A Case of Fulminant Type Community-Acquired Pneumonia Found to be Caused by Pseudomonas aeruginosa at Autopsy
Article Information
Mina Furumido1, Kei Takamura1*, Sho Nakakubo1, Hajime Kikuchi1, Makoto Yamamoto1, Keisuke Kikuchi2
1Department of Internal Medicine, Obihiro Kosei General Hospital, Obihiro, Japan
2Department of Diagnostic Pathology, Obihiro Kosei General Hospital, Obihiro, Japan
*Corresponding Author: Dr. Kei Takamura, Department of Internal Medicine, Obihiro Kosei General Hospital, Obihiro, Japan
Received: 04 August 2019; Accepted: 13 August 2019; Published: 14 November 2019
Citation: Furumido M, Takamura K, Nakakubo S, Kikuchi H, Yamamoto M, Kikuchi K. A Case of Fulminant Type Community-Acquired Pneumonia Found to be Caused by Pseudomonas aeruginosa at Autopsy. Archives of Clinical and Medical Case Reports 3 (2019): 451-456.
Share at FacebookAbstract
The present case involved a 27-year-old woman, who presented to a nearby physician with chief complaints of fever and dyspnea and hospitalized with a diagnosis of right lobar pneumonia on the same day. The patient was treated with antibiotics (aminobenzylpenicillin/sulbactam); however, exacerbation of respiratory status occurred with hypotension, and she was transferred to the authors’ hospital under tracheal intubation. The right superior lobe exhibited a wide range of infiltrative shadows with air bronchograms. Vasopressor and continuous hemodiafiltration were initiated to address overall exacerbation, and antibiotics (ciprofloxacin) were added. However, ventilation could not be maintained due to the large quantity of respiratory secretions; consequently, extracorporeal membrane oxygenation (ECMO) was initiated 5 h after admission to the intensive care unit. Due to the large quantity of Gram-negative bacilli confirmed by gram stain of respiratory secretions, amikacin was added. Although oxygenation was improved after initial ECMO induction, the patient died on day 2 of admission, despite being revived from sudden cardiac arrest. Pseudomonas aeruginosa was detected in respiratory secretions, blood cultures, and all lung tissues at autopsy, and the illness was believed to be a fulminant form of community-acquired pneumonia caused by the organism. This is a rare case and autopsy finding and, as such, contributes to the scarce literature.
Keywords
Pseudomonas aeruginosa; Fulminant community-acquired pneumonia; Autopsy
Pseudomonas aeruginosa articles, Fulminant community-acquired pneumonia articles, Autopsy articles
Pseudomonas aeruginosa articles Pseudomonas aeruginosa Research articles Pseudomonas aeruginosa review articles Pseudomonas aeruginosa PubMed articles Pseudomonas aeruginosa PubMed Central articles Pseudomonas aeruginosa 2023 articles Pseudomonas aeruginosa 2024 articles Pseudomonas aeruginosa Scopus articles Pseudomonas aeruginosa impact factor journals Pseudomonas aeruginosa Scopus journals Pseudomonas aeruginosa PubMed journals Pseudomonas aeruginosa medical journals Pseudomonas aeruginosa free journals Pseudomonas aeruginosa best journals Pseudomonas aeruginosa top journals Pseudomonas aeruginosa free medical journals Pseudomonas aeruginosa famous journals Pseudomonas aeruginosa Google Scholar indexed journals aeruginosa articles aeruginosa Research articles aeruginosa review articles aeruginosa PubMed articles aeruginosa PubMed Central articles aeruginosa 2023 articles aeruginosa 2024 articles aeruginosa Scopus articles aeruginosa impact factor journals aeruginosa Scopus journals aeruginosa PubMed journals aeruginosa medical journals aeruginosa free journals aeruginosa best journals aeruginosa top journals aeruginosa free medical journals aeruginosa famous journals aeruginosa Google Scholar indexed journals Fulminant community-acquired pneumonia articles Fulminant community-acquired pneumonia Research articles Fulminant community-acquired pneumonia