A New Score of Positivity in Thallium Studies of Ischemic Patients
Article Information
Samir Rafla*, Ahmed Gaber, Gehan Magdy, Ahmed Abdelaaty
Alexandria University, Faculty of Medicine, Cardiology Department, Alexandria, Egypt
*Corresponding author: Samir Rafla, Alexandria University, Faculty of Medicine, Cardiology Department, Alexandria, Egypt
Received: 27 December 2019; Accepted: 06 January 2020; Published: 23 January 2020
Citation: Samir Rafla, Ahmed Gaber, Gehan Magdy, Ahmed Abdelaaty. A New Score of Positivity in Thallium Studies of Ischemic Patients. Cardiology and Cardiovascular Medicine 4 (2020): 045-057.
Share at FacebookAbstract
The aim of this work was to detect means to increase accuracy of prediction of Thallium perfusion results. Also, we aimed to investigate the incidence and severity of chest pain during radionuclide myocardial perfusion imaging and its relation to the stress modality.
The study was conducted on two groups of patients that presented for radionuclide myocardial perfusion imaging. The first group included fifty patients subjected to exercise stress testing. The second group included fifty patients subjected to dipyridamole pharmacologic stress testing. The 2 groups were compared regarding chest pain, dyspnea, electrocardiographic changes, left ventricular dilatation, and increased lung thallium uptake. Exercise was associated with a statistically significant higher incidence and severity of chest pain compared to dipyridamole (p<0.001). The incidence and severity of chest pain were related to the number of vessel territories affected in the dipyridamole group (p=0.037), but not in the exercise group. Exercise was associated with a statistically significant higher incidence of electrocardiographic (ECG) changes compared to dipyridamole (p<0.001). There was no statistically significant difference in the incidence of left ventricular dilatation between the 2 groups. The incidence of left ventricular dilatation was related to the number of vessel territories affected in the exercise group (p=0.011) as well as the dipyridamole group (p=0.007). There was no statistically significant difference in the incidence of increased lung thallium-201 uptake between the 2 groups. The incidence of increased lung thallium-201 uptake was related to the number of vessel territories affected in the exercise group (p=0.017) but not in the dipyridamole group.
We summed four parameters 1- chest pain (one or two or three points), 2- ECG changes > 1mm (two points), 3- LV dilation (two points), and 4- Lung thallium uptake (two points), so maximum can be 9
Keywords
Radionuclide myocardial perfusion; Imaging; ischemic heart disease; Dipyridamole; Exercise stress test; Thallium
Radionuclide myocardial perfusion articles, Imaging articles, ischemic heart disease articles, Dipyridamole articles, Exercise stress test articles, Thallium articles
Article Details
Abbreviations
Myocardial perfusion imaging (MPI); Lung/heart ratio (LHR); Single photon emission computed tomography (SPECT); Coronary artery disease (CAD); Adenosine triphosphate (ATP); Verbal rating scale (VRS).
Introduction
Ischemic heart disease (IHD) is becoming a major health problem affecting many parts of the world. In Egypt, ischemic heart disease affected more than 2.5 million individuals in 2016 [1] and caused more than 144 thousand deaths [2].
Chest pain remains the second most common cause of non-injury related emergency department visits. Although the presence of chest pain raises the suspicion of myocardial ischemia, only 13% of the emergency department visits for chest pain are diagnosed with acute coronary syndrome [4,5].
A multitude of investigative tools are available for the assessment of chest pain. Radionuclide myocardial perfusion imaging is a well-established non-invasive imaging technique that provides both diagnostic and prognostic data. Radionuclide myocardial perfusion imaging uses intravenous radiopharmaceuticals that distributes to the myocardium in proportion to regional myocardial perfusion to assess myocardial perfusion during stress and rest. Myocardial distribution of the radiopharmaceutical is compared in states of stress and rest to provide information on perfusion anomalies, myocardial viability, and, when electrocardiographic gating is used, myocardial function [6,7].
