric sleep: diagnosis and management of sleep problems (3rd ed.). Philadelphia: Wolters Kluwer/Lippincott Williams and Wilkins (2015).
- Zhou J, Zhang X, Dong Z. Case report of narcolepsy in a six-year-old child initially misdiagnosed as atypical epilepsy.Shanghai Archives of Psychiatry 26 (2014): 232-235.
- Ratkiewicz M, Splaingard M. Treatment of Cataplexy in a Three-Year-Old Using Venlafaxine.Journal of Clinical Sleep Medicine 09 (2013): 341-1342.
- Kotagal S, Nichols CD, Grigg-Damberger MM, et al. Non-Respiratory Indications for Polysomnography and Related Procedures in Children: An Evidence-Based Review. Sleep 35 (2012): 1451-1466.
- Krahn LE, Hershner S, Loeding LD, et al. Quality Measures for the Care of Patients with Narcolepsy. Journal of Clinical Sleep Medicine 11 (2015): 335-338.