review articles Fulminant community-acquired pneumonia PubMed articles Fulminant community-acquired pneumonia PubMed Central articles Fulminant community-acquired pneumonia 2023 articles Fulminant community-acquired pneumonia 2024 articles Fulminant community-acquired pneumonia Scopus articles Fulminant community-acquired pneumonia impact factor journals Fulminant community-acquired pneumonia Scopus journals Fulminant community-acquired pneumonia PubMed journals Fulminant community-acquired pneumonia medical journals Fulminant community-acquired pneumonia free journals Fulminant community-acquired pneumonia best journals Fulminant community-acquired pneumonia top journals Fulminant community-acquired pneumonia free medical journals Fulminant community-acquired pneumonia famous journals Fulminant community-acquired pneumonia Google Scholar indexed journals pneumonia articles pneumonia Research articles pneumonia review articles pneumonia PubMed articles pneumonia PubMed Central articles pneumonia 2023 articles pneumonia 2024 articles pneumonia Scopus articles pneumonia impact factor journals pneumonia Scopus journals pneumonia PubMed journals pneumonia medical journals pneumonia free journals pneumonia best journals pneumonia top journals pneumonia free medical journals pneumonia famous journals pneumonia Google Scholar indexed journals Autopsy articles Autopsy Research articles Autopsy review articles Autopsy PubMed articles Autopsy PubMed Central articles Autopsy 2023 articles Autopsy 2024 articles Autopsy Scopus articles Autopsy impact factor journals Autopsy Scopus journals Autopsy PubMed journals Autopsy medical journals Autopsy free journals Autopsy best journals Autopsy top journals Autopsy free medical journals Autopsy famous journals Autopsy Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals ECMO articles ECMO Research articles ECMO review articles ECMO PubMed articles ECMO PubMed Central articles ECMO 2023 articles ECMO 2024 articles ECMO Scopus articles ECMO impact factor journals ECMO Scopus journals ECMO PubMed journals ECMO medical journals ECMO free journals ECMO best journals ECMO top journals ECMO free medical journals ECMO famous journals ECMO Google Scholar indexed journals cardiac articles cardiac Research articles cardiac review articles cardiac PubMed articles cardiac PubMed Central articles cardiac 2023 articles cardiac 2024 articles cardiac Scopus articles cardiac impact factor journals cardiac Scopus journals cardiac PubMed journals cardiac medical journals cardiac free journals cardiac best journals cardiac top journals cardiac free medical journals cardiac famous journals cardiac Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals pulmonary articles pulmonary Research articles pulmonary review articles pulmonary PubMed articles pulmonary PubMed Central articles pulmonary 2023 articles pulmonary 2024 articles pulmonary Scopus articles pulmonary impact factor journals pulmonary Scopus journals pulmonary PubMed journals pulmonary medical journals pulmonary free journals pulmonary best journals pulmonary top journals pulmonary free medical journals pulmonary famous journals pulmonary Google Scholar indexed journals
Article Details
1. Case presentation
The patient was a 27-year-old woman who developed a fever 2 days before hospital consultation and received a prescription for an antipyretic analgesic by a nearby physician and sent home. However, because dyspnea appeared on the day before consultation, the hospital was consulted, and it was hospitalization by a diagnosis of the right lobar pneumonia in an image in the hospital. Although she was treated with antibiotics (aminobenzylpenicillin [ABPC]/sulbactam [SBT]), her respiratory status became exacerbated, with a rapid reduction in blood pressure. She was transferred to the authors’ hospital after intubation in the middle of the night.
