A Comparative Study of Inflammatory Markers in Diabetics versus Non- Diabetics with Covid-19 and their Impact on Morbidity and Mortality Outcomes
Article Information
Vathul B Subramanian1*, Basavanagowdappa H2, Praveen Kulkarni3
1Department of General Medicine, JSS Medical College, JSS AHER, Mysore
2JSS Medical college, JSSAHER, Mysore
3Department of Community Medicine, JSSAHER, Mysore
*Corresponding author: Dr Vathul B Subramanian, Department of General medicine, JSS medical college, JSSAHER, Mysore.
Received: 11 May 2023; Accepted: 22 May 2023; Published: 10 August 2023
Citation: Vathul B Subramanian, Basavanagowdappa H, Praveen Kulkarni. A Comparative Study of Inflammatory Markers in Diabetics versus Non- Diabetics with Covid-19 and their Impact on Morbidity and Mortality Outcomes. Archives of Clinical and Biomedical Research. 7 (2023): 494-501.
Share at FacebookAbstract
Background and Aims: COVID-19 pandemic has been one of the most devastating public health emergency of 21st century. Diabetic patients tend to have a poorer prognosis compared to non-diabetics. In this study, we aimed to study the inflammatory markers (Ferritin, Lactate Dehydrogenase, C - reactive protein, Erythrocyte Sedimentation Rate, D-Dimer) in diabetics and non-diabetics with COVID-19 and their impact on morbidity and mortality.
Methods: This was a hospital-based combined retrospective and prospective study conducted among 1000 patients who presented with COVID-19 to a Tertiary Care Hospital in South India over a duration of 18 months from December 2020 to May 2022 after obtaining clearance from the institutional ethics committee and written informed consent from the study participants. They were divided into two groups-diabetics and nondiabetics. Their COVID and diabetes related morbidities were compared with the levels of their inflammatory markers like ESR, D-Dimer, Ferritin, LDH, CRP and IL-6.
Results: Among, 1000 subjects included in our study, 46% were diabetics. Males suffered the brunt of the disease (66%). Patients with higher HbA1c had more mortality (P value <.001). Diabetics had prolonged hospital stays, more oxygen requirement and a higher chance of requiring Non Invasive Ventilation (NIV) and mechanical ventilation. They also had more complications like acute respiratory distress syndrome (ARDS) ARDS, sepsis, acute kidney injury (AKI) and death. (P value 0.01 in all variables). Inflammatory markers like ESR, CRP, D-dimer, ferritin and LDH were compared between both groups. These markers were elevated irrespective of diabetic status and were elevated in all severe cases and its various complications like ventilator requirement and other COVIDrelated complications and death and these parameters were statistically significant.
Conclusions: Diabetics had a more adverse outcome in terms of complications and mortality in comparison to non-diabetics with COVID illness. Inflammatory markers like CRP, ESR, D-Dimer, ferritin and LDH were increased in both as the severity of COVID-19 increased indicating that it was an independent prognostic marker in itself.
Keywords
Inflammatory Markers; Diabetics; Non-Diabetics; Covid-19; Morbidity; Mortality
Article Details
1. Introduction
Emerging and re-emerging pathogens are global challenges for public health. Coronaviruses are enveloped RNA viruses that are distributed broadly among humans, other mammals, and birds and that cause respiratory, enteric, hepatic and neurological diseases. At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. It rapidly spread, resulting in an epidemic throughout China, followed by an increasing number of cases in other countries throughout the world. In February 2020, the World Health Organization designated the disease COVID-19, which stands for coronavirus disease 2019[1]. On 30th January, India reported its first case in Kerala, which rose to three cases by 3rd February; all were students returning from Wuhan. Since then, the world has undergone 4 waves, multiple variants of concerns and numerous lockdowns and restrictions since January 2020. The first wave of COVID-19 in India was till October 2020, following which the delta variant had taken the second wave in early 2021 with casualties in large numbers. The Omicron variant in early 2022 had been the major variant of concern during the third wave of this pandemic [2,3,4,5,6]. Vaccines of various pharmaceuticals have flooded the market and the way forward is even further coverage. Diabetes is a pro-inflammatory state and procoagulant state, and the proposed mechanism that cytokine storm is the reason for the oxidative damage and increased risk of thrombotic manifestations in COVID-19 patients. Early literature regarding the same has suggested that diabetic patients tend to have a poorer prognosis compared to non-diabetics in COVID-19 patients [7,8,9]. Inflammatory markers like CRP, D-Dimer, ESR and ferritin along with other markers of endothelial dysfunction and coagulation abnormalities like LDH and D-Dimer are proving to be vital tools for assessing prognosis and complications of COVID-19 viral disease.