Stress is achieved by exercise or pharmacologic agents. Exercise stress is preferred over pharmacologic agents as it is the most physiological form of cardiac stress, it allows the assessment of exercise capacity, heart rate and blood pressure responses including reserve and recovery, and the development of symptoms which are useful for clinical decision making. Additionally, exercise stress offers superior image quality compared with pharmacologic vasodilator stress due to splanchnic vasoconstriction which allows for a smaller proportion of the injected radiopharmaceutical tracer to appear in the gut [8]. Within normal coronary territories, exercise stress increases coronary blood flow 2-3 folds as a secondary effect to increased myocardial oxygen demand [9].
For patients unable to exercise or achieve an adequate level of exercise pharmacologic stress is used. The vasodilator pharmacologic stress agents used are adenosine, dipyridamole, or regadenoson. These agents increase the coronary blood flow 3-5 folds within normal coronary territories which are significantly higher than exercise and inotropic pharmacologic stress, however, vasodilator pharmacologic stress does not produce greater heterogenicity in perfusion between normal and abnormal coronary territories compared to exercise and inotropic pharmacologic stress. This is due to the plateauing relation between perfusion and uptake of the available radiopharmaceutical tracers at higher flow rates. This is known as the roll-off phenomenon [9]. In most cases perfusion heterogenicity occurs in the absence of metabolic ischemia, as myocardial oxygen demand is not affected [10].
The aim of this work was to investigate the incidence and severity of chest pain during radionuclide myocardial perfusion imaging and its relation to the stress modality used and the findings of the radionuclide myocardial perfusion imaging.
Methods
This study was conducted retrospectively and prospectively on two groups of patients that presented for radionuclide myocardial perfusion imaging. All the 100 patients had positive Thallium result i.e. showed perfusion defects.
- The first group: fifty patients subjected to exercise stress testing, twenty-five cases were prospective, and twenty-five cases were retrospective.
- The second group: fifty patients subjected to dipyridamole pharmacologic stress testing, twenty-five cases were prospective, and twenty-five cases were retrospective.
Exclusion criteria included assessment of myocardial viability through rest-redistribution protocol with no cardiac stress; the presence of contraindication to cardiac stress test, severe valvular heart disease, severe heart failure, or pregnancy, and inability to obtain patient’s consent.
Patients were subjected to detailed history taking including personal data, risk factors, current complaint and its analysis, medical conditions, medications, and previous surgeries. Patients were also subjected to full cardiac examination.
For the first group myocardial stress was achieved by treadmill exercise through the Bruce protocol.
The radiopharmaceutical was injected just prior to peak exercise followed by saline flush. Peak exercise was marked by the sustained achievement of target heart rate, that is, 85% of maximum predicted heart rate (220 – age for males, 210 – age for females) or the development of limiting chest pain. Patient continued to exercise for 1 minute following radiopharmaceutical injection before starting recovery. Heart rate, blood pressure, and 12-lead ECG were monitored for 4 minutes into recovery, or longer if chest pain or ischemic ECG changes were found.
For the second group myocardial stress was achieved by dipyridamole. Dipyridamole acts by increasing the extracellular concentration of endogenous adenosine which causes coronary vasodilatation and increases myocardial perfusion. Heart rate, blood pressure, and 12-lead ECG were recorded prior to dipyridamole injection. Dipyridamole (0.56 mg/kg diluted with 0.9% saline in a 10-ml syringe) was injected by hand over 4 minutes. Heart rate, blood pressure, and 12-lead ECG were recorded every 2 minutes or if side effects as chest pain, dyspnea, and dizziness developed. The radiopharmaceutical was injected 3-4 minutes after dipyridamole injection.
Thallium-201 (80 MBq) was injected during stress. Stress image acquisition was done 5-10 minutes post injection, while redistribution image acquisition was done 4 hours post injection. Image acquisition was done using Symbia E dual head multi-purpose SPECT system. Image interpretation was performed by experienced staff members of Alexandria university nuclear cardiology lab. Diagnostic criteria were based on the detection of reversible perfusion defects (considered as myocardial ischemia). No quantitative analysis was used, but rather the visual analysis of experienced observers.
