A Case of Subdural Haemorrhage Following a Trivial Fall - A Case Report
Article Information
Navin Kumar Devaraj*
Department of Family Medicine, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia
*Corresponding author: Navin Kumar Devaraj, Department of Family Medicine, Faculty of Medicine and Health Sciences, University Putra Malaysia, 43400 Serdang, Selangor, Malaysia
Received: 01 September 2019; Accepted: 20 September 2019; Published: 23 September 2019
Citation:
Navin Kumar Devaraj. A Case Of Subdural Haemorrhage Following A Trivial Fall- A Case Report. Archives of Internal Medicine Research 2 (2019): 030-033.
Share at FacebookAbstract
Mr. A initially presented with history of right sided headache for 2 weeks. He had a history of hitting his head against the floor after slipping from the last step of home stairs, but was well till this onset of headache. Computed tomography done showed right temporo-parietal subdural haemorrhage measuring 1.3 cm with a midline shift of 0.7 cm. Burr hole evacuation was done and he is currently recovering well.
Keywords
Subdural Haemorrhage; Chronic; Fall; Headache; Burr Hole
Subdural Haemorrhage articles Subdural Haemorrhage Research articles Subdural Haemorrhage review articles Subdural Haemorrhage PubMed articles Subdural Haemorrhage PubMed Central articles Subdural Haemorrhage 2023 articles Subdural Haemorrhage 2024 articles Subdural Haemorrhage Scopus articles Subdural Haemorrhage impact factor journals Subdural Haemorrhage Scopus journals Subdural Haemorrhage PubMed journals Subdural Haemorrhage medical journals Subdural Haemorrhage free journals Subdural Haemorrhage best journals Subdural Haemorrhage top journals Subdural Haemorrhage free medical journals Subdural Haemorrhage famous journals Subdural Haemorrhage Google Scholar indexed journals Chronic articles Chronic Research articles Chronic review articles Chronic PubMed articles Chronic PubMed Central articles Chronic 2023 articles Chronic 2024 articles Chronic Scopus articles Chronic impact factor journals Chronic Scopus journals Chronic PubMed journals Chronic medical journals Chronic free journals Chronic best journals Chronic top journals Chronic free medical journals Chronic famous journals Chronic Google Scholar indexed journals Fall articles Fall Research articles Fall review articles Fall PubMed articles Fall PubMed Central articles Fall 2023 articles Fall 2024 articles Fall Scopus articles Fall impact factor journals Fall Scopus journals Fall PubMed journals Fall medical journals Fall free journals Fall best journals Fall top journals Fall free medical journals Fall famous journals Fall Google Scholar indexed journals Headache articles Headache Research articles Headache review articles Headache PubMed articles Headache PubMed Central articles Headache 2023 articles Headache 2024 articles Headache Scopus articles Headache impact factor journals Headache Scopus journals Headache PubMed journals Headache medical journals Headache free journals Headache best journals Headache top journals Headache free medical journals Headache famous journals Headache Google Scholar indexed journals Burr Hole articles Burr Hole Research articles Burr Hole review articles Burr Hole PubMed articles Burr Hole PubMed Central articles Burr Hole 2023 articles Burr Hole 2024 articles Burr Hole Scopus articles Burr Hole impact factor journals Burr Hole Scopus journals Burr Hole PubMed journals Burr Hole medical journals Burr Hole free journals Burr Hole best journals Burr Hole top journals Burr Hole free medical journals Burr Hole famous journals Burr Hole Google Scholar indexed journals seizures articles seizures Research articles seizures review articles seizures PubMed articles seizures PubMed Central articles seizures 2023 articles seizures 2024 articles seizures Scopus articles seizures impact factor journals seizures Scopus journals seizures PubMed journals seizures medical journals seizures free journals seizures best journals seizures top journals seizures free medical journals seizures famous journals seizures Google Scholar indexed journals hypertension articles hypertension Research articles hypertension review articles hypertension PubMed articles hypertension PubMed Central articles hypertension 2023 articles hypertension 2024 articles hypertension Scopus articles hypertension impact factor journals hypertension Scopus journals hypertension PubMed journals hypertension medical journals hypertension free journals hypertension best journals hypertension top journals hypertension free medical journals hypertension famous journals hypertension Google Scholar indexed journals Neurological articles Neurological Research articles Neurological review articles Neurological PubMed articles Neurological PubMed Central articles Neurological 2023 articles Neurological 2024 articles Neurological Scopus articles Neurological impact factor journals Neurological Scopus journals Neurological PubMed journals Neurological medical journals Neurological free journals Neurological best journals Neurological top journals Neurological free medical journals Neurological famous journals Neurological Google Scholar indexed journals cranial nerves articles cranial nerves Research articles cranial nerves review articles cranial nerves PubMed articles cranial nerves PubMed Central articles cranial nerves 2023 articles cranial nerves 2024 articles cranial nerves Scopus articles cranial nerves impact factor journals cranial nerves Scopus journals cranial nerves PubMed journals cranial nerves medical journals cranial nerves free journals cranial nerves best journals cranial nerves top journals cranial nerves free medical journals cranial nerves famous journals cranial nerves Google Scholar indexed journals cerebellar articles cerebellar Research articles cerebellar review articles cerebellar PubMed articles cerebellar PubMed Central articles cerebellar 2023 articles cerebellar 2024 articles cerebellar Scopus articles cerebellar impact factor journals cerebellar Scopus journals cerebellar PubMed journals cerebellar medical journals cerebellar free journals cerebellar best journals cerebellar top journals cerebellar free medical journals cerebellar famous journals cerebellar Google Scholar indexed journals
Article Details
1. Introduction
Chronic subdural haemorrhage (SDH) is known to occur spontaneously in older individuals, with or without a history of falls. It typically presents with headache, seizures, syncope, altered mental state and extra pyramidal symptoms for e.g. dystonia and dyskinesia [1]. Risk factors for subdural haemorrhage include older male, presence of medical problem, including diabetes, hypertension and atrial fibrillation, intake of oral anti-platelets or anti-coagulant therapy and history of falls [2]. Diagnosis requires a high index of suspicion based on the clinical presentation, as sometimes the patient may not reveal that they had any trauma unless asked specifically. Computed tomography or magnetic resonance imaging of the brain is needed for diagnosis depending on the size of the bleeding. The former is able to delineate larger bleeds, especially those with middling shift, but the latter will be needed for smaller collection of haematoma [1].