The patient was a beautician, with a medical history of untreated, intermittent bronchial asthma. She smoked 20 cigarettes per day, but had no history of alcohol consumption or allergies, nor a history of bird exposure, hot-spring public bathing, or extensive foreign travel. On admission, her symptoms were G2VTM2 on the Glasgow Coma Scale, in an intubated state with 10 L of oxygen by mask. The patient exhibited tachycardia (heart rate, 110 beats/min), hypotension (blood pressure, 85/65mmHg) and decreased body temperature (35.7?), with a respiratory rate of 24 breaths/min. Oxygen saturation (SpO2) was not measured for peripheral coldness. On auscultation, breath sounds were diminished in the right embryonate. An infiltrative shadow with air bronchogram was apparent at the top right corner embryonate on chest X-ray at the previous hospitalization. Similarly, simple chest computed tomography revealed an infiltrative shadow on the right superior lobe. These findings were absent in the right lower lung field, left embryonate (Figure 1).
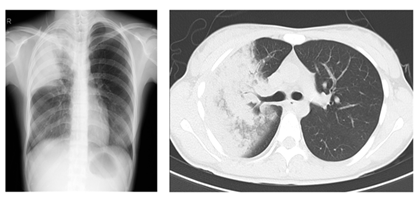
Figure 1: Pulmonary imaging. Chest X-ray revealing a consolidation shadow in the right apex area. Chest computed tomography revealing consolidation with air bronchogram shadow in the right superior lobe.
|
CBC/Coagulation |
Biochemistry |
Infection |
|||
|
WBC |
2.2x103/µl |
TP |
2.4 g/dL |
CRP |
11.45 mg/dL |
|
RBC |
3.85x106/µl |
Alb |
1.2 g/dL |
PCT |
0.5 ng/mL |
|
Hb |
11.7 g/dL |
LDH |
569 IU/L |
Urinary pneumococcus antigen (-) Urinary Legionella antigen (-) (Arterial blood gas Fi2 1.0 |
|
|
Hct |
36.4% |
y-TP |
5 IU/L |
||
|
Plt |
108x103/µl |
CK |
140 IU/L |
||
|
APTT |
120 s |
BUN |
35.8 /dL |
pH |
6.868 |
|
Fib |
50 mg/dL |
Cre |
1.69 mg/dL |
PCO2 |
130 mmol/L |
|
FDP |
1159.3 µg/dl |
UA |
4.8 mg/dL |
PO2 |
136.6 mmol/L |
|
D-dimer |
14.5 µg/dl |
Na |
144 mEq/L |
HCO3 |
23.11 mmol/L |
|
AT III |
22% |
K |
2.9 mEq/La |
Lac |
35.1 mg/dL |
Table 1: Laboratory findings
A blood count revealed a low white blood cell (220/µl) and platelet (108,000/ µl) counts. Coagulation tests revealed elevated levels of D dimer and fibrinogen/fibrin degradation products (14.5 and 1159.3 µg/dl, respectively), and ATIII was decreased (22%). Biochemical tests revealed renal dysfunction and hypoalbuminemia. High levels of C-reactive protein (11.45 mg/dl) were also observed. Examination for the urinary antigen of pneumococcus, Legionella, was negative. Partial pressure of carbon dioxide (PaCO2) was 130 torr and partial pressure of oxygen (PaO2) was 136.6 torr, hypoxemia with hypercapnia was found with artificial breathing on 100% oxygen (pH 6.868). Blood gas analysis revealed elevated lactate levels (Table 1).
Corticosteroids, vasopressors and sustained hemofiltration dialysis were initiated. Ventilatory volume decreased, and suction of fluids secreted from the airway, which were significant and frequent, was required. Due to progression of acidemia, extracorporeal membrane oxygenation (ECMO) was initiated. ABPC/SBT and levofloxacin were continued, and amikacin (AMK) was added because a large quantity of Gram-negative bacilli was confirmed on sputum gram-stain of secreted airway fluids. Additionally, endotoxin adsorption therapy was administered because blood endotoxin levels increased to 25 pg/ml. Nevertheless, the patient experienced sudden cardiac arrest 46 h after hospitalization. Cardiopulmonary resuscitation was performed immediately, and a heartbeat was rescued once; however, blood pressure could not be maintained, nor could heart rate after catecholamine administration. Death was confirmed 90 min after the first cardiac arrest. A pathological autopsy was performed. A sectioned surface of the lung is shown in Figure 2, with an invasive entity found in the right superior lobe. Evidence of pulmonary hemorrhage was also found. As the main lesion, macroscopic findings indicated that multiple organ failure was not found in the hemorrhagic pneumonia of both lungs.