Statistics: Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. The Kolmogorov-Smirnov test was used to verify the normality of distribution Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level. The tests used were Chi-square test, Fisher’s Exact, Monte Carlo correction, Student t-test, Mann Whitney test, and Spearman coefficient.
Results
|
Number of vessel territories affected |
Test of |
p |
||||||
|
1 Vessel territory |
2 Vessels territories |
3 Vessels territories |
||||||
|
No. |
No. |
No. |
||||||
|
NYHA class |
||||||||
|
Class I |
0 |
0.0 |
3 |
14.3 |
0 |
0.0 |
χ2= |
MCp= |
|
Class II |
15 |
71.4 |
10 |
47.6 |
2 |
25.0 |
||
|
Class III |
6 |
28.6 |
8 |
38.1 |
6 |
75.0 |
||
|
Class IV |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
||
|
VRS chest pain |
||||||||
|
No pain |
9 |
42.9 |
10 |
47.6 |
3 |
37.5 |
χ2= |
MCp= |
|
Mild pain |
6 |
28.6 |
3 |
14.3 |
1 |
12.5 |
||
|
Moderate pain |
2 |
9.5 |
3 |
14.3 |
1 |
12.5 |
||
|
Severe pain |
4 |
19.0 |
5 |
23.8 |
3 |
37.5 |
||
|
ECG changes |
||||||||
|
No |
8 |
38.1 |
8 |
38.1 |
2 |
25.0 |
χ2= |
0.779 |
|
Yes |
13 |
61.9 |
13 |
61.9 |
6 |
75.0 |
||
|
LV dilatation |
||||||||
|
No |
17 |
81.0 |
11 |
52.4 |
2 |
25.0 |
8.285* |
MCp= |
|
Yes |
4 |
19.0 |
10 |
47.6 |
6 |
75.0 |
||
|
Increased lung thallium-201 uptake |
||||||||
|
No |
21 |
100.0 |
15 |
71.4 |
6 |
75.0 |
χ2= |
MCp= |
|
Yes |
0 |
0.0 |
6 |
28.6 |
2 |
25.0 |
||
Table 1: Relation between number of vessel territories affected and different parameters in the exercise group
|
Number of vessel territories affected |
Test of |
p |
||||||
|
1 Vessel territory |
2 Vessels territories |
3 Vessels territories |
||||||
|
No. |
No. |
No. |
||||||
|
NYHA class |
||||||||
|
Class I |
1 |
3.8 |
0 |
0.0 |
0 |
0.0 |
χ2= |
MCp= |
|
Class II |
14 |
53.8 |
8 |
44.4 |
2 |
33.3 |
||
|
Class III |
9 |
34.6 |
9 |
50.0 |
4 |
66.7 |
||
|
Class IV |
2 |
7.7 |
1 |
5.6 |
0 |
0.0 |
||
|
VRS chest pain |
||||||||
|
No pain |
25 |
96.2 |
16 |
88.9 |
4 |
66.7 |
χ2= |
MCp= |
|
Mild pain |
1 |
3.8 |
0 |
0.0 |
0 |
0.0 |
||
|
Moderate pain |
0 |
0.0 |
1 |
5.6 |
0 |
0.0 |
||
|
Severe pain |
0 |
0.0 |
1 |
5.6 |
2 |
33.3 |
||
|
ECG changes |
||||||||
|
No |
21 |
80.8 |
16 |
88.9 |
3 |
50.0 |
χ2= |
MCp= |
|
Yes |
5 |
19.2 |
2 |
11.1 |
3 |
50.0 |
||
|
LV Dilatation |
||||||||
|
No |
17 |
65.4 |
7 |
38.9 |
0 |
0.0 |
χ2= |
MCp= |
|
Yes |
9 |
34.6 |
11 |
61.1 |
6 |
100.0 |
||
|
Increased lung thallium-201 uptake |
||||||||
|
No |
21 |
80.8 |
12 |
66.7 |
5 |
83.3 |
χ2= |
MCp= |
|
Yes |
5 |
19.2 |
6 |
33.3 |
1 |
16.7 |
||
Table 2: Relation between number of vessels territories affected and different parameters in dipyridamole group
Test hemodynamic response
Within the exercise group the resting heart rate ranged from 55 to 115 beats per minute with a mean of 78.5 ± 15.4 beats per minute. Peak heart rate ranged from 85 to 179 beats per minute with a mean of 134.8 ± 21.7 beats per minute. Exercise induced a mean increase of 56.2 ± 22.2 beats per minute in heart rate.