2. Materials and Methods
This was a hospital-based combined retrospective and prospective study conducted among 1000 patients who presented with COVID-19 to a Tertiary Care Hospital in South India, over 18 months from December 2020 to May 2022. The study was started after obtaining clearance from the institutional ethics committee and written informed consent was obtained from the study participants.
2.1 Methods of Data Collection
For the retrospective part of the study, appropriate permission from the Medical Superintendent for using the in patient records of all the patients admitted for COVID-19 disease fulfilling the inclusion criteria was obtained. Written informed consent for the prospective participating patients was obtained after explaining the process as well as maintenance of confidentiality (with a cover letter). Voluntary participation and nonthreatening processes were ensured.
2.2 Inclusion Criteria:
- All patients tested positive for COVID-19 by RT PCR method.
- All patients who were above 18 years of age admitted in JSS Hospital, Mysore.
- All the patients whose inflammatory markers levels were measured. (CRP, D-Dimer, Ferritin, LDH and ESR)
- All Diabetic subjects who were either, known diabetic at the time of admission; Newly diagnosed with HbA1C greater than 6.5. The comparator group (Non Diabetics) were selected on the basis of not being diabetic based on history and FBA/PPBS values.
2.3 Exclusion Criteria
1) Those whose inflammatory parameter was not available in case records for retrospective participants
2) Patients whose glycemic status was not documented among retrospective participants
All the data sources which fulfilled the inclusion/exclusion criteria were enrolled in the study. The clinical and lab data of the patients from the study period were documented in a pretested preformat.
a. Patient’s data were divided into two arms-
- Non-Diabetics
- Diabetics
b. Initial values of inflammatory markers i.e.-D-DIMER, FERRITIN, LDH, CRP, and ESR and IL-6 were collected in both groups. The two groups were further assessed based on the following morbidity indicators-
Severity of illness was done with the help of AIIMS guidelines-
Mild disease- Upper respiratory tract symptoms with no hypoxia
Moderate Disease-Respiratory rate > 24/ Sp02 less than 94 % at room air
Severe Disease-Respiratory Rate >30 or Sp02 less than 90 % at room air
- Levels of Inflammatory markers like Ferritin, LDH, D-Dimer, CRP, ESR.
- Duration of Hospital stay
- 02 support- Oxygen/NIV/High flow nasal cannula
- Mechanical Ventilation
- Duration of ICU stay
- Acute complications like Diabetic Ketoacidosis and Hyperosmolar Hyperketotic Syndrome
- Age
- Gender
- Comparison with other comorbidities like Hypertension, Stroke, Hypothyroidism,
- Ischemic heart disease, Malignancy, Chronic Kidney Disease, Chronic Liver Disease, Chronic Obstructive Pulmonary Disease, Bronchial Asthma etc.
c. Covid 19 Complications-
- Sepsis and Secondary Bacterial Infection- Sepsis was defined by Severe inflammatory response syndrome criteria
- ARDS, Pulmonary embolism- Pulmonary
- Acute Coronary syndromes, Myocarditis, Cardiac Arrest-Cardiac
- Stroke
- AKI and AO CKD
- ACUTE LIVER DYSFUNCTION.
- Outcome criteria were determined as-
- Recovered- Discharged without oxygen.