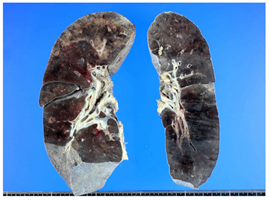
Figure 2: Pathological anatomy findings (macroscopic) from a sectioned surface of the lung. An invasive entity is apparent in the right superior lobe. General evidence of pulmonary hemorrhage is apparent.
Macroscopic imaging of the lung revealed that alveolar bleeding was the main evidence of hemorrhagic pneumonia with neutrophilic infiltration. Higher-power imaging suggested the presence of Pseudomonas aeruginosa supported by Gram-negative bacilli stained by periodic acid-Schiff staining (Figure 3). P. aeruginosa grew in all cultures of secretions from the right superior lobe, blood cultures of the airway, and the pathological anatomy. Septic shock due to pseudomonas pneumonia was diagnosed.
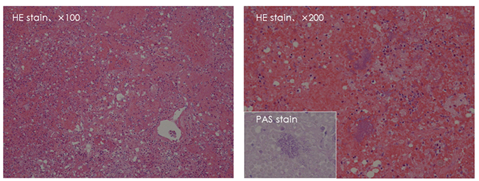
Figure 3: Pathological anatomy findings (microscopic). A low-power image of the lung. Alveolar bleeding was supportive evidence suggesting hemorrhagic pneumonia with neutrophilic infiltration. With a higher-power imaging, Pseudomonas aeruginosa was suspected based on gram-negative bacilli on periodic acid-Schiff staining.
2. Discussion
Pneumonias that occur in community settings usually have little or no direct connection with hospitals. As such, so-called “community-acquired pneumonia” is significantly different from pneumonia due to nosocomial infections, and depend on the type of pathogen and the identification, differential diagnosis, and many points such as the timing of treatment and intervention(s). There are predominant pneumococci causing community-acquired pneumonia, and, among the primary causative organism(s), atypical pneumonia, including Hemophilus influenzae and mycoplasma, are also common [1-4]. In contrast to hospital-acquired pneumonia, even in the case of elderly individuals, P. aeruginosa is not usually included in the differential diagnosis of community-acquired pneumonia [3]. Takayanagi et al. reported the frequency of community-acquired pneumonia due to P. aeruginosa in Japan to be 6.3% [5].
Pneumonia caused by P. aeruginosa is a predominantly nosocomial infection [3], and is extremely rare and does not often occur without underlying disease and risk factor(s) such as those exhibited by the patient described in the present report [3, 6]. Similar to Legionella, the use of a humidifier and/or foaming bathtubs are known to cause P. aeruginosa pneumonia; however, few such cases have been reported [3, 6]. In community-acquired pneumonia, P. aeruginosa is not usually considered as a primary causative organism of community-acquired pneumonia. More often, primary causative pneumococcus organisms, such as H. influenzae, or primary causative organisms of atypical pneumonia, such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella are suspected [1-4]. It is extremely difficult to predict the bacterial origin of pneumonia as P. aeruginosa before culture results are confirmed, unless pneumonia due to Gram-negative bacilli from gram staining of sputum is strongly suspected.