The resting systolic blood pressure ranged from 100 to 160 mmHg with a mean of 127.7 ± 15.56 mmHg. Peak systolic blood pressure ranged from 70 to 200 mmHg with a mean of 146.6 ± 21.53 mmHg. Exercise induced a mean increase of 18.90 ± 18.39 mmHg in systolic blood pressure.
The resting diastolic blood pressure ranged from 60 to 100 mmHg with a mean of 78.80 ± 7.46 mmHg. Peak diastolic blood pressure ranged from 40 to 110 mmHg with a mean of 86.98 ± 11.45 mmHg. Exercise induced a mean increase of 8.18 ± 9.64 mmHg in diastolic blood pressure.
Within the dipyridamole group the resting heart rate ranged from 55 to 120 beats per minute with a mean of 81.40 ± 13.37 beats per minute. Peak heart rate ranged from 61 to 121 beats per minute with a mean of 86.90 ± 13.80 beats per minute. Dipyridamole induced a mean increase of 5.50 ± 8.63 beats per minute in heart rate.
The resting systolic blood pressure ranged from 100 to 200 mmHg with a mean of 136.8 ± 24.11 mmHg. Peak systolic blood pressure ranged from 90 to 220 mmHg with a mean of 135.7 ± 27.81 mmHg. Dipyridamole induced a mean decrease of -1.10 ± 18.77 mmHg in systolic blood pressure.
The resting diastolic blood pressure ranged from 60 to 100 mmHg with a mean of 82.80 ± 10.31 mmHg. Peak diastolic blood pressure ranged from 60 to 120 mmHg with a mean of 83.80 ± 13.23 mmHg. Dipyridamole induced a mean increase of 1.0 ± 10.74 mmHg in diastolic blood pressure.
Comparison of the two groups according to chest pain and other ischemic parameters
Within the exercise group 22 patients (44%) experienced no chest pain during the test, 10 patients (20%) had mild chest pain, 6 patients (12%) had moderate chest pain, and 12 patients (24%) had severe chest pain.
ECG changes occurred in 32 patients (64%), increased lung thallium-201 uptake occurred in 8 patients (16%), and left ventricular dilatation occurred in 20 patients (40%) out of which 8 patients had preexisting dilatation that increased during the test.
Within the dipyridamole group 45 patients (90%) experienced no chest pain during the test, 1 patient (2%) had mild chest pain, 1 patient (2%) had moderate chest pain, and 3 patients (6%) had severe chest pain.
ECG changes occurred in 10 patients (20%), increased lung thallium-201 uptake occurred in 12 patients (24%), and left ventricular dilatation occurred in 26 patients (52%) out of which 14 patients had preexisting dilatation that increased during the test.
Comparison of the two groups according to the results of myocardial perfusion imaging
Within the exercise group 21 patients (42%) had ischemia in 1 vessel territory, of these 5 patients (10%) had ischemia in the left anterior descending artery (LAD) territory, 11 patients (22%) had ischemia in the right coronary artery (RCA) territory, and 5 patients (10%) had ischemia in the Left circumflex artery (LCX) territory.
21 patients (42%) had ischemia in 2 vessels territories, of these 11 patients (22%) had ischemia in the left anterior descending artery (LAD) and the right coronary artery (RCA) territories, 8 patients (16%) had ischemia in the left anterior descending artery (LAD) and the Left circumflex artery (LCX) territories, and 2 patients (4%) had ischemia in the right coronary artery (RCA) and the Left circumflex artery (LCX) territories. 8 patients (16%) had ischemia in 3 vessels territories.