- Partially Recovered- Discharged with home oxygen
2.4 Statistical Methods
Summary statistics were done using proportions for categorical/binary variables and mean, median, Standard deviation, Inter Quartile Range (IQR) for continuous variables. Inferential statistics were done by using the chi-square test, independent t-test, one-way ANOVA, Mann-Whitney test and Kruskal-Wallis test. All the statistical methods were done using SPSS 25.0 version for windows. P<0.05 was considered statistically significant. The chi-square test/Fisher exact test was used to compare two or more independent proportions. Fisher exact test is used when the expected numbers in >20% cells are<5. An Independent t-test was used to compare means between independent groups/mutually exclusive groups. One-way ANOVA was used to compare the difference in means between multiple independent groups. Mann-Whitney test was used to compare the continuous variables, which are not normally distributed, between two independent groups. Kruskal-Wallis test was used to compare the continuous variables, which are not normally distributed, between more than two independent groups.
3. Results
Out of the 1000 study population in our study, 66.6 % of the populations were males and the remaining were females, 460 were diabetics and 540 were non diabetics. Uncontrolled diabetics had more severe disease and more deaths in comparison to diabetics with good glycemic control. (P value 0.001- for all 3 values- Fasting Blood Sugar, Post Prandial Blood Sugar and HbA1c).
Table 1: Correlation between diabetic control and severity of COVID 19 illness
|
FBS |
PPBS |
HbA1c |
||
|
Severity |
Mild |
145 + 59 |
164.9 +81 |
7.8+1.7 |
|
Moderate |
165 + 65 |
200.8+98.7 |
8.5+2.0 |
|
|
Severe |
195 + 101 |
246.4+127.5 |
8.9+2.2 |
|
|
P Value |
|
0.001 |
0.001 |
0.001 |
|
Final outcome |
Expired |
205 +111 |
256.9+130 |
9.0+2.4 |
|
Partially Recovered |
220 +86 |
268.2+135 |
9.5+2.1 |
|
|
Recovered |
147 +55 |
171.4+80 |
8.0+1.7 |
|
|
P value |
|
0.001 |
0.001 |
0.001 |
A maximum number of individuals requiring ICU care were in the age group of 41-60 yrs. (43.4% n=218); while diabetics had a mean longer duration of stay in the age groups 41-80yrs, these were not statistically significant.
The mean duration of stay for diabetics (18.86) was greater than for non-diabetics. (17.54). This was albeit not a significant correlation.
Out of the other common comorbidities, hypertension constituted the most common comorbidity with 448 out of 1000 population suffering from it.
The most common symptom among both diabetics (85% n=390) and non-diabetics (84.7% n=458) was cough which was closely followed by fever which was a cumulative percentage of 70.9 %.
As shown in Table-2, Patients with diabetes had more oxygen requirement, NIV and needed mechanical ventilation with a significant P-value 0.001. Diabetic patients also suffered from sepsis, DKA, ARDS, PTE, ACS and acute CKD more than the non-diabetics which were statistically significant.
Out of 1000 patients, 137 patients had expired, 64.23 % out of them were diabetics and 35.76 % were non-diabetics which was statistically significant in comparison to non-diabetics (P-value 0.001).