2. Case Report
Mr A, a 50 year old man, works as a car mechanic. Pre-morbidly, he had hypertension well controlled on perindopril 8 mg daily and amlodipine 10 mg daily. One fine day after waking up from sleep, he suddenly developed a dull aching headache over his right temporal region that had persisted for the past 2 weeks with pain score of 3-7/10. There was no vomiting, dizziness or blurring of vision. He had severe headaches before, but none as long as this current episode or in this specific region. When asked, he recalled falling on the right side of his scalp 3 months ago when he accidentally missed the last step of his home, which just cause him some mild swelling which he treated on his own with ice compression and the swelling then spontaneously resolved.
On physical examination, Mr A repeatedly was holding the right side of his scalp during the consultation. His blood pressure (sitting) was 146/82 and 142/80 mmHg (standing). The pulse rate was 74 beats per minute, regularly regular with a temperature of 36.8°C. Neurological examination, including the cranial nerves and cerebellar signs examination was normal. Gait was normal. The Romberg test was negative. A provisional diagnosis of possible stroke or space occupying lesion was made. Case was referred for urgent non- contrast computed tomography of the brain, which noted showed right temporo-parietal subdural haemorrhage measuring 1.3 cm with a left midline shift of 0.7 cm (Figure A and B). The radiologist proceeded with magnetic resonance imaging of the brain, which confirmed the above findings.Case was referred to the neurosurgery team, which conducted an urgent burr hole surgery Subsequently Mr A was warded in the neurosurgical ward where he made an uneventful recovery. He was discharged after 5 days of undergoing the emergency burr hole surgery. His blood pressure in the ward was normal.
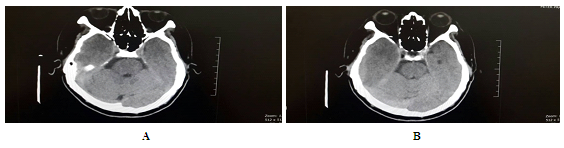
Figure 1A and 1B: Tomography of the brain, which noted showed right temporo-parietal subdural haemorrhage.
3. Discussion
Urgent evacuation is usually done in cases of subdural haemorrhage with either a single or two burr hole craniostomy or craniotomy [1, 3]. There is no difference in term of prognosis following treatment with either first two methods of craniostomy [3]. The craniotomy surgical procedure is usually reserved as a second line procedure for cases of recurrence and for patients that have ‘hard to evacuate’ solid haematoma [1]. The excess mortality risk following chronic subdural haemorrhage persists throughout life. Factors determining this risk of mortality will include the degree of disability or dependence upon discharge and the presence of cerebral atrophy medical risk factors like stroke and hypertension [2]. In those having risk factors like hypertension, diabetes and dyslipidaemia, adherence to medication is important to prevent the complication of subdural haemorrhage [4-6].
In summary, this was a case of chronic subdural haemorrhage that presented in a 50 year old man with only trivial symptoms of right sided headache and a history of fall three months prior to the development of the headache. It needed a high index of suspicion and investigation with a computed tomography of the brain to reach the diagnosis of intracranial haemorrhage before urgent burr hole surgery was done.
Acknowledgement
The author like to thank Mr A for his permission to publish this case.
Conflict of interest
The author declares no conflict of interest
References
- Sangondimath G, Chhabra HS, Venkatesh R, et al. A rare case of chronic subdural haematoma presenting with paraparesis: A case report and review of literature. Journal of Clinical Orthopaedics and Trauma 6 (2015): 265-268.
- Manickam A, Marshman LAG, Johnston R. Long-term survival after chronic subdural haematoma. Journal of Clinical Neuroscience 34 (2016): 100-104.
- Smith MD, Kishikova L, Norris JM. Surgical management of chronic subdural haematoma: One hole or two?. International Journal of Surgery 10 (2012): 450-452.
- Chia YC, Ching SM, Chew BN, et al. May Measurement Month 2017 blood pressure screening: findings from Malaysia-South-East Asia and Australasia. European Heart Journal Supplements 21 (2019): D77-D79.
- Rashid AA, Devaraj NK. Oh no! now I have diabetes. Rawal Medical Journal 43 (2018): 776-778.
- Devaraj NK. Prevalence, Factors Influencing, and Knowledge About Adherence to Lipid-Lowering Therapy Among Hyperlipidemia Patients. International Journal of Cardiology 249 (2017): S7-S8.