Collectively, ischemia within the left anterior descending artery (LAD) territory was present in 32 patients (64%), ischemia within the right coronary artery (RCA) territory was present in 32 patients (64%), and ischemia within the left circumflex artery (LCX) territory was present in 23 patients (46%).
Within the dipyridamole group 26 patients (52%) had ischemia in 1 vessel territory, of these 16 patients (32%) had ischemia in the left anterior descending artery (LAD) territory, 7 patients (14%) had ischemia in the right coronary artery (RCA) territory, and 3 patients (6%) had ischemia in the Left circumflex artery (LCX) territory.
18 patients (36%) had ischemia in 2 vessels territories, of these 8 patients (16%) had ischemia in the left anterior descending artery (LAD) and the right coronary artery (RCA) territories, 7 patients (14%) had ischemia in the left anterior descending artery (LAD) and the Left circumflex artery (LCX) territories, and 3 patients (6%) had ischemia in the right coronary artery (RCA) and the Left circumflex artery (LCX) territories. 6 patients (12%) had ischemia in 3 vessels territories.
Collectively, ischemia within the left anterior descending artery (LAD) territory was present in 37 patients (74%), ischemia within the right coronary artery (RCA) territory was present in 24 patients (48%), and ischemia within the left circumflex artery (LCX) territory was present in 19 patients (38%).
Relation between the number of vessel territories affected and different parameters
Within the exercise group the increase in the number of vessel territories affected was related to the occurrence of left ventricular dilatation and the increase in lung thallium-201 uptake.
While within the dipyridamole group the increase in the number of vessel territories affected was related to the occurrence of left ventricular dilatation and the incidence and severity of chest pain during the test.
We postulated new score of positivity or significance of thallium results, the higher the score the more evidence of multivessel disease or significant lesions: Criteria or parameters used are:
Severity of chest pain 1 for mild, 2 for moderate, 3 for severe pain
LV dilatation 2 points
Lung uptake of thallium (denotes LV dysfunction) 2 points
ST depression >1 mm = 2 points
If one gets all parameters positive, his total score will be 9
Perfusion defects one vessel area = 2 point, 2 vessel areas = 4, 3 vessel areas= 6
We compared the score with the degree of perfusion defect; we found significant correlation between the measured parameters and the severity of perfusion defects <0.05 in both groups exercise and dipyridamole groups. This should not be unexpected as it is logic the severer the ischemia by perfusion the more the clinical (pain and ST depression) and more Thallium findings (LV dilatation and Lung Thallium uptake). In some patients there were more perfusion defects than the 4 parameters, in others more positive parameters than perfusion defects.
|
Total score |
||
|
rs |
p |
|
|
Perfusion defect degree |
0.457* |
0.001* |
Table 3: Exercise Correlation between total score and perfusion defect degree (n = 50)
rs: Spearman coefficient *: Statistically significant at p ≤ 0.05
|
Total score |
||
|
rs |
p |
|
|
Perfusion defect degree |
0.457* |
0.001* |
Table 4: Dipyridamole Correlation between total score and perfusion defect degree (n = 50)
rs: Spearman coefficient
*: Statistically significant at p ≤ 0.05
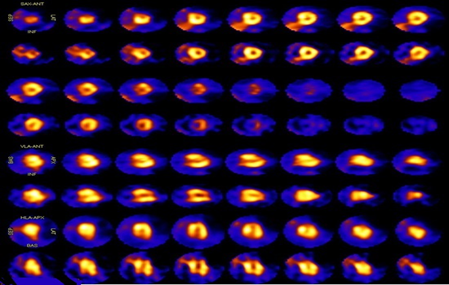
Figure 1: A 60 years old male patient presented to Alexandria university nuclear cardiology lab for assessment of class II chest pain. The patient was diabetic and had history of ischemic heart disease. The patient was not receiving any medications. The patient underwent exercise single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) using Bruce protocol. During the test, heart rate increased from 60 beats per minute to 146 beats per minute, systolic blood pressure increased from 130 mmHg to 150 mmHg, and diastolic blood pressure increased from 80 mmHg to 100 mmHg. Moderate chest pain and ECG changes occurred with stress. The test result showed ischemia in the left anterior descending (LAD) artery and the right coronary artery (RCA) territories, both left and right ventricle dilatation during rest that increased during stress, and no increased lung thallium-201 uptake. Our clinical score 2+2. Thallium score 2+2