Table 2: Comparing diabetics with non-diabetics in relation to morbidity and mortality indicators
|
Diabetics |
Non-Diabetics |
Total |
P-Value |
|
|
S.No |
N=460 |
N=540 |
||
|
Males |
303 (65.8 %) |
364 (67.3%) |
667 |
|
|
Females |
156 (33.9 %) |
177 (32. 7 %) |
333 |
|
|
Expired |
90 (19.5%) |
47 (8.7 %) |
137 |
0.001 |
|
Oxygen Requirment |
350 (76 %) |
327 (60%) |
677 |
0.001 |
|
NIV |
144 (31.3 %) |
60 (11.11%) |
204 |
0.001 |
|
MV |
75 (16.4 %) |
47 (8.7%) |
122 |
0.001 |
|
Sepsis |
113 (24.5%) |
47 (8.7%) |
160 |
0.001 |
|
ARDS |
229 (49.7%) |
115 (21.3%) |
344 |
0.001 |
|
PTE |
13 (2.82%) |
4 (0.74%) |
17 |
0.01 |
|
ACS |
14 (2.6 %) |
3 (0.56 %) |
17 |
0.01 |
|
AKI/Acute on CKD |
53 (11.5 %) |
15 (2.78%) |
68 |
0.01 |
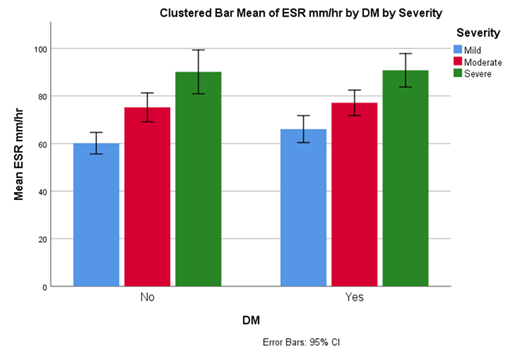
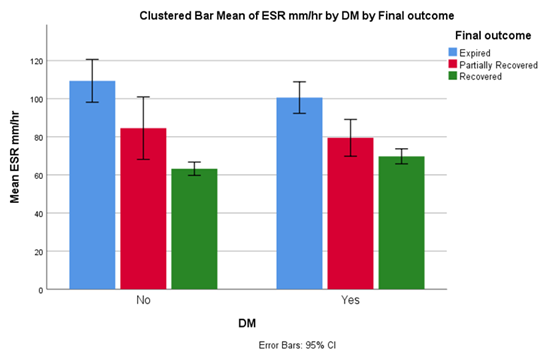
Figures 1 and Figure 2 depict ESR as an inflammatory marker which was elevated in severe COVID 19 patients and patients who succumbed to the illness in both groups.
Tables 3-6 studied the impact of CRP, D-Dimer, LDH and ferritin in both groups suffering from COVID 19. Their final outcomes, requirement of oxygen and assisted ventilation and complications like sepsis, ARDS, AKI/acute on CKD were studied and the inflammatory markers were elevated in both groups when they had a severe disease, required assisted ventilation and when they had the aforementioned complications and this was a statistically significant association.
Table 3: Comparison of median CRP between diabetics and non-diabetics
|
Non Diabetic |
Diabetic |
||
|
Severity |
Mild |
19.0(4.5-52) |
24.0(8.1-53) |
|
Moderate |
52.7(21.7-85.6) |
60.2(27-113.8) |
|
|
Severe |
79.9(27.4-191.4) |
108.0(64.7-188) |
|
|
Final outcome |
Expired |
117.0(59.4-209) |
131.3(78.8-194.4) |
|
Recovered |
26.0(6.3-66) |
37.0(13.6-96.1) |
|
|
NIV |
No |
28.7(7.0-68.9) |
38.0(14-96.1) |
|
Yes |
99.5(40.7-200.7) |
98.7(49.3-147.5) |
|
|
MV |
No |
28.7(7.3-68.9) |
41.0(16-100) |
|
Yes |
173.0(55-217) |
132.0(83.2-200) |
|
|
Sepsis |
No |
29.3(7.3-69) |
40.0(15.4-99) |
|
Yes |
140.0(52-209) |
109.1(65-161) |
|
|
ARDS |
No |
24.0(6.2-61.6) |
35.8(15.4-93) |
|
Yes |
75.0(33.4-160) |
81.0(33-138) |
|
|
AKI/Acute on CKD |
No |
32.3(8.2-75) |
48.0(19.1-110) |
|
Yes |
174.5(26.2-209) |
99.7(56-152) |
|
|
P value |
0.001 |
0.001 |
|
Table 4: Comparison of Median D-dimer between diabetics and non-diabetics
|
Non Diabetics |
Diabetics |
||
|
Severity |
Mild |
0.3(0.2-0.7) |
0.4(0.2-0.8) |
|
Moderate |
0.4(.2-.8) |
0.5(0.3-0.8) |
|
|
Severe |
0.5(0.2-1.0) |
0.6(0.4-1.9) |
|
|
Final outcome |
Expired |
1.2(0.6-2.8) |
0.6(0.4-1.5) |
|
Recovered |
0.3(0.2-0.6) |
0.4(0.2-0.8) |
|
|
NIV |
No |
0.3(0.2-0.8) |
0.4(0.3-0.8) |
|
Yes |
0.6(0.4-0.9) |
0.5(0.3-1.6) |
|
|
MV |
No |
0.3(0.2-0.7) |
0.4(0.3-0.8) |
|
Yes |
0.9(0.7-2.4) |
0.8(0.4-2) |
|
|
Sepsis |
No |
0.3(0.2-0.7) |
0.4(0.3-0.8) |
|
Yes |
0.9(0.4-1.8) |
0.6(0.3-1.7) |
|
|
ARDS |
No |
0.3(0.2-0.7) |
0.4(0.3-0.8) |
|
Yes |
0.6(.3-1.2) |
0.5(0.3-1.2) |
|
|
AKI/Acute on CKD |
No |
0.4(0.2-0.8) |
0.5(0.3-0.8) |
|
Yes |
1.8(0.3-2.6) |
0.6(0.4-2.3) |
|
|
P-Value |
0.001 |
0.001 |
|
Table 5: Comparison of median LDH between diabetics and non-diabetics
|
Non Diabetics |
Diabetics |
||
|
Severity |
Mild |
253.0(185-399) |
263.5(198-350) |
|
Moderate |