Pneumonias caused by nosocomial infection(s) and underlying respiratory disease are usually sudden. Despite the rarity of pseudomonal community-acquired pneumonias without respiratory underlying disease, many die from a fulminant course similar to this case [7, 8]. Henderson et al. [7], reported two cases of P. aeruginosa pneumonia without underlying disease, but who already exhibited shock and significant hypoxemia, similar to our case, at the hospital visit, and died within several hours after hospitalization. P. aeruginosa was not suspected in these cases, but became clear after culture results and death, similar to the case described in the present report. One patient was a 52-year-old man, in whom Legionella was suspected as the primary causative organism. He died 1 h after hospitalization without responding to treatment. On autopsy, air vesicles were full of bloody decoction, and bleeding was found in both adrenal glands. Friedlander's bacillus was the suspected primary causative organism in other case, a 27-year-old woman, who died 10 h after hospitalization without responding to vasopressor and oxygenation. On autopsy, air vesicles were full of bloody decoction. The disease course in both individuals was extremely violent, and both died despite gentamicin susceptibility. The prognosis of the Pseudomonas aeruginosa community-acquired pneumonia is extremely poor. Rello et al. examined 204 cases of community-acquired pneumonia of the severe form that required an intensive care, eight case of those are pseudomonas pneumonia and reported that seven of eight case died [8].
3. Conclusion
In this case, the patient was complicated by disseminated intravascular coagulation, septic shock and acute respiratory distress syndrome, and was suddenly aggravated. Despite combined multi-modality therapy, the patient died on the fourth day of illness. There was no consultation with the medical institution, and underlying disease associated with smoking history in youth was not found. Additionally, the P. aeruginosa species detected had good chemical sensitivity to systemic carbapenem and quinolone, with no results indicating resistance. It is not apparent why P. aeruginosa pneumonia without underlying disease exhibits a violent course. Both patients described by Henderson et al. died < 36 h from onset and, even if diagnosis is difficult, the violent course cannot be explained solely by a delay in treatment. Because case 1 described by Henderson et al. exhibited bleeding in both adrenal glands, Waterhouse-Friderichsen syndrome should have been considered [9] due to similar meningococcal pathology. However, bilateral adrenal hemorrhage is not necessarily caused by P. aeruginosa pneumonia all cases. Evidence of adrenal hemorrhage was not found at autopsy in the present case.
P. aeruginosa is a bacterial species not commonly assumed to be the cause of community-acquired pneumonia; however, it should be considered in cases of severe pneumonia with rapid exacerbation, for which it is necessary to start a broad-spectrum antimicrobial agent at an early stage.
References
- Makoto Aoki. Lower respiratory infectious disease (pneumonia). Infection practice manual for residents, medical study, Tokyo (2000): 211-224.
- Japanese Respiratory Society community-acquired pneumonia practice guidelines making Committee: A basic way of thinking of the adult community-acquired pneumonia practice. Japanese Respiratory Society (2000).
- Shigeru Kawano, Kazunori Asano. Change of respiratory infection that we examined from the respiratory infection primary causative organism of elderly people. Japanese Internal Medicine Society Magazine 87 (1998): 210-216.
- Chikara Nakahama. The management in the outpatient department of the community-acquired pneumonia – Importance of the initial diagnosis differential diagnosis to see in the current situation. Medical ASAHI (2003): 12-14.
- Takayanagi N, Taido H, Tokunaga Y, et al. A causative agent and prognosis according to the severity according to the age of the community-acquired pneumonia hospitalization case. The Japanese Respiratory Society Magazine 44 (2006): 906-915.
- Rello J, Rodriguez R, Jubert P, et al. Severe community-acquired pneumonia in the elderly: epidemiology and prognosis. Study Group for Severe Community-Acquired Pneumonia. Clin Infect Dis 23 (1996): 723-728.
- Henderson A, Kelly W, Wright M. Fulminant primary Pseudomonas aeruginosa pneumonia and septicaemia in previously well adults. Intensive Care Med 18 (1992): 430-432.
- Rello J, Bodi M, Mariscal D, et al. Microbiological testing and outcome of patients with severe community-acquired pneumonia. Chest 123 (2003): 174-180.
- Hamilton D, Harris MD, Foweraker J, et al. Waterhouse-Friderichsen syndrome as a result of non-meningococcal infection. J Clin Pathol 57 (2004): 208-209.