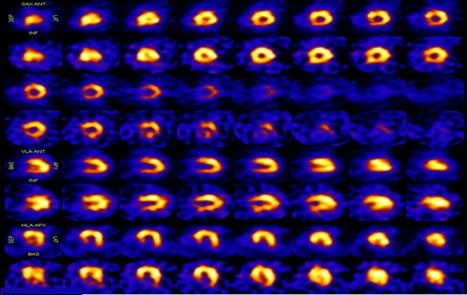
Figure 2: A 61 years old male patient presented to Alexandria university nuclear cardiology lab for assessment of class III chest pain and dyspnea. The patient was smoker and hypertensive. The patient was not receiving any medications. The patient underwent pharmacologic single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) using dipyridamole. During the test, heart rate increased from 69 beats per minute to 76 beats per minute, systolic blood pressure decreased from 140 mmHg to 130 mmHg, and diastolic blood pressure decreased from 90 mmHg to 80 mmHg. Severe chest pain and ECG changes occurred during the test which warranted the use of nitrate. The test result showed ischemia in the left anterior descending (LAD) artery, the right coronary artery (RCA), and the Left circumflex (LCX) artery territories, left ventricle dilatation during stress, and no increased lung thallium-201 uptake. Our clinical score 3+2+2; thallium score 2+2+2.
Discussion
Chest pain
In single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI), clinical studies report chest pain as either present or absent with no regard to its type, location, or degree [11,12].
In this study we applied the verbal rating scale (VRS) to assess chest pain during and after the test. Chest pain occurred in 56% of the exercise group compared to only 10% of the dipyridamole group. We found that exercise was associated with a statistically significant higher incidence and severity of chest pain compared to dipyridamole (χ2=24.350, MCp<0.001). The incidence and severity of chest pain were related to the number of vessel territories affected in the dipyridamole group (χ2=10.118, MCp=0.037), but not in the exercise group.
One study by Chow et al. comparing exercise and dipyridamole as modes of stress for Positron emission tomography (PET) myocardial perfusion imaging (MPI) within same group of patients found that chest pain was higher with dipyridamole (62%) compared with exercise (38%) [12].
In a study aimed to evaluate a combined exercise stress and dipyridamole stress protocol, Cortinas et al. compared 3 groups that underwent single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) using 3 different strategies for stress, namely, exercise only protocol, dipyridamole only protocol, or combined exercise and dipyridamole protocol and reported the occurrence of chest discomfort only in 10% of the cases of the dipyridamole only protocol group [13].
Electrocardiographic (ECG) changes
In this study we compared the incidence of electrocardiographic (ECG) changes between the exercise group and the dipyridamole group. Electrocardiographic (ECG) changes occurred in 64% of the exercise group compared to only 20% of the dipyridamole group. We found that exercise was associated with a statistically significant higher incidence of electrocardiographic (ECG) changes compared to dipyridamole (χ2=19.869, p<0.001). The incidence of electrocardiographic (ECG) changes was not related to the number of vessel territories affected in any of the 2 groups.
Chow et al. found that electrocardiographic (ECG) changes were higher with exercise (70%) compared with dipyridamole (30%) despite chest pain being higher with dipyridamole compared with exercise [12].
Left ventricular dilatation
In this study we compared the incidence of left ventricular dilatation between the exercise group and the dipyridamole group. Left ventricular dilatation occurred in 40% of the exercise group (out of which 16% had preexisting left ventricular dilatation that increased with stress) compared to 52% of the dipyridamole group (out of which 28% had preexisting left ventricular dilatation that increased with stress). There was no statistically significant difference in the incidence of left ventricular dilatation between the 2 groups. The incidence of left ventricular dilatation was related to the number of vessel territories affected in the exercise group (χ2=8.285, MCp=0.011) as well as the dipyridamole group (χ2=9.289, MCp=0.007).