293.0(215.5-453.5) |
306.0(211-453) |
|
|
Severe |
363.0(237-580) |
380.0(245-540) |
|
|
Final outcome |
Expired |
454.0(322-705) |
433.0(250-564.7) |
|
Recovered |
256.0(192-405) |
287.0(201-394.5) |
|
|
NIV |
No |
258.0(192-420) |
287.0(201-404) |
|
Yes |
368.0(264-737) |
355.5(235-490.7) |
|
|
MV |
No |
260.5(198.5-414.5) |
288.0(209.5-432) |
|
Yes |
441.8(266-580) |
438.0(253-542) |
|
|
Sepsis |
No |
257.5(196-411.5) |
290.0(206-443.7) |
|
Yes |
453.0(302-769) |
344.0(224-489.3) |
|
|
ARDS |
No |
252.5(179-407) |
280.0(198-430) |
|
Yes |
347.0(245-488) |
331.0(227-479) |
|
|
AKI/Acute on CKD |
No |
265.0(202-434) |
290.0(210-440) |
|
Yes |
721.0(332-1005) |
438.0(253-844.5) |
|
|
P-Value |
0.001 |
0.001 |
|
Table 6: Comparison of Median ferritin between diabetics and non-diabetics
|
Non Diabetics |
Diabetics |
||
|
Severity |
Mild |
245.0(142-432) |
302.0(164-534.6) |
|
Moderate |
368.0(242-606) |
383.8(221-687) |
|
|
Severe |
501.0(306-680) |
570.9(359-1102) |
|
|
Final outcome |
Expired |
560.0(258-1096) |
602.0(351.7-1193) |
|
Recovered |
286.5(170.5-475.5) |
353.0(211.7-596.7) |
|
|
NIV |
No |
295.5(172.4-496) |
351.0(208-565) |
|
Yes |
491.5(251.5-795.5) |
570.5(313-1008.5) |
|
|
MV |
No |
299.0(182-504) |
368.5(219-643) |
|
Yes |
475.0(234-834) |
537.0(342-1240) |
|
|
Sepsis |
No |
294.0(173-498) |
362.0(219-638) |
|
Yes |
535.0(305-947) |
487.0(306-1012) |
|
|
ARDS |
No |
292.5(172.8-468) |
334.0(210-537) |
|
Yes |
456.0(215-742) |
462.0(279-873) |
|
|
AKI/Acute on CKD |
No |
300.0(182-511) |
373.0(221-648) |
|
Yes |
647.0(452-1159) |
565.0(341.6-1240) |
|
|
P-Value |
0.001 |
0.001 |
|
4. Discussion
Our study was a cross sectional study where brunt of the disease was suffered by males. Studies have shown that this could due to an altered immune response in males. In our study, a total of 677 individuals required oxygen. 51.69% of them were diabetics. (P value-<0.001) Out of the 204 people requiring non-invasive ventilation, 70 % (144) patients were diabetics (P value 0.001). Out of 122 patients requiring mechanical ventilation, 75 patients were diabetics. (61.4 %) (P value 0.001)
In a study by begum et al, diabetics using oxygen 77% and 57.7% required ICU care. The main reasons for this could be the cytokine storm and the increased expression of ACE receptors in diabetics, which has been postulated [10]. Diabetes and related complications like diabetic ketoacidosis (DKA) were common in COVID illness. Since many of the patients were on high-dose steroids and were already in a preexisting immune compromised state, managing glycaemia was a challenge in COVID settings. Even out of the previous non-diabetics, 5.7 % of the individuals developed DKA and 28 % of the diabetics had DKA (P value <0.001). In a systematic review, 77% of patients with COVID-19 who developed ketoacidosis had T2DM [11,12]. Studies have shown that levels of glucose in monocytes have proven to be an important factor in virus expression and multiplication which leads to a dysregulated immune response [13,14]. COVID-19 viral disease also had a set of other complications like acute respiratory distress syndrome, sepsis, prothrombotic states like pulmonary thromboembolism, acute coronary syndrome, acute kidney injury and worsening of preexisting kidney disease. Out of 160 patients who had suffered from sepsis, 70 % were diabetics (P-value 0.001). 50 percent of all diabetic patients had suffered from ARDS as opposed to non-diabetics where it was seen only 21 % of them suffered from ARDS. (P-value 0.01). COVID-19 being a procoagulant state, pulmonary thromboembolism was seen in 1.7 % of our study population and 13 of these individuals were diabetic. (P value0.01) Similar significant patterns were seen in patients suffering from acute coronary syndrome and acute chronic kidney disease respectively. (P value of 0.002, 0.001) In a study done by Begum et al, ARDS, acute cardiac injury, acute kidney injury, acute liver injury and incidence of secondary infection were compared between diabetics and non-diabetics. In this study, diabetics suffered more often with ARDS, AKI, Acute cardiac injury and acute liver injury with a significant p-value. Our study primarily focused on inflammatory markers and their role in predicting outcomes in COVID-19 viral disease. Cytokine storm is the major contributing factor for the various outcomes in COVID illness and inflammatory markers were a gateway for understanding the nature of the disease. ESR is a commonly used test in our day-to-day practice and it had a significant role in understanding the inflammatory pattern of COVID-19. This study showed that as the severity increased, ESR values were elevated irrespective of diabetic or non-diabetic status. In both groups, the inflammatory markers correlated with the severity of the disease and the P values were significant. (0.001) A similar picture was seen when we compared the people who expired (P 0.001 in both groups). This was an interesting observation as we hypothesized that diabetics would have a more significant rise in ESR when compared to non-diabetics, our study showed that irrespective of diabetic status, ESR was elevated in COVID illness when the patient developed complications. Our study also compared other markers like procalcitonin, D-dimer, ferritin, CRP and LDH which are all documented important markers of inflammation in COVID-19 viral pneumonia. Our study showed that these inflammatory markers were elevated irrespective of diabetic and non-diabetic status. The inflammatory markers were significantly elevated and were well correlated with parameters like severity, the requirement of oxygen, mechanical ventilation, non-invasive ventilation, and mortality outcomes. While looking at complications, the most commonly encountered ones in our study were ARDS, sepsis and AKI/acute on CKD. These complications were seen to have a significant increase in the markers mentioned above showing that diabetes alone did not have an impact on the severity of the disease. A meta-analysis by Zeng et all done in China also compared inflammatory markers between severe and non-severe COVID-19 cases. They compared markers like CRP, Procalcitonin, IL-6, ESR and serum ferritin and found that these markers were elevated in severe disease manifestation [15]. In a study done by Guo et all, which compared inflammatory markers in diabetics and non-diabetics, they found that CRP, D- Dimer, and ESR were elevated in diabetics with statistical significance. IL-6 and serum ferritin levels were not significantly elevated [16].