In a study aimed to develop normal limits and evaluate diagnostic power of transient left ventricular dilatation Sestamibi, Xu et al. demonstrated an increase in transient left ventricular dilatation with the increase in coronary artery disease severity. Transient left ventricular dilatation occurred in 5% of subjects with insignificant coronary artery disease, 15% of subjects with moderate coronary artery disease, and more than 24% of subjects with severe coronary artery disease [14].
Hansen et al. evaluated the relationship between elevated lung/heart ratio (LHR) and transient left ventricular dilatation after exercise single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) and reported that transient left ventricular dilatation occurred in 7.8% of the subjects [15-18].
Increased lung thallium-201 uptake
In this study we compared the incidence of increased lung thallium-201 uptake between the exercise group and the dipyridamole group. Increased lung thallium-201 uptake occurred in 16% of the exercise group compared to 24% of the dipyridamole group. There was no statistically significant difference in the incidence of increased lung thallium-201 uptake between the 2 groups. The incidence of increased lung thallium-201 uptake was related to the number of vessel territories affected in the exercise group (χ2=7.817, MCp=0.017) but not in the dipyridamole group.
Choy and Leslie investigated increased lung uptake of technetium-99m Sestamibi during exercise, dipyridamole, or combined exercise/dipyridamole single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) and its relation to the severity of coronary artery disease (CAD) and reported no significant difference in lung/heart ratio (LHR) among the 3 groups. Additionally, lung/heart ratio (LHR) showed a positive correlation with the number of diseased vessels and the coronary artery disease severity score [19-22].
The mechanism of dipyridamole action is different and does not involve the myocardial ischemia process. Dipyridamole inhibits facilitated transport of adenosine into cells and thus increases extracellular endogenous adenosine level leading to coronary vasodilatation. However, dipyridamole may occasionally provoke myocardial ischemia by a steal effect, via collaterals from a low flow abnormal capillary bed into a high flow normal coronary territory and consequently may be associated with chest pain [10].
In general, chest pain and other ischemic parameters can be an indicator to the presence and the extent of ischemic heart disease.
In our study we postulated a new score that proved able to predict severity of thallium perfusion defects.
Conclusion
Despite having the same end result of achieving heterogenous perfusion between segments supplied by normal vessels and segments supplied by diseased vessels, exercise stress and vasodilator pharmacologic stress act through different mechanisms.
Occasional myocardial ischemia may develop during dipyridamole stress by steal effect via collaterals from a low flow abnormal capillary bed into a high flow normal coronary territory.
Myocardial ischemia is the cause of chest pain and electrocardiographic (ECG) changes during single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI). Left ventricular dilatation and increased lung thallium-201 uptake are related to the extent of myocardial ischemia.
Our new score of adding 4 parameters together was correlated with the severity of perfusion defects. These were 1-chest pain, 2-ECG changes, 3-Lung thallium uptake and 4- LV dilatation.
Conflict of interest:
None
Ethical standards:
Full consent was taken from patients, studies were done for benefit of the patient.
Funding:
none
References
- Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390 (2017):1260-1344.
- Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet 390 (2017): 1151-1210.
- Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388 (2016): 1459-1544.
- Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. NCHS Data Brief 43 (2010): 1–8.
- Hoorweg BB, Willemsen RT, Cleef LE, Boogaerts T, Buntinx F, Glatz JF, et al. Frequency of chest pain in primary care, diagnostic tests performed and final diagnoses. Heart 103 (2017): 1727-1732.
- Loong CY. Diagnosis of coronary artery disease by radionuclide myocardial perfusion imaging. Heart 90 (2004): 2–9.
- Anagnostopoulos C. Procedure guidelines for radionuclide myocardial perfusion imaging. Heart 90 (2004):1i–10.