In a study done by Naveen Kumar, which was done in India, showed that diabetics had elevated levels of inflammatory markers in comparison to non-diabetics which was in contrast to our study which showed that elevated levels of inflammatory markers were independent of diabetic status [17]. While IL-6 is a major cytokine involved in the pathogenesis of COVID-19 viral disease and cytokine storm, all our subjects could not get IL-6 levels done to study the effects of its levels and this is one of the drawbacks of the study
All in all, our study which was done in a tertiary care center showed that COVID-19 was more common among the middle-aged population. Males suffered the brunt of the disease. Diabetics suffered adverse outcomes in comparison to non-diabetics and uncontrolled diabetics had a worse outcome in comparison with controlled diabetics. Although diabetics had a more severe disease course, inflammatory markers in both groups were elevated on par with the disease severity of COVID illness. The major complications seen in our study were ARDS, sepsis and acute CKD. Other complications were few and far in between and much could not be analyzed for the same.
5. Conclusion:
Diabetics had more adverse outcomes in terms of complications and mortality when compared to non-diabetics. Inflammatory markers like CRP, ESR, D-Dimer, ferritin and LDH were increased in both diabetics and non-diabetics as the severity of COVID-19 increased.
Limitation of the study
Interleukin-6 is an important cytokine in the pathogenesis of the COVID illness, levels of which could have been a potent prognostic marker was not sufficiently represented in our study.
Computed tomography was another prognostic marker of which was used extensively during the pandemic to understand the nature of the disease. Computed tomography was not routinely done in all cases in our study and hence its impact could not be assessed in our study.
Acknowledgements:
We would like to thank the Department of General medicine, JSS Hospital, Mysore and the medical records department of JSS Hospital, Mysore to conduct this study.
Conflicts of Interest:
Nil
References:
- World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV (2020).
- Li B, Deng A, Li K, et al. Viral infection and transmission in a large, well-traced outbreak caused by the SARS-CoV-2 Delta variant. Nature Com 460 (2022).
- Ong SWX, Chiew CJ, AngLW, et al. Clinical and virological features of SARS-CoV-2 variants of concern: a retrospective cohort study comparing B.1.1.7 (Alpha), B.1.315 (Beta), and B.1.617.2 (Delta). Clin Infect Dis 75 (2022): 1128-1136.
- Sheikh A, McMenamin J, Taylor B, et al. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 397 (2021): 2461.
- Twohig KA, Nyberg T, Zaidi A, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis 22 (2022): 35-42.
- Fisman DN, Tuite AR. Evaluation of the relative virulence of novel SARS-CoV-2 variants: a retrospective cohort study in Ontario, Canada. CMAJ 193 (2021): 1619.
- Carey IM. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care 41 (2018): 513-521.
- Wu C. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med 180 (2020): 934-943.
- Critchley JA. Glycemic control and risk of infections among people with type 1 or type 2 diabetes in a large primary care cohort study. Diabetes Care 41 (2018): 2127-2135.
- Begum F, Barman M, Jahir ET. Markers of coagulation dysfunction and inflammation in diabetic and non- diabetic covid-19 patients- a retrospective study. Journal of Clinical and Diagnostic Research 16 (2022): 12-16.
- Gianchandani R. Managing hyperglycemia in the COVID-19 inflammatory storm. Diabetes 69 (2020): 2048-2053.
- Pal R, Banerjee M, Yadav U, et al. Clinical profile and outcomes in COVID-19 patients with diabetic ketoacidosis: a systematic review of literature. Diabetes Metab. Syndr 14 (2020): 1563-1569.
- Carey IM. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care 41 (2018): 513-521.
- Wu C. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med 180 (2020): 934-943.
- Furong Zeng, Yuzhao Huang, Ying Guo, et al. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis 96 (2020): 467-474.
- Weina Guo, Mingyue Li, Yalan Dong, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev 36 (2020): 3319.
- Naveen M, Harmeet PSD, Saurabh A, et al. The Effect of Diabetes Mellitus on Outcomes of Patients Admitted with COVID-19: A Single - Center Experience from a Tertiary Hospital in India. Indian J Endocrinol Metlab 26 (2022): 376-383.