- Arbit B, Azarbal B, Hayes SW, Gransar H, Germano G, Friedman JD, et al. Prognostic Contribution of Exercise Capacity, Heart Rate Recovery, Chronotropic Incompetence, and Myocardial Perfusion Single-Photon Emission Computerized Tomography in the Prediction of Cardiac Death and All-Cause Mortality. Am J Cardiol 116 (2015): 1678-1684.
- Salerno M, Beller GA. Noninvasive Assessment of Myocardial Perfusion. Circ Cardiovasc Imaging 2 (2009): 412-424.
- Sabharwal N, Arumugam P, Kelion A. Nuclear cardiology. Second edition. Oxford: Oxford University Press 2017: 293.
- Unal K, Akdemir O, Unlu M, Guner L. Clinical evaluation of the ACCF/ASNC appropriateness criteria for myocardial perfusion SPECT imaging. J Nucl Med 54 (2013): 1706–1706.
- Chow BJW, Ananthasubramaniam K, deKemp RA, Dalipaj MM, Beanlands RSB, Ruddy TD. Comparison of treadmill exercise versus dipyridamole stress with myocardial perfusion imaging using rubidium-82 positron emission tomography. J Am Coll Cardiol 45 (2005): 1227–1234.
- Cortinas IV, Beretta M, Alonso O, Mut F. New Exercise-Dipyridamole Combined Test for Nuclear Cardiology in Insufficient Effort: Appropriate Diagnostic Sensitivity Keeping Exercise Prognosis. Arq Bras Cardiol 105 (2015): 123-129.
- Xu Y, Arsanjani R, Clond M, Hyun M, Lemley M, Fish M, et al. Transient ischemic dilation for coronary artery disease in quantitative analysis of same-day sestamibi myocardial perfusion SPECT. J Nucl Cardiol 19 (2012): 465-473.
- Hansen CL, Sangrigoli R, Nkadi E, Kramer M. Comparison of pulmonary uptake with transient cavity dilation after exercise thallium-201 perfusion imaging. J Am Coll Cardiol 33 (1999):1323–1327.
- Kinoshita N, Sugihara H, Adachi Y, Nakamura T, Azuma A, Kohno Y, et al. Assessment of transient left ventricular dilatation on rest and exercise on Tc-99m tetrofosmin myocardial SPECT. Clin Nucl Med 27 (2002): 34–39.
- Rischpler C, Higuchi T, Fukushima K, Javadi MS, Merrill J, Nekolla SG, et al. Transient Ischemic Dilation Ratio in 82Rb PET Myocardial Perfusion Imaging: Normal Values and Significance as a Diagnostic and Prognostic Marker. J Nucl Med 53 (2012): 723-730.
- Chouraqui P, Rodrigues EA, Berman DS, Maddahi J. Significance of dipyridamole-induced transient dilation of the left ventricle during thallium-201 scintigraphy in suspected coronary artery disease. Am J Cardiol 66 (1990): 689–694.
- Choy JB, Leslie WD. Clinical correlates of Tc-99m sestamibi lung uptake. J Nucl Cardiol Off Publ Am Soc Nucl Cardiol 8 (2001): 639–644.
- Leslie WD, Tully SA, Yogendran MS, Ward LM, Nour KA, Metge CJ. Prognostic Value of Lung Sestamibi Uptake in Myocardial Perfusion Imaging of Patients With Known or Suspected Coronary Artery Disease. J Am Coll Cardiol 45 (2005): 1676–1682.
- Patel GM, Hauser TH, Parker JA, Pinto DS, Sanders GP, Aepfelbacher FC, et al. Quantitative relationship of stress Tc-99m sestamibi lung uptake with resting Tl-201 lung uptake and with indices of left ventricular dysfunction and coronary artery disease. J Nucl Cardiol Off Publ Am Soc Nucl Cardiol 11 (2004): 408–413.
- Georgoulias P, Tsougos I, Valotassiou V, Tzavara C, Xaplanteris P, Demakopoulos N. Long-term prognostic value of early post stress 99mTc-tetrofosmin lung uptake during exercise (SPECT) myocardial perfusion imaging. Eur Eur J Nucl Med Mol Imaging 37 (2010): 789-798.